Podcast
Questions and Answers
Which of the following best describes the role of the stroma within the bone marrow?
Which of the following best describes the role of the stroma within the bone marrow?
- Producing T and B lymphocytes for the immune response.
- Releasing hormones that stimulate hematopoiesis.
- Providing structural support and connective tissue within the bone marrow. (correct)
- Directly differentiating into erythrocytes and leukocytes.
A patient's blood test reveals a high count of neutrophils. This most likely indicates which condition?
A patient's blood test reveals a high count of neutrophils. This most likely indicates which condition?
- Bacterial infection (correct)
- Allergic reaction
- Thrombocytopenia
- Anemia
Which of the following cell types is NOT derived from the myeloid stem cell line?
Which of the following cell types is NOT derived from the myeloid stem cell line?
- Monocytes
- Platelets
- T Lymphocytes (correct)
- Erythrocytes
After a monocyte leaves the circulation and enters the body tissues, what does it differentiate into?
After a monocyte leaves the circulation and enters the body tissues, what does it differentiate into?
What is the primary mechanism by which macrophages defend the body against foreign invaders?
What is the primary mechanism by which macrophages defend the body against foreign invaders?
If a patient has a history of prolonged bleeding after minor cuts, which cell type is most likely deficient or dysfunctional?
If a patient has a history of prolonged bleeding after minor cuts, which cell type is most likely deficient or dysfunctional?
Which of the following is a function of the reticuloendothelial system (RES)?
Which of the following is a function of the reticuloendothelial system (RES)?
In the context of hematopoiesis, what is the significance of the differentiation of stem cells?
In the context of hematopoiesis, what is the significance of the differentiation of stem cells?
A patient diagnosed with anemia is experiencing persistent fatigue and shortness of breath. Which intervention should the nurse prioritize to address these symptoms?
A patient diagnosed with anemia is experiencing persistent fatigue and shortness of breath. Which intervention should the nurse prioritize to address these symptoms?
A patient undergoing chemotherapy for leukemia develops thrombocytopenia. Which nursing intervention is most important to implement?
A patient undergoing chemotherapy for leukemia develops thrombocytopenia. Which nursing intervention is most important to implement?
A patient with Non-Hodgkin's lymphoma is scheduled for radiation therapy. What potential side effect should the nurse educate the patient about?
A patient with Non-Hodgkin's lymphoma is scheduled for radiation therapy. What potential side effect should the nurse educate the patient about?
A patient with Hodgkin's disease is undergoing treatment that includes chemotherapy. What is a crucial nursing consideration regarding infection prevention for this patient?
A patient with Hodgkin's disease is undergoing treatment that includes chemotherapy. What is a crucial nursing consideration regarding infection prevention for this patient?
A patient with sickle cell anemia is admitted during a vaso-occlusive crisis. Besides pain management & oxygenation, what other intervention is critical in the initial management of this crisis?
A patient with sickle cell anemia is admitted during a vaso-occlusive crisis. Besides pain management & oxygenation, what other intervention is critical in the initial management of this crisis?
A patient is diagnosed with a clotting disorder and is prescribed an anticoagulant. What should the nurse emphasize in patient education?
A patient is diagnosed with a clotting disorder and is prescribed an anticoagulant. What should the nurse emphasize in patient education?
An older adult patient is newly diagnosed with anemia. What normal age-related change should the nurse consider when assessing this patient?
An older adult patient is newly diagnosed with anemia. What normal age-related change should the nurse consider when assessing this patient?
What is the most appropriate way for a nurse to encourage self-care and independence in a patient with a hematologic disorder experiencing fatigue?
What is the most appropriate way for a nurse to encourage self-care and independence in a patient with a hematologic disorder experiencing fatigue?
Which of the following factors has the LEAST influence on the signs and symptoms a patient experiences with anemia?
Which of the following factors has the LEAST influence on the signs and symptoms a patient experiences with anemia?
A patient presents with fatigue, pallor, and complains of shortness of breath upon exertion. Initial blood work reveals low hemoglobin and hematocrit levels. Which of the following diagnostic tests would be MOST helpful in further classifying the type of anemia this patient may have?
