Podcast
Questions and Answers
What indicates an acute cholecystitis in a diagnostic procedure?
What indicates an acute cholecystitis in a diagnostic procedure?
Which of the following is NOT a complication associated with severe cases of pancreatitis?
Which of the following is NOT a complication associated with severe cases of pancreatitis?
What condition is characterized by a yellowish discoloration of the skin and eyes due to excess bilirubin?
What condition is characterized by a yellowish discoloration of the skin and eyes due to excess bilirubin?
What imaging technique provides the best differentiation between obstructive and nonobstructive jaundice?
What imaging technique provides the best differentiation between obstructive and nonobstructive jaundice?
Signup and view all the answers
What is a common treatment option for pancreatitis patients with severe symptoms?
What is a common treatment option for pancreatitis patients with severe symptoms?
Signup and view all the answers
What is the primary function of the gallbladder in the hepatobiliary system?
What is the primary function of the gallbladder in the hepatobiliary system?
Signup and view all the answers
Which duct merges with the cystic duct to form the common bile duct?
Which duct merges with the cystic duct to form the common bile duct?
Signup and view all the answers
What triggers the release of bile into the duodenum?
What triggers the release of bile into the duodenum?
Signup and view all the answers
Which enzyme is NOT produced by the pancreas?
Which enzyme is NOT produced by the pancreas?
Signup and view all the answers
What type of imaging is primarily used for identifying calcifications in the hepatobiliary system?
What type of imaging is primarily used for identifying calcifications in the hepatobiliary system?
Signup and view all the answers
Which part of the pancreas is responsible for insulin and glucagon production?
Which part of the pancreas is responsible for insulin and glucagon production?
Signup and view all the answers
What complication can gas in the gallbladder or biliary tree indicate?
What complication can gas in the gallbladder or biliary tree indicate?
Signup and view all the answers
What is a primary use of an Endoscopic Retrograde Cholangiopancreatogram (ERCP)?
What is a primary use of an Endoscopic Retrograde Cholangiopancreatogram (ERCP)?
Signup and view all the answers
Which imaging method is highly accurate for detecting gallstones?
Which imaging method is highly accurate for detecting gallstones?
Signup and view all the answers
What is the primary purpose of T-Tube Cholangiography?
What is the primary purpose of T-Tube Cholangiography?
Signup and view all the answers
How does a CT scan benefit the evaluation of hepatobiliary conditions?
How does a CT scan benefit the evaluation of hepatobiliary conditions?
Signup and view all the answers
Which procedure is useful for detecting deep hepatobiliary lesions?
Which procedure is useful for detecting deep hepatobiliary lesions?
Signup and view all the answers
What is the main characteristic of Alcoholic Hepatitis?
What is the main characteristic of Alcoholic Hepatitis?
Signup and view all the answers
What is the role of Magnetic Resonance Cholangiopancreatography (MRCP)?
What is the role of Magnetic Resonance Cholangiopancreatography (MRCP)?
Signup and view all the answers
During which stage of alcohol-related liver disease does fat begin to accumulate in liver cells?
During which stage of alcohol-related liver disease does fat begin to accumulate in liver cells?
Signup and view all the answers
Which imaging technique can enhance evaluation of complications such as cholecystitis?
Which imaging technique can enhance evaluation of complications such as cholecystitis?
Signup and view all the answers
Which surgical option may be used to alleviate portal hypertension in patients?
Which surgical option may be used to alleviate portal hypertension in patients?
Signup and view all the answers
Which type of hepatitis is transmitted via the fecal-oral route and does not lead to chronic hepatitis?
Which type of hepatitis is transmitted via the fecal-oral route and does not lead to chronic hepatitis?
Signup and view all the answers
What is the gold standard for diagnosing liver conditions?
What is the gold standard for diagnosing liver conditions?
Signup and view all the answers
Which symptom is NOT commonly associated with viral hepatitis?
Which symptom is NOT commonly associated with viral hepatitis?
Signup and view all the answers
Which type of gallstones most commonly occurs and is primarily composed of cholesterol?
Which type of gallstones most commonly occurs and is primarily composed of cholesterol?
Signup and view all the answers
What is a common risk factor for cholelithiasis?
