Podcast
Questions and Answers
What is the primary function of the seminiferous tubules in the male reproductive system?
What is the primary function of the seminiferous tubules in the male reproductive system?
Which of the following cells is NOT found in the testis?
Which of the following cells is NOT found in the testis?
Which structure does the spermatozoa travel through after leaving the seminiferous tubules?
Which structure does the spermatozoa travel through after leaving the seminiferous tubules?
What type of tissue primarily surrounds the seminiferous tubules in the testis?
What type of tissue primarily surrounds the seminiferous tubules in the testis?
Signup and view all the answers
In which part of the male reproductive system are sperm matured and stored?
In which part of the male reproductive system are sperm matured and stored?
Signup and view all the answers
What is the first stage of spermatogenesis?
What is the first stage of spermatogenesis?
Signup and view all the answers
Which of the following describes Sertoli cells?
Which of the following describes Sertoli cells?
Signup and view all the answers
What is the role of Leydig cells in the male reproductive system?
What is the role of Leydig cells in the male reproductive system?
Signup and view all the answers
How long does it normally take for sperm to be formed in humans?
How long does it normally take for sperm to be formed in humans?
Signup and view all the answers
What characterizes the syncytium in the male germ cells?
What characterizes the syncytium in the male germ cells?
Signup and view all the answers
During spermiogenesis, what happens to the cytoplasm of the developing sperm?
During spermiogenesis, what happens to the cytoplasm of the developing sperm?
Signup and view all the answers
What type of epithelium is found in the seminiferous tubules?
What type of epithelium is found in the seminiferous tubules?
Signup and view all the answers
What is the primary function of anti-Müllerian hormone produced by Sertoli cells?
What is the primary function of anti-Müllerian hormone produced by Sertoli cells?
Signup and view all the answers
What is the role of GDNF in the testis?
What is the role of GDNF in the testis?
Signup and view all the answers
What triggers Leydig cells to produce androgens?
What triggers Leydig cells to produce androgens?
Signup and view all the answers
Which layer of the endometrium is not shed during menstruation?
Which layer of the endometrium is not shed during menstruation?
Signup and view all the answers
What is the primary hormone involved in the modifications of the endometrium during the menstrual cycle?
What is the primary hormone involved in the modifications of the endometrium during the menstrual cycle?
Signup and view all the answers
What characterizes the myometrium during pregnancy?
What characterizes the myometrium during pregnancy?
Signup and view all the answers
Which follicle stage is characterized by the presence of stratified granulosa cells?
Which follicle stage is characterized by the presence of stratified granulosa cells?
Signup and view all the answers
Which structure forms after the ovulation of a dominant follicle?
Which structure forms after the ovulation of a dominant follicle?
Signup and view all the answers
Which follicle stage takes approximately six months to become ready for ovulation?
Which follicle stage takes approximately six months to become ready for ovulation?
Signup and view all the answers
What is found in the ovarian medulla?
What is found in the ovarian medulla?
Signup and view all the answers
What happens to the corpus luteum if fertilization does not occur?
What happens to the corpus luteum if fertilization does not occur?
Signup and view all the answers
Which of the following is NOT a stage of follliculogenesis?
Which of the following is NOT a stage of follliculogenesis?
Signup and view all the answers
What is the functional significance of the zona pellucida?
What is the functional significance of the zona pellucida?
Signup and view all the answers
How many ovarian follicles are typically present in the two ovaries of a normal young woman?
How many ovarian follicles are typically present in the two ovaries of a normal young woman?
Signup and view all the answers
Which layer serves as the thick outer capsule of the ovary?
Which layer serves as the thick outer capsule of the ovary?
Signup and view all the answers
What is the role of the cumulus oophorus?
What is the role of the cumulus oophorus?
Signup and view all the answers
What is the primary purpose of the antrum of the secondary follicle?
What is the primary purpose of the antrum of the secondary follicle?
Signup and view all the answers
What indicates the potential presence of Polycystic Ovary Syndrome (PCOS)?