A patient presents with fatigue, pallor, and complains of shortness of breath upon exertion. Initial blood work reveals low hemoglobin and hematocrit levels. Which of the following diagnostic tests would be MOST helpful in further classifying the type of anemia this patient may have?
A patient with chronic kidney disease is found to have anemia. The physician suspects 'anemia of chronic disease'. Which of the following management strategies would be MOST appropriate FIRST LINE approach?
A patient with chronic kidney disease is found to have anemia. The physician suspects 'anemia of chronic disease'. Which of the following management strategies would be MOST appropriate FIRST LINE approach?
A patient with a history of multiple transfusions and is experiencing chills and a fever during a transfusion. Which type of transfusion reaction is the MOST likely cause?
A patient with a history of multiple transfusions and is experiencing chills and a fever during a transfusion. Which type of transfusion reaction is the MOST likely cause?
A patient of Mediterranean descent is diagnosed with hemolytic anemia. Further testing reveals a deficiency in an enzyme that protects red blood cells from oxidative damage. Which of the following conditions is MOST likely the cause of this patient's anemia?
A patient of Mediterranean descent is diagnosed with hemolytic anemia. Further testing reveals a deficiency in an enzyme that protects red blood cells from oxidative damage. Which of the following conditions is MOST likely the cause of this patient's anemia?
Which action is MOST important for the nurse to take to prevent transfusion-associated circulatory overload (TACO)?
Which action is MOST important for the nurse to take to prevent transfusion-associated circulatory overload (TACO)?
A patient is diagnosed with aplastic anemia. Which of the following treatment modalities aims to directly stimulate the patient's bone marrow to produce more red blood cells, white blood cells, and platelets?
A patient is diagnosed with aplastic anemia. Which of the following treatment modalities aims to directly stimulate the patient's bone marrow to produce more red blood cells, white blood cells, and platelets?
A patient receiving a platelet transfusion suddenly develops urticaria and itching. What is the MOST appropriate initial intervention by the nurse?
A patient receiving a platelet transfusion suddenly develops urticaria and itching. What is the MOST appropriate initial intervention by the nurse?
A delayed hemolytic reaction is suspected in a patient who received a blood transfusion two weeks ago. Which of the signs/symptoms would the nurse expect to find?
A delayed hemolytic reaction is suspected in a patient who received a blood transfusion two weeks ago. Which of the signs/symptoms would the nurse expect to find?
During a blood transfusion, a patient reports feeling anxious, has a sudden onset of chest tightness, and difficulty breathing. What is the priority nursing intervention?
During a blood transfusion, a patient reports feeling anxious, has a sudden onset of chest tightness, and difficulty breathing. What is the priority nursing intervention?
A patient presents with extreme fatigue, easy bruising, and abnormal bleeding. Which initial assessment would be most appropriate, based on these symptoms?
A patient presents with extreme fatigue, easy bruising, and abnormal bleeding. Which initial assessment would be most appropriate, based on these symptoms?
Which blood product is at HIGHEST risk for bacterial contamination?
Which blood product is at HIGHEST risk for bacterial contamination?
A patient's history reveals prior radiation and chemotherapy treatments. How do these factors primarily contribute to potential hematologic issues?
A patient's history reveals prior radiation and chemotherapy treatments. How do these factors primarily contribute to potential hematologic issues?
What is the PRIMARY cause of an acute hemolytic transfusion reaction?
What is the PRIMARY cause of an acute hemolytic transfusion reaction?
A nurse is educating a patient scheduled for a blood transfusion. Which of the following signs and symptoms should the nurse instruct the patient to report IMMEDIATELY?
A nurse is educating a patient scheduled for a blood transfusion. Which of the following signs and symptoms should the nurse instruct the patient to report IMMEDIATELY?
During a physical assessment, a nurse observes petechiae in the buccal mucosa and a smooth, beefy red tongue. What condition might these findings suggest?
During a physical assessment, a nurse observes petechiae in the buccal mucosa and a smooth, beefy red tongue. What condition might these findings suggest?
A patient is diagnosed with a condition requiring removal of the spleen. What is the primary rationale for considering a splenectomy in this setting?
A patient is diagnosed with a condition requiring removal of the spleen. What is the primary rationale for considering a splenectomy in this setting?