What is a common risk factor for cholelithiasis?
Signup and view all the answers
Which treatment is generally recommended for managing acute nausea and vomiting in hepatitis patients?
Which treatment is generally recommended for managing acute nausea and vomiting in hepatitis patients?
Signup and view all the answers
Which hepatitis virus requires the presence of Hepatitis B for its infection?
Which hepatitis virus requires the presence of Hepatitis B for its infection?
Signup and view all the answers
What is an effective imaging technique for detecting gallstones?
What is an effective imaging technique for detecting gallstones?
Signup and view all the answers
Cholecystitis is primarily associated with which condition?
Cholecystitis is primarily associated with which condition?
Signup and view all the answers
Which of the following imaging techniques is specifically used to assess the extent of ascites and other complications associated with cirrhosis?
Which of the following imaging techniques is specifically used to assess the extent of ascites and other complications associated with cirrhosis?
Signup and view all the answers
Which of the following conditions is NOT a potential cause of cirrhosis?
Which of the following conditions is NOT a potential cause of cirrhosis?
Signup and view all the answers
What is the primary reason for the accumulation of fluid in the abdominal cavity, known as ascites, in patients with cirrhosis?
What is the primary reason for the accumulation of fluid in the abdominal cavity, known as ascites, in patients with cirrhosis?
Signup and view all the answers
What is the primary difference between alcoholic cirrhosis and Nonalcoholic Fatty Liver Disease (NAFLD)?
What is the primary difference between alcoholic cirrhosis and Nonalcoholic Fatty Liver Disease (NAFLD)?
Signup and view all the answers
What imaging technique is specifically utilized to detect fatty deposits in the liver without the need for contrast dyes?
What imaging technique is specifically utilized to detect fatty deposits in the liver without the need for contrast dyes?
Signup and view all the answers
Which of the following complications is directly associated with portal hypertension, a consequence of cirrhosis?
Which of the following complications is directly associated with portal hypertension, a consequence of cirrhosis?
Signup and view all the answers
What is the main goal of treatment for cirrhosis?
What is the main goal of treatment for cirrhosis?
Signup and view all the answers
Which of the following factors is NOT a risk factor for developing Nonalcoholic Fatty Liver Disease (NAFLD)?
Which of the following factors is NOT a risk factor for developing Nonalcoholic Fatty Liver Disease (NAFLD)?
Signup and view all the answers
Which of the following statements about cirrhosis is TRUE?
Which of the following statements about cirrhosis is TRUE?
Signup and view all the answers
What is the primary function of the hepatobiliary scan?
What is the primary function of the hepatobiliary scan?
Signup and view all the answers
Flashcards
Liver
Liver
The largest organ in the body, involved in metabolism, detoxification, and blood synthesis.
Hepatic artery
Hepatic artery
Blood vessel supplying oxygenated blood to the liver.
Portal vein
Portal vein
Vein transporting venous blood from abdominal organs to the liver.
Common bile duct
Common bile duct
Signup and view all the flashcards
Gallbladder
Gallbladder
Signup and view all the flashcards
Sphincter of Oddi
Sphincter of Oddi
Signup and view all the flashcards
Percutaneous Transhepatic Cholangiography (PTC)
Percutaneous Transhepatic Cholangiography (PTC)
Signup and view all the flashcards
Radionuclide Cholescintigraphy
Radionuclide Cholescintigraphy
Signup and view all the flashcards
Acute Cholecystitis
Acute Cholecystitis
Signup and view all the flashcards
Chronic Pancreatitis
Chronic Pancreatitis
Signup and view all the flashcards
Obstructive Jaundice
Obstructive Jaundice
Signup and view all the flashcards
Hepatocellular Adenoma
Hepatocellular Adenoma
Signup and view all the flashcards
TIPSS
TIPSS
Signup and view all the flashcards
Liver transplantation
Liver transplantation
Signup and view all the flashcards