What indicates the potential presence of Polycystic Ovary Syndrome (PCOS)?
Signup and view all the answers
Which structure is associated with the degeneration of the corpus luteum?
Which structure is associated with the degeneration of the corpus luteum?
Signup and view all the answers
What effect does low levels of gonadotrophin have on the Graafian follicle?
What effect does low levels of gonadotrophin have on the Graafian follicle?
Signup and view all the answers
During which phase does the functionalis of the endometrium secrete substances?
During which phase does the functionalis of the endometrium secrete substances?
Signup and view all the answers
What is the primary composition of the zona pellucida in a secondary follicle?
What is the primary composition of the zona pellucida in a secondary follicle?
Signup and view all the answers
What role do peristaltic waves in the muscularis of the oviduct serve?
What role do peristaltic waves in the muscularis of the oviduct serve?
Signup and view all the answers
What is a characteristic of primary follicles?
What is a characteristic of primary follicles?
Signup and view all the answers
What is primarily formed by the aggregation of granulosa and thecal cells after ovulation?
What is primarily formed by the aggregation of granulosa and thecal cells after ovulation?
Signup and view all the answers
Which layer of the oviduct is responsible for nutrient secretion that aids in sperm activation?
Which layer of the oviduct is responsible for nutrient secretion that aids in sperm activation?
Signup and view all the answers
What occurs to the corpus luteum if fertilization does not happen?
What occurs to the corpus luteum if fertilization does not happen?
Signup and view all the answers
Which cell type serves as the primary source of testosterone in the testes?
Which cell type serves as the primary source of testosterone in the testes?
Signup and view all the answers
What is the function of ciliated cells in the oviduct?
What is the function of ciliated cells in the oviduct?
Signup and view all the answers
What are the characteristics of atretic follicles?
What are the characteristics of atretic follicles?
Signup and view all the answers
Which of the following describes the tunica albuginea?
Which of the following describes the tunica albuginea?
Signup and view all the answers
How does sperm travel through the vas deferens during ejaculation?
How does sperm travel through the vas deferens during ejaculation?
Signup and view all the answers
Which anatomical region is primarily involved in fertilization?
Which anatomical region is primarily involved in fertilization?
Signup and view all the answers
What is the role of sertoli cells?
What is the role of sertoli cells?
Signup and view all the answers
What can lead to an increased risk of ectopic pregnancy?
What can lead to an increased risk of ectopic pregnancy?
Signup and view all the answers
What does the term "communicating hydrocele" refer to?
What does the term "communicating hydrocele" refer to?
Signup and view all the answers
What is the primary histological feature of the seminiferous tubule epithelium?
What is the primary histological feature of the seminiferous tubule epithelium?
Signup and view all the answers
What is the primary role of the rete testis?
What is the primary role of the rete testis?
Signup and view all the answers
What type of epithelium lines the epididymis?
What type of epithelium lines the epididymis?
Signup and view all the answers
Which structure is responsible for sperm propulsion during ejaculation?
Which structure is responsible for sperm propulsion during ejaculation?
Signup and view all the answers
What type of glands are found in the prostate gland?
What type of glands are found in the prostate gland?
Signup and view all the answers
Which part of the endometrium is sloughed off during menstruation?
Which part of the endometrium is sloughed off during menstruation?
Signup and view all the answers
What is the primary function of the myometrium?
What is the primary function of the myometrium?
Signup and view all the answers
During which phase does the endometrium become thicker and more vascularized?
During which phase does the endometrium become thicker and more vascularized?
Signup and view all the answers
What structural characteristic differentiates secretory endometrium from proliferative endometrium?
What structural characteristic differentiates secretory endometrium from proliferative endometrium?
Signup and view all the answers
What major change occurs in the ovarian follicles post-ovulation?
What major change occurs in the ovarian follicles post-ovulation?
Signup and view all the answers
How are the glands in the secretory endometrium affected by hormonal support?
How are the glands in the secretory endometrium affected by hormonal support?