A patient with a hematologic disorder is scheduled for erythrocytapheresis. What is the primary goal of this therapeutic approach?
A patient with a hematologic disorder is scheduled for erythrocytapheresis. What is the primary goal of this therapeutic approach?
Prior to a blood transfusion, what is the most critical assessment a nurse should perform to ensure patient safety?
Prior to a blood transfusion, what is the most critical assessment a nurse should perform to ensure patient safety?
A patient undergoing a blood transfusion develops hives and itching. What type of reaction is the patient most likely experiencing?
A patient undergoing a blood transfusion develops hives and itching. What type of reaction is the patient most likely experiencing?
A patient presents with back pain, loss of height, and kyphosis during a physical assessment for a hematologic disorder. What could these findings indicate?
A patient presents with back pain, loss of height, and kyphosis during a physical assessment for a hematologic disorder. What could these findings indicate?
A patient with a history of CHF is about to receive a blood transfusion. Which intervention is most important for the nurse to implement before starting the transfusion?
A patient with a history of CHF is about to receive a blood transfusion. Which intervention is most important for the nurse to implement before starting the transfusion?
A patient receiving a blood transfusion suddenly develops dyspnea, tachycardia, and an increase in blood pressure. Which complication should the nurse suspect?
A patient receiving a blood transfusion suddenly develops dyspnea, tachycardia, and an increase in blood pressure. Which complication should the nurse suspect?
A patient is suspected of having TRALI following a blood transfusion. What is a key sign or symptom that would support this diagnosis?
A patient is suspected of having TRALI following a blood transfusion. What is a key sign or symptom that would support this diagnosis?
Following the discovery of a transfusion reaction, what is the priority nursing intervention?
Following the discovery of a transfusion reaction, what is the priority nursing intervention?
A patient with anemia is prescribed erythropoietin. How does this medication help to treat anemia?
A patient with anemia is prescribed erythropoietin. How does this medication help to treat anemia?
A patient is diagnosed with anemia due to folate deficiency. Which type of anemia is this classified as?
A patient is diagnosed with anemia due to folate deficiency. Which type of anemia is this classified as?
Which of the following is the most likely cause of hemolytic anemia?
Which of the following is the most likely cause of hemolytic anemia?
A patient receiving a blood transfusion starts to shiver and complains of feeling cold. Their temperature is slightly elevated. What type of transfusion reaction is this patient most likely experiencing?
A patient receiving a blood transfusion starts to shiver and complains of feeling cold. Their temperature is slightly elevated. What type of transfusion reaction is this patient most likely experiencing?
Flashcards
Hematology
Hematology
The study of blood and blood-forming tissues.
Neoplastic Disorders
Neoplastic Disorders
Conditions involving uncontrolled growth of abnormal cells.
Anemia
Anemia
A condition characterized by a deficiency of red blood cells or hemoglobin in the blood, resulting in pallor and fatigue.
Leukemia
Leukemia
Signup and view all the flashcards
Lymphoma
Lymphoma
Signup and view all the flashcards
Hodgkin's Disease
Hodgkin's Disease
Signup and view all the flashcards
Sickle Cell Disease
Sickle Cell Disease
Signup and view all the flashcards
Clotting Disorders
Clotting Disorders
Signup and view all the flashcards
Blood Plasma
Blood Plasma
Signup and view all the flashcards
Hematopoiesis
Hematopoiesis
Signup and view all the flashcards
Stem Cells (Myeloid & Lymphoid)
Stem Cells (Myeloid & Lymphoid)
Signup and view all the flashcards
Myeloid Stem cells
Myeloid Stem cells
Signup and view all the flashcards
Lymphoid Stem Cells
Lymphoid Stem Cells
Signup and view all the flashcards
Neutrophils
Neutrophils
Signup and view all the flashcards
Macrophages (in RES)
Macrophages (in RES)
Signup and view all the flashcards
