Podcast
Questions and Answers
What is the primary function of the pulmonary circulation?
What is the primary function of the pulmonary circulation?
- To transport lymphocytes and leukocytes
- To move oxygenated blood to body tissues
- To return fluids from the interstitium to the circulatory system
- To deliver blood to the lungs for oxygenation (correct)
Which part of the heart has the thicker myocardial layer?
Which part of the heart has the thicker myocardial layer?
- The right ventricle
- The left atrium
- The left ventricle (correct)
- The right atrium
How does unoxygenated blood flow through the heart?
How does unoxygenated blood flow through the heart?
- From the left atrium to the right atrium
- From the left ventricle to the lungs
- From the right atrium to the right ventricle via the tricuspid valve (correct)
- From the right atrium to the aorta
What separates the right and left sides of the heart?
What separates the right and left sides of the heart?
Where does oxygenated blood enter the heart after it leaves the lungs?
Where does oxygenated blood enter the heart after it leaves the lungs?
Which structure contains the heart and is a double-walled sac?
Which structure contains the heart and is a double-walled sac?
What is the primary role of the SA node in the heart?
What is the primary role of the SA node in the heart?
Which structure receives the cardiac action potential directly from the SA node?
Which structure receives the cardiac action potential directly from the SA node?
What is the primary purpose of the lymphatic system?
What is the primary purpose of the lymphatic system?
How does the refractory period affect cardiac function?
How does the refractory period affect cardiac function?
Which chamber of the heart receives blood from the systemic circulation?
Which chamber of the heart receives blood from the systemic circulation?
Which of the following factors directly affects contractility in the heart?
Which of the following factors directly affects contractility in the heart?
What distinguishes myocardial cells from skeletal muscle cells?
What distinguishes myocardial cells from skeletal muscle cells?
Which adrenergic receptors are primarily responsible for the constriction of coronary arteries?
Which adrenergic receptors are primarily responsible for the constriction of coronary arteries?
What occurs due to troponin's interaction with calcium during muscle contraction?
What occurs due to troponin's interaction with calcium during muscle contraction?
What directly increases preload in the cardiac cycle?
What directly increases preload in the cardiac cycle?
What is the function of the atrioventricular valves in the heart?
What is the function of the atrioventricular valves in the heart?
Which phase of the cardiac cycle is characterized by the contraction of the myocardium?
Which phase of the cardiac cycle is characterized by the contraction of the myocardium?
What initiates the electrical impulses that stimulate the heart's contractions?
What initiates the electrical impulses that stimulate the heart's contractions?
Which statement correctly describes the role of the autonomic nervous system concerning the heart?
Which statement correctly describes the role of the autonomic nervous system concerning the heart?
What results from the depolarization of the entire ventricular myocardium during an ECG?
What results from the depolarization of the entire ventricular myocardium during an ECG?
What are collateral arteries important for?
What are collateral arteries important for?
What is the normal range for cardiac action potentials generated by the SA node?
What is the normal range for cardiac action potentials generated by the SA node?
What process is involved in the formation of new collateral vessels in the heart?
What process is involved in the formation of new collateral vessels in the heart?
How does Laplace's law relate to the generation of contractile force within a chamber?
How does Laplace's law relate to the generation of contractile force within a chamber?
What primarily assists blood flow through the veins?
What primarily assists blood flow through the veins?
What is true about the tunica media in arteries closest to the heart?
What is true about the tunica media in arteries closest to the heart?
What roles do precapillary sphincters play in blood flow?
What roles do precapillary sphincters play in blood flow?
What is the role of the endothelium in relation to vasomotion?
What is the role of the endothelium in relation to vasomotion?
How do vessel walls differ within the circulatory system?
How do vessel walls differ within the circulatory system?
What factors affect blood flow within the circulatory system?
What factors affect blood flow within the circulatory system?
What factors primarily contribute to resistance to blood flow in a vessel?
What factors primarily contribute to resistance to blood flow in a vessel?
Where does blood flow from after it leaves the capillaries?
Where does blood flow from after it leaves the capillaries?
How does total peripheral resistance change when blood vessels are arranged in series compared to parallel?
How does total peripheral resistance change when blood vessels are arranged in series compared to parallel?
Which of the following hormones primarily cause vasodilation?
Which of the following hormones primarily cause vasodilation?
During which phase of the cardiac cycle does blood flow into the coronary arteries occur?
During which phase of the cardiac cycle does blood flow into the coronary arteries occur?
What is the role of myoglobin in heart muscle during the cardiac cycle?
What is the role of myoglobin in heart muscle during the cardiac cycle?
Which factor does NOT influence arterial blood pressure?
Which factor does NOT influence arterial blood pressure?
What primarily influences venous pressure?
What primarily influences venous pressure?
What condition promotes optimal perfusion pressure in coronary vessels despite systolic effects?