Signup and view all the answers
What type of fluid aids in the transport of the oocyte in the female reproductive tract?
What type of fluid aids in the transport of the oocyte in the female reproductive tract?
Signup and view all the answers
Which layer of the endometrium serves as the basis for regeneration after menstruation?
Which layer of the endometrium serves as the basis for regeneration after menstruation?
Signup and view all the answers
What type of muscle is predominant in the myometrium?
What type of muscle is predominant in the myometrium?
Signup and view all the answers
Study Notes
Seminiferous Tubules
- Complex structure responsible for sperm production
- Located in the testis, surrounded by connective tissue
- 500 tubules per testis, totaling 600 meters in length
- Lined by seminiferous epithelium: stratified epithelium with developing germ cells
- Spermatogonia (germ cells) undergo mitosis and meiosis within the tubules
- Move towards lumen starting from basal compartment
Sertoli Cells
- Found within seminiferous epithelium, supporting germ cell development.
- Have a distinct triangle-shaped nucleus
- Extend from the basal side to the apical side of the epithelium
- Create the blood-testis barrier with tight junctions, preventing immune attack on developing sperm.
- Produce luminal fluid to facilitate movement of the sperm towards the rete testis.
- Nurse cells of the testis, supporting spermatogenesis in response to FSH and testosterone
Leydig Cells
- In loose connective tissue called intertubular tissue
- Produce testosterone, which stimulates the accessory male reproductive organs
- Have rod-shaped crystals of Reinke within cytoplasm, function unknown.
- Respond to LH from the anterior pituitary gland.
Spermatogenesis
- Process of sperm formation, involving mitosis, meiosis, and spermiogenesis
- Takes about 70 days to complete
- 100 million sperm produced daily, with about 40 million ejaculated.
- Starts with spermatogonia and culminates in spermatozoa
- The syncytium occurs during spermatogenesis, where cytoplasmic bridges maintain connections between germ cells
- Spermiogenesis involves nuclear compaction, cytoplasm discarding, tail development, and acrosome formation.
- Different stages of spermatogenesis are visible in cross-sections of the seminiferous tubules.
Rete Testis
- Network of channels connecting seminiferous tubules to efferent ducts
- Allows sperm to transition from testes to accessory organs
Epididymis
- Head, body, and tail structures storing sperm for weeks
- Sperm gain initial motility in the epididymis
- Lined with pseudostratified columnar epithelium with stereocilia (long microvilli)
- Stereocilia are important for absorbing luminal fluid and providing surface area for sperm maturation.
Vas Deferens
- Thick-walled tube with three layers of smooth muscle, allowing for sperm propulsion
- Has epithelium similar to epididymis with stereocilia
- Can absorb sperm after a vasectomy
Prostate Gland
- Tubuloalveolar glands with a capsule forming lobules
- Secretes fluids containing zinc, citric acid, proteolytic enzymes, and prostaglandins.
- Secretory epithelium (cuboidal, columnar, pseudostratified)
- Has a similar appearance to the uterus but lacks endometrial glands.
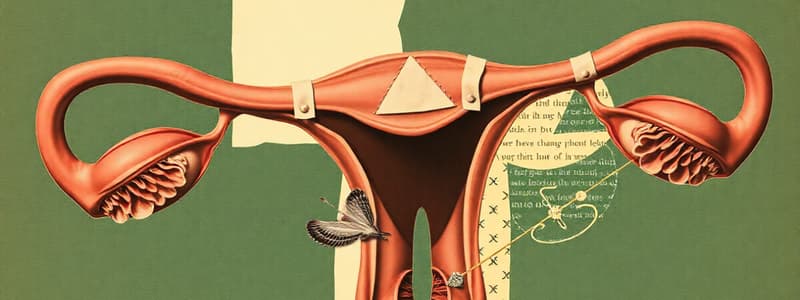
Ovary
- Almond-shaped organ responsible for oocyte production and release.
- Contains a cortex with follicles and a medulla with vascular tissue.