Kupffer Cells
Kupffer Cells
Signup and view all the flashcards
Hematologic Assessment Findings
Hematologic Assessment Findings
Signup and view all the flashcards
Hematologic Health History Factors
Hematologic Health History Factors
Signup and view all the flashcards
Oral/Lymph Node Signs
Oral/Lymph Node Signs
Signup and view all the flashcards
Systemic Hematologic Signs
Systemic Hematologic Signs
Signup and view all the flashcards
Initial Hematologic Test
Initial Hematologic Test
Signup and view all the flashcards
Cellular Morphology
Cellular Morphology
Signup and view all the flashcards
Splenectomy
Splenectomy
Signup and view all the flashcards
Pre-Transfusion Steps
Pre-Transfusion Steps
Signup and view all the flashcards
Neutropenia
Neutropenia
Signup and view all the flashcards
Hematocrit
Hematocrit
Signup and view all the flashcards
Reticulocyte Count
Reticulocyte Count
Signup and view all the flashcards
Hypoproliferative Anemia
Hypoproliferative Anemia
Signup and view all the flashcards
Hemolytic Anemia
Hemolytic Anemia
Signup and view all the flashcards
Transfusion reaction S/S
Transfusion reaction S/S
Signup and view all the flashcards
Febrile nonhemolytic reaction
Febrile nonhemolytic reaction
Signup and view all the flashcards
Acute hemolytic reaction
Acute hemolytic reaction
Signup and view all the flashcards
Allergic reaction (transfusion)
Allergic reaction (transfusion)
Signup and view all the flashcards
Transfusion-associated circulatory overload (TACO)
Transfusion-associated circulatory overload (TACO)
Signup and view all the flashcards
Bacterial contamination (transfusion)
Bacterial contamination (transfusion)
Signup and view all the flashcards
Delayed hemolytic reaction
Delayed hemolytic reaction
Signup and view all the flashcards
Too much blood
Too much blood
Signup and view all the flashcards
Orthopnea
Orthopnea
Signup and view all the flashcards
Circulatory Overload
Circulatory Overload
Signup and view all the flashcards
TRALI (Transfusion-Related Acute Lung Injury)
TRALI (Transfusion-Related Acute Lung Injury)
Signup and view all the flashcards
TRALI Symptoms
TRALI Symptoms
Signup and view all the flashcards
Transfusion Reaction Steps
Transfusion Reaction Steps
Signup and view all the flashcards
Growth Factors
Growth Factors
Signup and view all the flashcards
Study Notes
Hematologic System
- Blood and blood-forming sites include bone marrow and the reticuloendothelial system (RES).
- Blood consists of plasma (the fluid portion) and blood cells (erythrocytes, leukocytes, thrombocytes).
- Hematopoiesis refers to the formation of blood cells.
Bone Marrow
- Bone marrow contains stem cells, which differentiate into myeloid and lymphoid lineages.
- The Myeloid lineage produces erythrocytes (RBCs), leukocytes (WBCs), and platelets.
- The Lymphoid lineage produces lymphocytes (T cells, B cells & plasma cells).
- Stroma is the part of a tissue or organ with a structural or connective role.
Hematopoiesis
- Hematopoiesis is the complex process of blood cell formation and maturation that occurs in bone marrow.
- Stem cells differentiate into myeloid or lymphoid stem cells.
- Myeloid stem cells differentiate erythrocytes, leukocytes, and platelets.
- Lymphoid stem cells differentiate into either T or B lymphocytes.
Question #2
- Neutrophils increase in number when a patient encounters a bacterial infection.
- Neutrophils are mature, circulating white blood cells.
- Neutrophils increase to phagocytize bacteria during a bacterial infection.
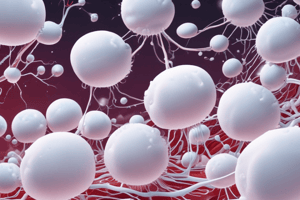
Reticuloendothelial System
- The RES is composed of special tissue macrophages.
- Monocytes released from marrow circulate briefly (about 24 hours) and then enter body tissues.
- Within the tissues, monocytes differentiate into macrophages, which can survive for months or years.
- Macrophages defend the body against bacteria and pathogens via phagocytosis.
- Macrophages remove old or damaged cells, stimulate inflammation, and present antigens to the immune system.
- Macrophages give rise to tissue histiocytes, which are phagocytic cells in loose connective tissue.
- Histiocytes include Kupffer cells of the liver, peritoneal macrophages, and alveolar macrophages.
- The spleen also is part of the RES.