Hepatitis A (HAV)
Hepatitis A (HAV)
Signup and view all the flashcards
Hepatitis B (HBV)
Hepatitis B (HBV)
Signup and view all the flashcards
Hepatitis C (HCV)
Hepatitis C (HCV)
Signup and view all the flashcards
Hepatitis D (HDV)
Hepatitis D (HDV)
Signup and view all the flashcards
Cholelithiasis
Cholelithiasis
Signup and view all the flashcards
Cholecystectomy
Cholecystectomy
Signup and view all the flashcards
Sonography
Sonography
Signup and view all the flashcards
Cholecystitis
Cholecystitis
Signup and view all the flashcards
ERCP
ERCP
Signup and view all the flashcards
Operative Cholangiography
Operative Cholangiography
Signup and view all the flashcards
T-Tube Cholangiography
T-Tube Cholangiography
Signup and view all the flashcards
Real-Time Sonography
Real-Time Sonography
Signup and view all the flashcards
CT in Hepatobiliary System
CT in Hepatobiliary System
Signup and view all the flashcards
SPECT
SPECT
Signup and view all the flashcards
Cholescintigraphy
Cholescintigraphy
Signup and view all the flashcards
MRI Applications
MRI Applications
Signup and view all the flashcards
Alcohol-Induced Liver Disease
Alcohol-Induced Liver Disease
Signup and view all the flashcards
Alcoholic Cirrhosis
Alcoholic Cirrhosis
Signup and view all the flashcards
Nonalcoholic Fatty Liver Disease (NAFLD)
Nonalcoholic Fatty Liver Disease (NAFLD)
Signup and view all the flashcards
Steatosis
Steatosis
Signup and view all the flashcards
Portal Hypertension
Portal Hypertension
Signup and view all the flashcards
Ascites
Ascites
Signup and view all the flashcards
Hepatobiliary Scan
Hepatobiliary Scan
Signup and view all the flashcards
MRI for Liver
MRI for Liver
Signup and view all the flashcards
CT Scan
CT Scan
Signup and view all the flashcards
Liver Biopsy
Liver Biopsy
Signup and view all the flashcards
Liver Dysfunction Symptoms
Liver Dysfunction Symptoms
Signup and view all the flashcards
Study Notes
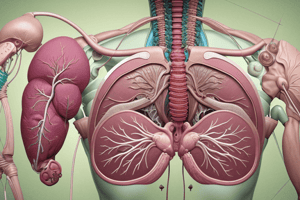
Hepatobiliary System
- The liver is the largest organ in the body, located in the right upper quadrant of the abdomen, protected by the ribs and anchored by peritoneal ligaments.
- Abdominal pressure helps hold the liver in place.
- Liver functions include metabolism of substances from the portal circulation, synthesis of clotting factors and vitamins, and detoxification.
- The liver receives blood from two sources: the hepatic artery (oxygenated blood) and the portal vein (venous blood from the abdominal viscera).
Biliary Tree
- The biliary tree comprises ducts that transport bile from the liver to the duodenum.
- The right and left hepatic ducts merge to form the common hepatic duct.
- The cystic duct from the gallbladder joins the common hepatic duct to form the common bile duct.
- The common bile duct may join with the pancreatic duct before entering the duodenum at the hepatopancreatic ampulla (ampulla of Vater).
- The sphincter of Oddi controls the flow of bile and pancreatic juice into the duodenum, and bile release is triggered by cholecystokinin in response to fatty foods.
Gallbladder
- The gallbladder is a pear-shaped sac located under the liver's right lobe.
- It stores and concentrates bile produced by the liver, releasing it into the duodenum to aid fat digestion.
Pancreas
- The pancreas is an elongated organ behind the stomach, spanning the left abdomen.
- Pancreatic exocrine functions include producing digestive enzymes (trypsin, amylase, lipase) for protein, starch, and lipid digestion, discharging them into the duodenum.
- Pancreatic endocrine functions involve islets of Langerhans (α- and β-cells) that produce insulin and glucagon, regulating carbohydrate metabolism.
Imaging Considerations
- Radiography: Abdominal radiographs are helpful for identifying calcium deposits (calcifications) in the hepatobiliary system and detecting radiopaque gallstones. Visualization of gas in the gallbladder and common bile duct may indicate infection or complications like gallstone ileus or postoperative issues.
- Dynamic Imaging: CT and MRI provide excellent contrast resolution and can be enhanced with Intravenous contrast media for the assessment of masses and conditions like cholecystitis.
