Podcast
Questions and Answers
What role does the hypothalamic–pituitary–gonadal (HPG) axis primarily play in the body?
What role does the hypothalamic–pituitary–gonadal (HPG) axis primarily play in the body?
- Regulating metabolic rates
- Stimulating appetite
- Regulating reproduction and fertility (correct)
- Controlling body temperature
What triggers the secretion of luteinizing hormone (LH) and follicle-stimulating hormone (FSH)?
What triggers the secretion of luteinizing hormone (LH) and follicle-stimulating hormone (FSH)?
- Estrogen release
- Testosterone activation
- Growth hormone stimulation
- Gonadotropin-releasing hormone (GnRH) (correct)
How is GnRH released in the body?
How is GnRH released in the body?
- In a pulsatile fashion (correct)
- Continuously at a constant rate
- Only during sleep
- In response to stress
What happens to GnRH shortly after it is released?
What happens to GnRH shortly after it is released?
What is the function of gonadotropins in males and females?
What is the function of gonadotropins in males and females?
What hormone primarily regulates testosterone secretion from the testes?
What hormone primarily regulates testosterone secretion from the testes?
During which life stage does testosterone secretion experience a perinatal surge?
During which life stage does testosterone secretion experience a perinatal surge?
What is the primary consequence of the increases in testosterone levels during male puberty?
What is the primary consequence of the increases in testosterone levels during male puberty?
What portion of circulating testosterone is bound to sex hormone-binding globulin (SHBG)?
What portion of circulating testosterone is bound to sex hormone-binding globulin (SHBG)?
What happens to circulating testosterone levels after middle age?
What happens to circulating testosterone levels after middle age?
What is the role of the androgen-AR complex once it binds to hormone response elements on DNA?
What is the role of the androgen-AR complex once it binds to hormone response elements on DNA?
Which effect does testosterone NOT have on the skeletal system?
Which effect does testosterone NOT have on the skeletal system?
Which of the following describes how androgens impact the nervous system?
Which of the following describes how androgens impact the nervous system?
What mechanism occurs when either testosterone or DHT binds to androgen receptors?
What mechanism occurs when either testosterone or DHT binds to androgen receptors?
How do androgens generally affect the body's immunological response?
How do androgens generally affect the body's immunological response?
Which of the following is NOT a symptom of hypogonadism in adult men?
Which of the following is NOT a symptom of hypogonadism in adult men?
What is Klinefelter's Syndrome primarily associated with?
What is Klinefelter's Syndrome primarily associated with?
Which condition results from iron overload affecting testosterone production?
Which condition results from iron overload affecting testosterone production?
Which option is a DIRECT cause of primary hypogonadism?
Which option is a DIRECT cause of primary hypogonadism?
What is a known effect of aging on testosterone levels in men?
What is a known effect of aging on testosterone levels in men?
Which of the following hormones are affected by Kallmann Syndrome?
Which of the following hormones are affected by Kallmann Syndrome?
Which of the following symptoms is associated with testosterone deficiency?
Which of the following symptoms is associated with testosterone deficiency?
What can result from the treatment of cancer with chemotherapy?
What can result from the treatment of cancer with chemotherapy?
What are the sex steroids synthesized and secreted in females and males?
What are the sex steroids synthesized and secreted in females and males?
Which hormone is crucial for the proliferation of Sertoli cells during early puberty in boys?
Which hormone is crucial for the proliferation of Sertoli cells during early puberty in boys?
What is the primary function of the luteinizing hormone (LH) in males?
What is the primary function of the luteinizing hormone (LH) in males?
Which of the following accurately describes the action of FSH in the male reproductive system?
Which of the following accurately describes the action of FSH in the male reproductive system?
What effect does negative feedback from sex steroids have in the body?
What effect does negative feedback from sex steroids have in the body?
Which protein is crucial for the action of steroid hormones in Sertoli cells?
Which protein is crucial for the action of steroid hormones in Sertoli cells?
How do Leydig cells respond to an increase in luteinizing hormone (LH)?