Hemostasis
- Hemostasis occurs in three stages following blood vessel injury:
- Vasoconstriction occurs first.
- Platelet plug formation proceeds after vasoconstriction.
- The final step is blood coagulation.
Assessment of Hematologic Health History
- Assess family history for blood disorders or abnormal bleeding.
- Evaluate history of bleeding: nosebleeds, tooth/gum bleeding, hematuria, menorrhea, hematochezia, GIB, or ulcers.
- Assess for extreme fatigue and for easy, deep bruising.
- Evaluate any abnormal bleeding or joint pain (potential sickle cell disease).
- Review blood cell count for abnormalities.
- Assess for any present illness despite low risk.
- Note any prior radiation/chemotherapy treatments.
- Ask about occupation, especially exposure to military Agent Orange.
- Assess alcohol consumption, diet history, herbal supplement use, and current medications.
Physical Assessment
- Skin: Note any gray, tan, brown or ruddy complexion, ecchymoses, petechiae, conjunctiva hemorrhage, pallor, or jaundice.
- Oral cavity: Check for petechiae in buccal mucosa, beefy red tongue, altered corner of mouth, or enlarged gums.
- Check for enlarged, firm, and fixed lymph nodes.
- Note increased respiratory rate, deep respiration, and adventitious sounds.
- Check for distended neck veins, edema, hypertension, murmur, or gallop.
- Assess for hematuria and proteinuria.
- Musculoskeletal: check for rib/sternal tenderness, back pain, loss of height, kyphosis, or pain/swelling in knees/wrists/hands.
- Abdominal: check for enlarged spleen and liver as well stool positive for occult blood.
- Neurologic: Assess for cranial nerve dysfunction, peripheral nerve dysfunction, visual changes, and headaches.
- Gynecologic: Check for menorrhagia.
Diagnostic Evaluation
- Hematologic studies, such as CBC and peripheral blood smear (RBC, WBC, H/H, and platelets) are important.
- Cellular morphology/shape and appearance are key.
- Bone marrow aspiration and biopsy will provide additional data.
Therapeutic Approaches
- Splenectomy is a surgical procedure in therapeutic approaches.
- Apheresis (Separation) is for platelet pheresis, leukapherisis, erythrocytapheresis, plasmapheresis, and stem cell harvest.
- Hematopoietic stem cell transplantation (HSCT) is a therapeutic approach.
- Phlebotomy and blood component therapy are treatment approches.
- Special preparations may also be used in therapeutic approches.
Blood Transfusion
- Pretransfusion assessment includes history of previous transfusion and reactions, number of pregnancies, and cardiac, pulmonary, and vascular disease.
- Informed consent must be obtained before the procedure.
- Patient education should include signs/symptoms of transfusion reaction.
- Ensure correct administration techniques based on agency policies and procedures.
Transfusion Complications
- Febrile nonhemolytic reaction, acute hemolytic reaction, allergic reaction, TACO, bacterial contamination
- TRALI, delayed hemolytic reaction, disease acquisition, long-term transfusion therapy
Transfusion Complications Explained
- A febrile nonhemolytic reaction is caused by antibodies to donor leukocytes, in patients with prior transfusions and in Rh-negative women with Rh-positive children.
- An acute Hemolytic Reaction is the most dangerous type of transfusion reaction and occurs when donor blood is incompatible with recipient blood.
- An allergic Reaction is due to sensitivity to a plasma protein causing urticaria, itching, and flushing.
- Allergic reactions are usually mild and respond to antihistamines.
Transfusion Complications Explained cont.
- Bacterial Contamination incidence is very low and can occur from procurement/processing.
- Platelets stored at room temperature are at greater risk of contamination.
- A Delayed Hemolytic Reaction usually occurs within 14 days after transfusion. Symptoms include fever, anemia, and jaundice. There may rarely be hemoglobinuria.
Transfusion-Associated Circulatory Overload (TACO)
- Results from too much blood infused too quickly, causing hypervolemia, and is aggravated in patients with CHF, renal dysfunction, advanced age, or acute MI.
- Assess carefully for circulatory overload or positive fluid status before transfusion.
- Pts at risk may be given diuretics before/between units of PRBCs.
