Podcast
Questions and Answers
How is flow through blood vessels primarily driven?
How is flow through blood vessels primarily driven?
- By the temperature of the fluid
- By the surface area of the vessel
- By the viscosity of the fluid
- By the gradient of pressure (correct)
Which statement accurately describes laminar flow?
Which statement accurately describes laminar flow?
- Fluid layers move in concentric layers with varying speeds (correct)
- Velocity is highest at the edges of the vessel
- Velocity is uniform across the vessel
- Flow resistance is minimized
What effect does an increase in vessel radius have on mean velocity at a constant flow?
What effect does an increase in vessel radius have on mean velocity at a constant flow?
- It increases mean velocity (correct)
- It does not affect mean velocity
- It inversely affects flow resistance
- It decreases mean velocity
Which factor influences the flow resistance in blood vessels?
Which factor influences the flow resistance in blood vessels?
What happens when blood flow becomes turbulent?
What happens when blood flow becomes turbulent?
How does viscosity affect the central layers of fluid in laminar flow?
How does viscosity affect the central layers of fluid in laminar flow?
In the context of blood flow, which best describes the relationship between mean velocity and surface area?
In the context of blood flow, which best describes the relationship between mean velocity and surface area?
What governs the flow for a given pressure gradient in blood vessels?
What governs the flow for a given pressure gradient in blood vessels?
What initiates the action potential in the heart muscle?
What initiates the action potential in the heart muscle?
Which structure acts as the primary pacemaker of the heart?
Which structure acts as the primary pacemaker of the heart?
During which phase of the cardiac cycle do the ventricles actively fill with blood?
During which phase of the cardiac cycle do the ventricles actively fill with blood?
What occurs as intraventricular pressure exceeds aortic pressure during ventricular systole?
What occurs as intraventricular pressure exceeds aortic pressure during ventricular systole?
Which sound is produced by the closure of the a/v valves during the cardiac cycle?
Which sound is produced by the closure of the a/v valves during the cardiac cycle?
What is the duration of ventricular systole during a typical heartbeat?
What is the duration of ventricular systole during a typical heartbeat?
What causes the closure of the a/v valves during ventricular systole?
What causes the closure of the a/v valves during ventricular systole?
In which phase are all heart valves closed and the volume of blood in the ventricles remains constant?
In which phase are all heart valves closed and the volume of blood in the ventricles remains constant?
Which type of valve prevents backflow from the aorta into the left ventricle?
Which type of valve prevents backflow from the aorta into the left ventricle?
What is the interval between the first heart sound and the second heart sound during a normal resting state?
What is the interval between the first heart sound and the second heart sound during a normal resting state?
What event occurs immediately after the closure of the outflow valves?
What event occurs immediately after the closure of the outflow valves?
What is the primary function of the pacemaker cells in the sinoatrial node?
What is the primary function of the pacemaker cells in the sinoatrial node?
What type of heart murmur is produced by narrowed blood flow through a valve?
What type of heart murmur is produced by narrowed blood flow through a valve?
How often does the sinoatrial node generate an action potential at rest?
How often does the sinoatrial node generate an action potential at rest?
What occurs to the arterial pressure if the heart pumps more blood while the resistance of arterioles remains constant?
What occurs to the arterial pressure if the heart pumps more blood while the resistance of arterioles remains constant?
How does the resistance in blood vessels change when the vessel expands due to increased pressure?
How does the resistance in blood vessels change when the vessel expands due to increased pressure?
In a situation where blood flows through a narrowed vessel, what effect is expected on the flow?
In a situation where blood flows through a narrowed vessel, what effect is expected on the flow?
What is the relationship between flow, resistance, and pressure when flow is constant?
What is the relationship between flow, resistance, and pressure when flow is constant?
Which statement accurately describes the behavior of blood in capillaries?
Which statement accurately describes the behavior of blood in capillaries?
How does viscosity of blood influence the difficulty of blood flow through vessels?
How does viscosity of blood influence the difficulty of blood flow through vessels?
What happens to the effective resistance when blood vessels are connected in parallel?
What happens to the effective resistance when blood vessels are connected in parallel?
In the context of blood flow and resistance in the cardiovascular system, which factor primarily leads to a greater pressure drop?
In the context of blood flow and resistance in the cardiovascular system, which factor primarily leads to a greater pressure drop?
What is the primary characteristic of veins in relation to resistance within the circulation?
What is the primary characteristic of veins in relation to resistance within the circulation?
When considering the impact of vessel diameter on blood flow, which statement is true?