What condition promotes optimal perfusion pressure in coronary vessels despite systolic effects?
What is the primary function of lymph nodes in the lymphatic system?
What is the primary function of lymph nodes in the lymphatic system?
What does cardiac catheterization primarily measure?
What does cardiac catheterization primarily measure?
Which test is particularly useful for detecting disturbances of impulse generation in cardiac disorders?
Which test is particularly useful for detecting disturbances of impulse generation in cardiac disorders?
How can the sensitivity of stress testing for cardiovascular disease be improved?
How can the sensitivity of stress testing for cardiovascular disease be improved?
What cardiovascular condition is most prevalent in older adults?
What cardiovascular condition is most prevalent in older adults?
What procedure allows for the visualization of the coronary circulation?
What procedure allows for the visualization of the coronary circulation?
Which evaluation technique can be used to assess systemic vascular health?
Which evaluation technique can be used to assess systemic vascular health?
Why is age considered a significant factor in cardiovascular risk?
Why is age considered a significant factor in cardiovascular risk?
Flashcards
Pulmonary Circulation
Pulmonary Circulation
The low-pressure circulation that delivers blood to the lungs for oxygenation. It's driven by the right side of the heart.
Systemic Circulation
Systemic Circulation
The high-pressure circulation that carries oxygenated blood to the body's tissues and waste products to the lungs, kidneys, and liver. Driven by the left side of the heart.
Lymphatic System
Lymphatic System
A network of vessels that collect fluids from tissues and return them to the circulatory system. Also transports immune cells.
Heart Chambers
Heart Chambers
Signup and view all the flashcards
Heart Valves
Heart Valves
Signup and view all the flashcards
Myocardium
Myocardium
Signup and view all the flashcards
Pericardium
Pericardium
Signup and view all the flashcards
Blood Flow Through the Heart
Blood Flow Through the Heart
Signup and view all the flashcards
Atrioventricular Valves
Atrioventricular Valves
Signup and view all the flashcards
Semilunar Valves
Semilunar Valves
Signup and view all the flashcards
Cardiac Cycle
Cardiac Cycle
Signup and view all the flashcards
Diastole
Diastole
Signup and view all the flashcards
Systole
Systole
Signup and view all the flashcards
SA Node
SA Node
Signup and view all the flashcards
ECG (Electrocardiogram)
ECG (Electrocardiogram)
Signup and view all the flashcards
Collateral Arteries
Collateral Arteries
Signup and view all the flashcards
SA Node Pacemaker
SA Node Pacemaker
Signup and view all the flashcards
AV Node Backup
AV Node Backup
Signup and view all the flashcards
Cardiac Conduction Pathway
Cardiac Conduction Pathway
Signup and view all the flashcards
Refractory Period
Refractory Period
Signup and view all the flashcards
Autonomic Heart Regulation
Autonomic Heart Regulation
Signup and view all the flashcards
Myocardial Cell Differences
Myocardial Cell Differences
Signup and view all the flashcards
Actin-Myosin Interaction
Actin-Myosin Interaction
Signup and view all the flashcards
Cardiac Performance Factors
Cardiac Performance Factors
Signup and view all the flashcards
Laplace's Law
Laplace's Law
Signup and view all the flashcards
Capillary Function
Capillary Function
Signup and view all the flashcards
Venules: Smallest Veins
Venules: Smallest Veins
Signup and view all the flashcards
Artery Wall Layers
Artery Wall Layers
Signup and view all the flashcards
Precapillary Sphincters
Precapillary Sphincters
Signup and view all the flashcards
Vein Blood Flow
Vein Blood Flow
Signup and view all the flashcards
Factors Affecting Blood Flow
Factors Affecting Blood Flow
Signup and view all the flashcards
What is lymph?
What is lymph?
Signup and view all the flashcards
Where does lymph travel?
Where does lymph travel?
Signup and view all the flashcards
What is the function of lymph nodes?
What is the function of lymph nodes?
Signup and view all the flashcards
What does a Holter monitor do?
What does a Holter monitor do?
Signup and view all the flashcards
What is a stress test?
What is a stress test?
Signup and view all the flashcards
What is cardiac catheterization used for?
What is cardiac catheterization used for?
Signup and view all the flashcards
What is the most common cardiovascular disease in older adults?
What is the most common cardiovascular disease in older adults?
Signup and view all the flashcards
What is the relationship between age and cardiovascular risk?
What is the relationship between age and cardiovascular risk?