- Ultrasound (US): A preferred noninvasive method for evaluating the gallbladder and biliary tree; highly accurate in detecting gallstones and assessing liver conditions.
- Percutaneous Transhepatic Cholangiography (PTC): Involves inserting a needle into the biliary tree to inject contrast medium to differentiate medical from surgical jaundice and detect obstructions or tumors.
- Endoscopic Retrograde Cholangiopancreatography (ERCP): A gastroenterologist utilizes an endoscope to visualize the biliary system and pancreatic duct. It assesses obstructions, bleeding disorders, and pancreatic issues.
- Operative Cholangiography: Performed during surgical procedures like cholecystectomy to detect biliary calculi.
- T-Tube Cholangiography: Post-cholecystectomy procedure to confirm the common bile duct is clear or free of calculi.
Inflammatory Diseases
- Various inflammatory liver diseases exist, such as alcoholic induced liver disease.
- Common types include fatty liver, alcoholic hepatitis, and cirrhosis.
Nonalcoholic Fatty Liver Disease (NAFLD)
- NAFLD is a liver condition characterized by fat accumulation in liver cells (hepatocytes).
- The buildup of fat may not be a result of alcohol consumption but various other factors.
- Early stages often exhibit no symptoms, making diagnosis challenging.
- Weight loss and exercise can help address insulin resistance and metabolic issues.
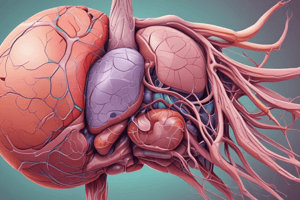
Cirrhosis
- Cirrhosis is a chronic liver condition where healthy liver tissue is replaced by fibrous tissue.
- Causes range from chronic alcohol abuse to diseases.
- Symptoms include jaundice, portal hypertension, and complications like esophageal varices and ascites.
Viral Hepatitis
- Viral hepatitis is a common condition that interferes with the liver's ability to excrete bilirubin.
- This condition is caused by various viruses, resulting in acute liver inflammation.
- Different types of viral hepatitis exist (hepatitis A, B, C, D, E, G), each with varying modes of transmission and courses.
Jaundice
- Jaundice is a sign, not a disease, presenting as yellowish skin and eye discoloration due to bilirubin accumulation.
- Causes of jaundice include hemolytic disease, liver damage, and biliary system obstruction.
- Imaging methods like sonography help differentiate between obstructive and nonobstructive jaundice.
- Common bile duct dilation typically indicates an obstruction.
Neoplastic Diseases
- Neoplastic diseases of the liver include hepatocellular adenoma, hepatocellular carcinoma, hemangiomas, and metastatic liver disease.
- Diagnostic methods may involve sonography, CT, MRI, and liver biopsy.
- Treatments can include surgical resection, chemotherapy, and liver transplantation, depending on the specific type and extent of the neoplasm.
Carcinoma of the Gallbladder
- Gallbladder carcinoma, frequently a malignant adenocarcinomas.
- Symptoms generally include nonspecific abdominal complaints (pain, jaundice) and weight loss.
- Diagnosis often involves CT scan and sonography.
- Prognosis is usually poor due to early metastasis.
Carcinoma of the Pancreas
- Pancreatic carcinoma often presents late with nonspecific symptoms.
- Risk factors include smoking, alcoholism, chronic pancreatitis, diabetes, and family history.
- Diagnosis involves CT scans, sonography, MRI, and barium studies.
- Treatment options involve radical surgery, radiation therapy, and chemotherapy.
- Prognosis is generally poor with a limited 5-year survival rate.
Key Takeaways of Neoplastic Diseases
- Advanced imaging techniques like CT and MRI and sonography are crucial for diagnosis.
- Treatment options are limited and outcomes in some cases, particularly for carcinoma types, often poor.
- Early detection is essential, particularly for conditions like hepatocellular carcinoma and pancreatic cancer.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Test your knowledge on the hepatobiliary system and pancreatitis with these diagnostic and treatment-related questions. This quiz covers conditions like acute cholecystitis, complications of pancreatitis, and the functions of various organs involved. Perfect for medical students or healthcare professionals seeking to refresh their understanding.