When considering the impact of vessel diameter on blood flow, which statement is true?
Flashcards are hidden until you start studying
Study Notes
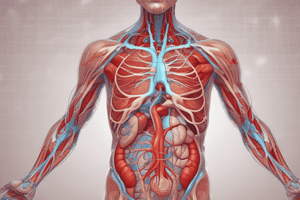
### The Heart
- The heart consists of two pumps working in series: the right and left sides of the heart.
- Each side of the heart consists of two chambers: a thin-walled atrium and a muscular ventricle.
- Blood flows into and out of the ventricles through valves: atrioventricular valves (mitral and tricuspid) and outflow valves (aortic and pulmonary).
Heart Muscle
- Heart muscle is a specialized form of muscle tissue with discrete cells connected electrically.
- When an action potential reaches the membrane of a heart cell, it causes a contraction.
- The action potential causes an influx of intracellular calcium, which leads to a prolonged contraction.
- A single heart contraction (systole) lasts approximately 280 milliseconds.
- Excitation spreads from cell to cell in the heart muscle, triggering a coordinated contraction.
Pacemakers
- Pacemakers are specialized groups of cells that generate action potentials, which then spread throughout the heart.
- These action potentials cause coordinated contractions.
- Pacemakers generate one action potential at regular intervals, creating the rhythmic heartbeat.
Phases of the Cardiac Cycle
- Each action potential in the heart generates one heartbeat, consisting of systole (contraction) and diastole (relaxation).
Spread of Excitation - 1
- The pacemaker of the heart is located in the sino-atrial (SA) node, located in the right atrium.
- Excitation spreads throughout the atria, causing atrial systole.
- This excitation then reaches the atrioventricular (AV) node, where it is delayed for approximately 120 milliseconds.
Spread of Excitation - 2
- From the AV node, the excitation spreads down the septum between the ventricles.
- From the septum, it spreads through the ventricular myocardium from the inner (endocardial) to the outer (epicardial) surface.
- This coordinated spread of excitation leads to the ventricle contracting from the apex upwards, propelling blood towards the outflow valves.
The Cardiac Cycle Overview
- At rest, the SA node generates an action potential approximately once per second.
- This leads to a short atrial systole followed by a longer ventricular systole.
- Ventricular systole lasts about 280 milliseconds, followed by relaxation lasting about 700 milliseconds before the next systole.
The Left Ventricle
- The inflow valve of the left ventricle is the mitral valve, which allows blood to flow from the atrium to the ventricle but not vice versa.
- The mitral valve opens when atrial pressure exceeds ventricular pressure and closes when ventricular pressure exceeds atrial pressure.
The Left Ventricle (cont.)
- The outflow valve of the left ventricle is the aortic valve, allowing blood to flow from the ventricle to the aorta but not vice versa.
- The aortic valve opens when ventricular pressure exceeds aortic pressure and closes when aortic pressure exceeds ventricular pressure.
The Cardiac Cycle - 1
- The cardiac cycle starts towards the end of ventricular systole.
- At this point, the ventricles are contracted, and intraventricular pressure is high.
- The outflow valves are open, and blood is flowing into the arteries.
- Ventricular pressure exceeds atrial pressure, keeping the AV valves closed.
The Cardiac Cycle - 2
- As the ventricles begin to relax, intraventricular pressure falls, becoming less than arterial pressure.
- This causes a brief backflow of blood, closing the outflow valves.
- All valves are now closed, and the period of isovolumetric relaxation begins.
The Cardiac Cycle - 3
- During systole, blood has continued to return to the atria.
- This leads to relatively high atrial pressure.
- As intraventricular pressure continues to fall, it eventually becomes less than atrial pressure.
- As a result, the AV valves open.
The Cardiac Cycle - 4
- With the AV valves open, the ventricles begin to fill rapidly, known as the 'rapid filling phase'.
- This phase lasts approximately 200 to 300 milliseconds and accounts for the majority of ventricular filling.
The Cardiac Cycle - 5
- As diastole continues, the ventricles fill more slowly.
- Intraventricular pressure rises slightly as ventricular walls stretch.
- Filling continues until intraventricular pressure matches atrial pressure, at which point filling stops.
The Cardiac Cycle - 6
- Atrial systole occurs, forcing a small additional volume of blood into the ventricles.
- However, the heart can pump perfectly well without atrial systole.
The Cardiac Cycle - 7
- Ventricular systole begins, causing intraventricular pressure to rise rapidly.