- The infusion rate should be titrated to patient's tolerance of less than 100–120 mL/h.
- Signs of circulatory overload include dyspnea, orthopnea, tachycardia, increased blood pressure, sudden anxiety, jugular vein distention, crackles, and hypoxemia. Pulmonary edema can develop quickly, causing severe dyspnea and pink, frothy sputum.
Transfusion-Related Acute Lung Injury (TRALI)
- TRALI is the most common cause of transfusion-related death and is defined as acute lung injury within 6 hours of transfusion.
- This can occur after blood transfusion or blood components, including IVIG, cryoprecipitate, and stem cells.
- Symptoms include acute SOB, hypoxia [SaO2] less than 90%, hypotension, fever, and eventual pulmonary edema.
- A commonly used preventive strategy involves limiting the frequency and amount of blood products transfused.
Nursing Management of Transfusion Reactions
- Stop the transfusion, assess the patient, and notify the primary provider.
- Implement any treatments that are prescribed and continue to monitor.
- Return blood, obtain any necessary samples, and document.
Transfusion Alternatives
- Growth factors (hematopoietic).
- Erythropoietin.
- Granulocyte/macrophage colony-stimulating factor.
- Thrombopoietin to enhance platelet formation.
Chapter 29: Management of Patients with Non-Malignant Hematologic Disorder
- Beginning of second chapter.
Anemia Defined
- Lower than normal levels of hemoglobin and fewer than the normal circulating erythrocytes; it is a sign of an underlying disorder.
- Hypoproliferative: defect in production of erythrocytes (RBCs); caused by deficiency in iron, vitamin B12, or folate erythropoietin.
- Hemolytic: excess destruction of erythrocytes (RBCs); caused by altered erythropoiesis or direct injury to the erythrocyte.
Manifestations of Anemia
- Manifestations depend on the rapidity/duration of anemia, metabolic demands, concurrent problems, and concomitant features.
- General symptoms include fatigue, weakness, and malaise.
- Physical signs include pallor or jaundice.
- Patients may experience cardiac, GI, neurologic, and respiratory symptoms.
- Tongue and nail changes also may occur.
- Angular cheilitits and Pica are also potential signs of anemia.
Symptoms of Anemia
- Eyes - Yellowing
- Skin - Paleness, Coldness and Yellowing
- Respiratory - Shortness of breath
- Muscular - Weakness
- Intestinal - Changed stool color
- Central - Fatigue, Dizziness, Fainting
- Blood vessels - Low blood pressure
- Heart - Palpitations, Rapid heart rate, Chest pain, Angina, Heart attack
- Spleen - Enlargement
Diagnostic Testing for Anemia
- Hemoglobin and hematocrit.
- Reticulocyte count and RBC indices.
- Iron studies, vitamin B12 and Folate.
- Haptoglobin and erythropoietin levels.
- Bone marrow aspiration.
Medical Management of Anemias
- Correct or control the cause of the anemia.
- Provide Transfusion via packed RBCs.
- Treat the condition specific to the anemia.
- Dietary therapy.
- Iron/Vitamin supplementation with iron, folate, B12.
- Transfusions, immunosuppressive therapy, and other treatments as needed.
Hemolytic Anemias
- Sickle cell disease.
- Thalassemia.
- Glucose-6-phosphate dehydrogenase deficiency.
- Immune hemolytic anemia.
- Hereditary hemochromatosis.
- other anemias.
Hypoproliferative Anemias
- Iron deficiency anemia.
- Anemia in renal disease.
- Anemia of inflammation.
- Aplastic anemia.
- Megaloblastic anemia:
- Folic acid deficiency.
- Vitamin B12 deficiency.
Neutropenia
- Neutropenia is defined by decreased production/increased destruction of neutrophils (<2000/mm³).
- Neutropenia leads to increased risk for infection; monitor closely.
- Absolute neutrophil count (ANC).
- Medical management involves treatment dependent on the cause.
- Nursing management involves patient education, preventing/managing complications.
Lymphopenia
- Reduction of lymphocytes to below 1500/mm³.
- Causes:
- Exposure to radiation.
- Long-term use of corticosteroids.
- Infections/Neoplasms/Alcohol abuse.
Polycythemia
- Increased volume of RBCs.