- Surface covered by germinal epithelium (simple squamous or cuboidal).
- Follicles contain oocytes at different stages of development.
- Folliculogenesis: primordial follicle to primary follicle, secondary follicle, antral follicle, Graafian follicle
- Antrum formation is associated with increasing estrogen production by follicular cells.
- Takes around 6 months for a primordial follicle to become a Graafian follicle.
Folliculogenesis Stages
- Primordial follicle: Simple squamous epithelium surrounding a small oocyte
- Primary follicle: Single layer of cuboidal granulosa cells surrounding the oocyte
- Secondary follicle: Stratified granulosa cells; zona pellucida is visible.
- Antral follicle: Development of a fluid-filled space called the antrum; cumulus oophorus forms around the oocyte.
- Graafian follicle: Mature follicle with large antrum; oocyte with corona radiata is ready for ovulation
Ovulation
- Rupture of the Graafian follicle and release of the oocyte
- Stimulated by LH surge
- Oocyte is drawn into the fallopian tube by follicular fluid.
Corpus luteum
- Structure formed from remaining follicle after ovulation
- Secretes progesterone and some estrogen.
- Degenerates into corpus albicans if fertilization does not occur.
Oviduct (Fallopian Tube)
- Tube connecting the ovary to the uterus
- Site of fertilization
- Lined with ciliated epithelium that helps propel the oocyte towards the uterus
- Has three layers: mucosa, lamina propria, muscularis
Uterus
- Pear-shaped, hollow organ
- Has three layers: endometrium, myometrium, and perimetrium
- Endometrium: The inner lining, responsible for implantation, has two layers: functionalis and basalis.
- Myometrium: Thick layer of smooth muscle, responsible for uterine contractions.
- Perimetrium: Serous membrane covering the uterus.
Endometrial Cycle
- Changes in the endometrium throughout the menstrual cycle
- Menstrual phase (days 1-4): Sloughing of the functionalis layer.
- Proliferative phase (days 5-14): Glands are straight and long, epithelium is pseudostratified columnar. Endometrium is stimulated by estrogen.
- Secretory phase (days 15-28): Glands coil and become sawtooth-shaped; endometrium is stimulated by progesterone.
Key Terms
- Atresia: Degeneration and resorption of ovarian follicles.
- Spermatogonia: Germ cells that give rise to sperm.
- Sertoli cells: Nurse cells of the testis, providing support for sperm development
- Leydig cells: Cells in the testis responsible for testosterone production.
- **Rete testis:**Network of channels within testis.
- Epididymis: Tubular structure where sperm mature and are stored.
- Vas deferens: Tube that carries sperm from the epididymis to the urethra.
- Prostate gland: Gland that produces fluids that contribute to semen.
- Ovarian follicle: Structure containing an oocyte and supporting cells.
- Corpus luteum: Structure formed after ovulation, responsible for progesterone production.
- Endometrium: Inner lining of the uterus, responsible for implantation.
- Myometrium: Smooth muscle layer of the uterus.
- Functionalis: Layer of the endometrium that sloughs off during menstruation.
- Basalis: Layer of the endometrium that regenerates the functionalis layer.
- Ovulation: Release of an oocyte from the ovary.
- Oviduct (fallopian tube): Tube that carries the oocyte from the ovary to the uterus.
- Capacitation: Process by which sperm become capable of fertilization.
Oviduct
- The oviduct is made up of 3 sections: the infundibulum, the ampulla (where fertilization occurs), and the isthmus.
- 50% of fimbrial cells have cilia, which aid in the propulsion of gametes and embryos alongside muscular contractions and tubal secretions.
- The muscularis layer of the oviduct is surrounded by a serosa covered by a simple squamous epithelium, allowing the oviduct to remain mobile within the pelvis.
- Obstruction in the lumen of the oviduct caused by salphingitis can lead to ectopic pregnancy.
Testes
- The testes are divided into 350-370 lobules by septa that radiate from the tunica albuginea and converge at the mediastinum.