How do Leydig cells respond to an increase in luteinizing hormone (LH)?
What is the role of P-450 aromatase in the male reproductive system?
What is the role of P-450 aromatase in the male reproductive system?
Flashcards
Androgens
Androgens
Testosterone and dihydrotestosterone (DHT) are the primary male sex hormones called androgens, responsible for male characteristics.
LH's role in testosterone production
LH's role in testosterone production
LH (luteinizing hormone) controls the production of testosterone by stimulating the conversion of cholesterol to pregnenolone in Leydig cells within the testes.
Testosterone transport
Testosterone transport
Most testosterone in the bloodstream is bound to proteins, primarily Sex Hormone-Binding Globulin (SHBG) and albumin, with only a small amount circulating freely.
Testosterone and puberty
Testosterone and puberty
Signup and view all the flashcards
Inhibins
Inhibins
Signup and view all the flashcards
What is the HPG axis?
What is the HPG axis?
Signup and view all the flashcards
Where is GnRH produced and what does it do?
Where is GnRH produced and what does it do?
Signup and view all the flashcards
How does GnRH signal to the pituitary gland?
How does GnRH signal to the pituitary gland?
Signup and view all the flashcards
What are FSH and LH, and what do they do?
What are FSH and LH, and what do they do?
Signup and view all the flashcards
How do FSH and LH act on the gonads?
How do FSH and LH act on the gonads?
Signup and view all the flashcards
What is the mechanism of androgen action?
What is the mechanism of androgen action?
Signup and view all the flashcards
What is the role of the androgen receptor (AR)?
What is the role of the androgen receptor (AR)?
Signup and view all the flashcards
How does testosterone affect bone?
How does testosterone affect bone?
Signup and view all the flashcards
What is the effect of testosterone on the immune system?
What is the effect of testosterone on the immune system?
Signup and view all the flashcards
How does testosterone affect the nervous system?
How does testosterone affect the nervous system?
Signup and view all the flashcards
Hypogonadism
Hypogonadism
Signup and view all the flashcards
Primary Hypogonadism
Primary Hypogonadism
Signup and view all the flashcards
Secondary Hypogonadism
Secondary Hypogonadism
Signup and view all the flashcards
Klinefelter's Syndrome
Klinefelter's Syndrome
Signup and view all the flashcards
Mumps Orchitis
Mumps Orchitis
Signup and view all the flashcards
Hemochromatosis
Hemochromatosis
Signup and view all the flashcards
Kallmann Syndrome
Kallmann Syndrome
Signup and view all the flashcards
Pituitary Disorders
Pituitary Disorders
Signup and view all the flashcards
Gonadotropins
Gonadotropins
Signup and view all the flashcards
Sex steroids
Sex steroids
Signup and view all the flashcards
Negative feedback loop of sex steroids
Negative feedback loop of sex steroids
Signup and view all the flashcards
Luteinizing hormone (LH)
Luteinizing hormone (LH)
Signup and view all the flashcards
Follicle-stimulating hormone (FSH)
Follicle-stimulating hormone (FSH)
Signup and view all the flashcards
Leydig cells
Leydig cells
Signup and view all the flashcards
Sertoli cells
Sertoli cells
Signup and view all the flashcards
Spermatogenesis
Spermatogenesis
Signup and view all the flashcards
Study Notes
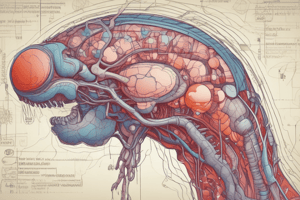
Hypothalamic-Pituitary-Gonadal (HPG) Axis
- The HPG axis is crucial for regulating reproduction, fertility, and the formation of gonadal sex steroids.