- Intraventricular pressure quickly exceeds atrial pressure, leading to a brief backflow, and the AV valves close.
- All valves are closed again, and the period of isovolumetric contraction begins.
The Cardiac Cycle - 8
- Intraventricular pressure continues to rise rapidly, exceeding arterial pressure, which has been falling during diastole.
- As a result, the outflow valves open.
The Cardiac Cycle - 9
- With the outflow valves open, blood is ejected rapidly into the arteries, known as the rapid ejection phase.
- Arterial pressure rises rapidly.
The Cardiac Cycle - 10
- As arterial pressure rises, the rate of ejection falls.
- Both arterial and intraventricular pressure peak towards the end of systole.
- Eventually, the ejection of blood ceases despite blood remaining in the ventricle.
The Cardiac Cycle - 11
- Systole ends and the cycle repeats from step 1.
Heart Sounds
- The heart produces two main sounds due to the closing of valves.
- The first sound, 'lup', is caused by the closure of the AV valves.
- The second sound, 'dup', is caused by the closure of the outflow valves.
Heart Sounds (cont.)
- The first sound occurs at the onset of ventricular systole.
- The second sound occurs at the end of ventricular systole.
- At rest, the interval between the first and second sound is approximately 280 milliseconds.
- The interval from the second sound to the next first sound is approximately 700 milliseconds.
Heart Murmurs
- Turbulent blood flow generates murmurs, which can indicate abnormalities in the heart valves.
- A narrowed valve (stenosis) or a valve that doesn't close properly (incompetence) can both lead to turbulent flow.
- Murmurs occur when blood flow is highest, so their timing within the cardiac cycle can help diagnose the underlying valve problem.
Heart Murmurs (cont.)
- For example, an aortic stenosis produces a murmur during the rapid ejection phase.
Cardiac Output
- With each beat, the heart ejects a stroke volume of blood.
- Cardiac output is the volume of blood pumped by the heart per minute and is calculated as stroke volume multiplied by heart rate.
- At rest, cardiac output is approximately 5 liters per minute (80 ml stroke volume x 60 beats per minute).
Cardiovascular System - Flow, Resistance, and Pressure
- Flow is proportional to the pressure difference, meaning a greater pressure difference results in a greater flow.
- Resistance is determined by the properties of the fluid and the vessel.
- Flow resistance is the opposition to flow.
- Viscosity is the property of a fluid that resists flow.
- Flow is inversely proportional to viscosity.
- The wider the tube, the faster the flow (inversely proportional to the cross-sectional area).
Series and Parallel Resistance
- The effective resistance of vessels connected in series is the sum of the individual resistances (like electrical resistors in series).
- The effective resistance of vessels connected in parallel is lower than the individual resistances (like electrical resistors in parallel).
Pressure, Flow, and Resistance
- At a constant flow, higher resistance leads to greater changes in pressure from one end of the vessel to the other.
- At a constant pressure, higher resistance leads to lower flow.
The Whole Circulation
- Flow is the same at all points in the circulation.
- Arteries have low resistance, so the pressure drop across arteries is small.
- Arterioles have high resistance, so the pressure drop across arterioles is significant.
- While individual capillaries also have high resistance, there are many connected in parallel, reducing the overall resistance.
- Venules and veins have low resistance, so the pressure drop across these vessels is also low.
The Whole Circulation (cont.)
- Because of the high arteriolar resistance, arterial pressure is high.
- For a given total flow, higher arteriolar resistance leads to higher arterial pressure.
The Whole Circulation (cont.)
- If the heart pumps more blood with constant arteriolar resistance, arterial pressure will rise.
Special Problems of Flow in Blood Vessels - 1
- In some vessels like the aorta, flow can become turbulent, increasing resistance.
- Turbulent flow can also occur in narrowed vessels, such as those affected by atherosclerosis.
- Turbulent flow generates sound.
Special Problems of Flow in Blood Vessels - 2
- Blood vessels have distensible walls.
- Pressure inside a vessel generates a 'transmural pressure' between the inside and outside, stretching the vessel.
Distensible Vessels
- As vessels stretch, their resistance falls.
- Therefore, the higher the pressure in a vessel, the easier it is for blood to flow through it.
- Distensible vessels store blood, also known as 'capacitance'.
- Veins are the most distensible vessels in the circulatory system.
Funny Things About Blood
- Blood cells tend to congregate in the middle of flowing blood streams, increasing the apparent viscosity.
- This causes red blood cells to travel faster than plasma.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.