Signup and view all the flashcards
Poiseuille's Law
Poiseuille's Law
Signup and view all the flashcards
Resistance to Blood Flow
Resistance to Blood Flow
Signup and view all the flashcards
Total Peripheral Resistance (TPR)
Total Peripheral Resistance (TPR)
Signup and view all the flashcards
Neural Regulation of Blood Flow
Neural Regulation of Blood Flow
Signup and view all the flashcards
Arterial Blood Pressure
Arterial Blood Pressure
Signup and view all the flashcards
Hormonal Regulation of Vasomotion
Hormonal Regulation of Vasomotion
Signup and view all the flashcards
Venous Pressure
Venous Pressure
Signup and view all the flashcards
Coronary Blood Flow: Diastolic Flow
Coronary Blood Flow: Diastolic Flow
Signup and view all the flashcards
Study Notes
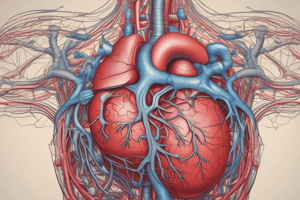
Pulmonary Circulation
- Driven by the right side of the heart
- Delivers blood to the lungs for oxygenation
- Low-pressure system
Systemic Circulation
- Driven by the left side of the heart
- Moves oxygenated blood to body tissues
- Delivers waste products to lungs, kidneys, and liver
- Higher pressure system
Lymphatic System
- Collects fluids from the interstitium
- Returns fluids to the circulatory system
- Transports lymphocytes and leukocytes
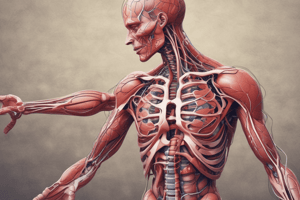
Heart Structure
- Four chambers (two atria, two ventricles)
- Four valves (two AV valves, two semilunar valves)
- Muscular wall (epicardium, myocardium, endocardium)
- Fibrous skeleton
- Conducting system
- Nerve fibers
- Coronary circulation
- Openings for great vessels
Heart Wall Layers
- Epicardium (outer layer)
- Myocardium (muscular layer)
- Endocardium (inner lining)
- Contained within a double-walled pericardium
Myocardium Thickness
- Atrial myocardium is thinner than ventricular myocardium
- Ventricular myocardium is thicker and stronger to generate pressure
- Separated by interatrial and interventricular septa
Blood Flow Through the Heart
- Unoxygenated blood enters right atrium from venae cavae
- Flows through right AV (tricuspid) valve to the right ventricle
- Passes through pulmonary semilunar valve to pulmonary artery
- Oxygenated blood enters the left atrium through pulmonary veins
- Flows through left AV (mitral) valve to left ventricle
- Passes through aortic semilunar valve to the aorta
- Delivers oxygenated blood to systemic arteries
Heart Valves
- Atrioventricular valves (AV valves): ensure one-way flow from atria to ventricles
- Semilunar valves: ensure one-way flow from ventricles to arteries (pulmonary artery and aorta)
Coronary Circulation
- Oxygenated blood enters coronary arteries from the aorta
- Deoxygenated blood exits through coronary veins into the right atrium (through coronary sinus)
Cardiac Cycle
- Diastole: Myocardium relaxes, chambers fill with blood
- Systole: Myocardium contracts, forces blood out of ventricles
- One cardiac cycle = one heartbeat
Conduction System
- Sinoatrial (SA) node: Generates electrical impulses
- Conduction system: Transmits impulses to stimulate contraction
- Autonomic nerves (sympathetic/parasympathetic) adjust heart rate/force, but do not initiate heartbeat
Cardiac Action Potentials
- SA node generates rhythmic impulses (60-100 bpm)
- Travel through conduction system
- Trigger myocardial contraction
- Atrial depolarization (P wave)
- Ventricular depolarization (QRS complex)
- Complete ventricular depolarization (ST interval)
Cardiac Conduction
- SA node is the natural pacemaker
- AV node assumes control if SA node fails
- Impulses travel through bundle of His, bundle branches, Purkinje fibers
- Refractory period prevents backward impulse transmission
Autonomic Regulation
- Adrenergic receptors (α, β) influence heart rate, contractile force, and coronary artery dilation/constriction
- Norepinephrine and epinephrine are involved
Myocardial Cells
- Intercalated discs enable faster action potential transmission
- Abundant mitochondria for ATP synthesis
- Ready access to ions facilitates continuous work
Muscle Contraction
- Cross-bridges between actin and myosin enable contraction
- Calcium interaction with troponin complex facilitates contraction/relaxation
Cardiac Performance
- Preload: Pressure in the ventricles at the end of diastole, dependent on blood volume
- Afterload: Resistance to blood ejection, depends on aortic pressure
- Contractility: Potential for myocardial fiber shortening during systole, determined by preload and stretch
Lymphatic System
- Lymph (interstitial fluid, immune cells) flows through lymphatic vessels
- Lymph nodes are sites of immune function
- Lymph flows into the right lymphatic duct and thoracic duct, which drain into the subclavian veins
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Explore the intricacies of the human circulatory system through this quiz. Learn about pulmonary and systemic circulation, the structure of the heart, and the lymphatic system. Dive into the functions and layers associated with the heart's anatomy.