- The tunica albuginea, a fibromuscular connective tissue capsule, surrounds the testes and has a high collagen content to protect the testes.
- Peritubular myoid cells, located around the seminiferous tubules and alongside Leydig cells, have a contractile nature and help to propel sperm into the rete testes.
- Leydig cells are the primary source of testosterone.
- The rete testes is a network of tubules connecting the seminiferous tubules and the ductus efferentes; tubular ectasia in this area presents as numerous benign cysts.
- Spermatozoa are released into the lumens of the seminiferous tubules after they differentiate from spermatids.
- The epididymis is lined by pseudostratified epithelium with long microvilli (immotile stereocilia) that allow for sperm storage and maturation, fluid reabsorption, and sperm phagocytosis after vasectomy.
- The epididymis is a common site of inflammation in males due to untreated gonorrhoea and chlamydia infections.
Vas Deferens
- The lumen of the vas deferens has a limited storage capacity and is made up of 3 layers of muscle surrounded by adventitia, which is made up of connective tissue.
- Peristaltic contractions help to propel sperm along the vas deferens during ejaculation.
Epididymis
- Pseudostratified columnar epithelium lines the epididymis allowing for fluid reabsorption and contributing to the maturation of sperm cells.
Prostate
- Contains the ejaculatory duct, which is formed by the union of the vas deferens and the duct of the seminal vesicle.
- The prostate is divided into 5 lobes by fibromuscular septa.
- Benign prostatic hyperplasia (BPH) commonly develops in the periurethral zone of the prostate, obstructing the flow of urine.
Hydrocele
- A hydrocele is an abnormal collection of serous fluid in the peritoneal space.
- It occurs when there is a communication (communicating) between the visceral and parietal compartments of the tunica vaginalis.
- Alternatively, the fluid may remain localized within the testes (non-communicating).
- A Valsalva manoeuvre can be used to determine the presence of a communicating hydrocele.
Ovary
- The ovary is a key female reproductive organ.
- The antrum of secondary follicles contains nutritive fluid for the oocyte.
- Increased antrum counts combined with irregular periods may indicate Polycystic ovary syndrome (PCOS).
- Ovulation occurs via the stigma, expelling the oocyte, zona pellucida, and follicular cells (corona radiata).
- The corpus luteum persists in the presence of human chorionic gonadotrophin.
- Poor estrogen production by the corpus luteum negatively affects embryo viability.
- The corpus albicans is made up of fibrous tissue remaining after corpus luteum degeneration.
- Sometimes the corpus albicans remains in the ovary, forming spots throughout the ovaries.
- The primary follicles contain a simple squamous epithelium lining the oocyte, while secondary follicles are lined by stratified squamous epithelium
- Atretic follicles are a normal outcome of reduced FSH exposure, leading to the formation of granuloza cells.
- Granulosa cells cannot distinguish the oocyte.
- The Graafian follicle is selected from a cohort of recruited follicles to become dominant and increase in size.
- The zona pellucida, surrounding the oocyte, can result in infertility if sperm binding is difficult.
Uterus
- The endometrium, lined by simple columnar epithelium, undergoes cyclical changes dictated by the menstrual cycle.
- In the proliferative phase the endometrium proliferates, in the secretory phase it secretes, and in the menstrual phase it sloughs off.
- During the secretory phase, the endometrial glands secrete glycogen rich mucus that is essential for embryo implantation.
- The muscularis of the oviduct has peristaltic waves that assist in the transport of the conceptus to the uterus.
Additional Terms
- Sertoli cells: Nurse cells of developing germ cells. They remain present in rare cases of infertility, while germ cells are absent (germ cell aplasia).
- Stigma: The point on the surface of the ovary where the oocyte is released during ovulation. Often described as a bulge on the ovary.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Description
Test your knowledge about the male reproductive system with this quiz. Questions cover the functions of seminiferous tubules, structures associated with sperm production, and the maturation of sperm. Ideal for students of human biology.