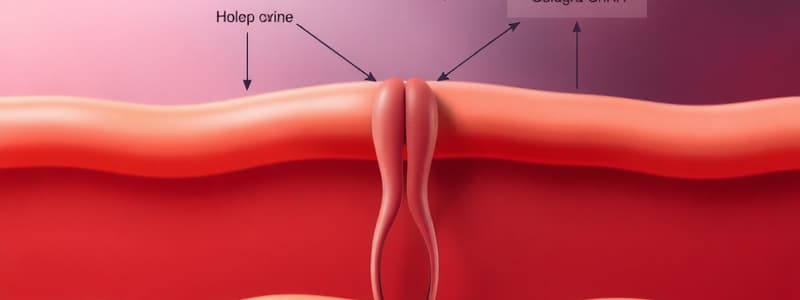
- Gonadotropin-releasing hormone (GnRH) is secreted from the hypothalamus' arcuate nucleus.
- The anterior pituitary gland produces luteinizing hormone (LH) and follicle-stimulating hormone (FSH).
- The gonads (testes and ovaries) produce estrogen and testosterone.
GnRH
- GnRH is a peptide hormone that activates gonadotrope cells.
- Its receptor is a G-protein-coupled receptor.
- GnRH stimulates phospholipase C, leading to calcium and protein kinase C mobilization.
- This activation of proteins is involved in the synthesis and secretion of LH and FSH.
- GnRH is degraded by proteolysis within a few minutes.
- GnRH activity is low during childhood, activated at puberty/adolescence.
- GnRH is released in a pulsatile fashion.
Pituitary Gonadotropins
- Anterior pituitary gonadotrope cells respond to GnRH by secreting FSH and LH.
- FSH and LH affect males and females differently, but both act via a two-cell system.
- Gonadotropins stimulate sex steroid synthesis and secretion: estradiol and progesterone in females, and testosterone in males.
- Negative feedback of sex steroids inhibits the hypothalamus and pituitary.
Male Gonadotropin Effects
- FSH stimulates Sertoli cells, which support spermatogenesis.
- LH stimulates Leydig cells, which produce testosterone.
- Testosterone is converted to estradiol by aromatase.
- 5α-reductase converts testosterone to dihydrotestosterone (DHT).
- DHT and testosterone act on androgen receptors (ARs).
Testosterone
- Testosterone plays a role in adult levels during three periods of male life: first trimester of intrauterine life, early neonatal life, and continually after puberty.
- Adult testosterone levels decline with age.
- Testosterone is primarily produced by Leydig cells.
- Testosterone is bound to specific proteins (45% to SHBG, 55% to albumin and corticosteroid-binding globulin).
- A small fraction of testosterone circulates freely.
- Once inside a cell, testosterone either binds to the AR or converts to DHT.
- The androgen-AR complex acts as a transcription factor, binding to hormone response elements in DNA.
Follicle-Stimulating Hormone (FSH)
- FSH is a pituitary glycoprotein hormone.
- The primary target of FSH in the testis is the Sertoli cell.
- FSH indirectly increases the number of Leydig cells, which is key to pubertal development.
- FSH stimulates Sertoli cells, promoting important genes and protein production for steroid hormone synthesis and action.
- FSH supports androgen-binding protein (ABP), P-450 aromatase (converting testosterone to estradiol), growth factors, inhibin production.
Androgens
- Androgens, primarily testosterone and DHT, are responsible for male secondary characteristics.
- Androgens influence protein synthesis, amino acid utilization and skeletal muscle strength.
- They affect erythropoietin (EPO) and hematocrit.
- They affect bone mineral density (BMD), osteoblast growth, and osteocyte apoptosis.
- They affect T cell maturation and autoantibody production.
- Testosterone influences lipogenesis and nervous system activity, and plays a role in tumor growth.
Hypogonadism
- Hypogonadism is a disorder characterized by a defect in testosterone synthesis and can be primary (testis failure) or secondary (pituitary failure).
- Symptoms include loss of skeletal muscle, reduced bone mineral density, reduced sperm levels, sexual dysfunction, fatigue, depression, and testicular atrophy, among others.
- Causes include Klinefelter syndrome, undescended testes, mumps orchitis, hemochromatosis, physical injury, and cancer.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.