- Excessive production of erythropoietin is associated with reduced oxygen or cyanotic heart disease.
- Nonpathologic associations include smoking, obstructive sleep apnea, sever heart disease, high altitude exposure etc.
- Secondary polycythemia can be the result of neoplasms that stimulate erythropoietic production.
- Treatment not needed if condition is mild:
-Treat underlying cause
- Therapeutic phlebotomy.
Bleeding Disorders #1
- Failure of hemostatic mechanisms.
Causes:
- Trauma.
- Platelet abnormality.
- Coagulation factor abnormality.
- Medical management: the use of specific blood products.
- Nursing management includes limiting injury, assessing for bleeding and bleeding precautions.
Bleeding Disorders #2
- Secondary thrombocytosis.
- Thrombocytopenia.
- Immune thrombocytopenic purpura (ITP).
- Platelet defects.
- Hemophilia.
- von Willebrand disease.
Assessment of the Patient with Anemia
- Includes health history, physical exam, and laboratory data.
- Note the presence of symptoms and their impact on life, such as fatigue, weakness, malaise, and pain.
- Conduct nutritional as well as medication assessments.
- Assess cardiac and GI systems; look for blood loss.
- Neurologic assessment is important.
Complications of Anemia
- Heart failure.
- Angina.
- Paresthesias.
- Confusion.
- Injury related to falls.
- Depressed mood.
Goals & Intervention for the Patient with Anemia
- Major goals include decreased fatigue.
- Maintenence of adequate nutrition and tissue perfusion.
- Promote balance of physical activity/exercise and rest.
- Patient education to promote compliance with medications and nutrition.
- Monitor VS and pulse oximetry; provide supplemental oxygen as needed.
- Monitor for potential complications.
Sickle Cell Disease
- SCD is an autosomal recessive disorder caused by inheriting the sickle hemoglobin (HbS) gene.
- Marked by severe hemolytic anemia.
- The HbS gene causes the erythrocyte to change shape when exposed to low oxygen.
- Erythrocytes are usually pliable/biconcave but become rigid and sickle shaped in this disease.
- Rigid cells adhere to the walls of blood vessels, causing decreased blood flow and ischemia/infarction, with severe pain, swelling, and fever or sickle cell crisis.
- Exposure to oxygen can reverse the process if cell membranes aren't too rigid.
- can be triggered by cold due to vasoconstriction that slows blood flow
Assessment for Sickle Cell Disease
- Collect a comprehensive health history, including a physical examination and pain assessment.
- Get lab data, focusing on S-shaped hemoglobin.
- Identify presence of symptoms; swelling, fever, pain.
- Conduct overall sickle cell crisis assessment.
- Monitor for blood loss along with cardiovascular /neurologic issues.
Complications of Sickle Cell Disease
- Include: hypoxia, ischemia, infection, dehydration and CVA.
- Anemia, acute/chronic kidney disease, and heart failure are potential complications.
- Impotence , along with poor compliance and substance abuse are also complications.
Interventions for the Patient with Sickle Cell Disease
- Pain management.
- Manage fatigue.
- Infection prevention.
- Promote coping and patient education regarding the disease.
- Monitor for complications.
Acquired Coagulation Disorders Acquired Coagulation Disorders
- Liver disease, Vitamin K deficiency, along with complications of anticoagulant therapy.
- Disseminated intravascular coagulation (DIC) and Thrombotic disorders.
- Hyperhomocysteinemia.
- Antithrombin deficiency, along with Protein C & S deficiency
- Activated factor for protein C resistance and Factor 5 Leiden malfunction.
- Also acquired can be Acquired thrombophilia and Malignancy.
Disseminated Intravascular Coagulation (DIC)
- DIC isn't a disease but a sign of an underlying disorder.
- Severity can vary and be fatal.
- Triggers include sepsis, other trauma, cancer and abruptio placenta. -Altered hemostasis leads to clotting in microcirculation. -Clotting factors and platelets are consumed, leading to bleeding.
- Treatment: target underlying cause; correct tissue ischemia.
Pathophysiology of DIC
- Significant illness leads to Activation of coagulation, resulting in activation of fibrinolysis (initially).
- Also forms thrombi, consuming platelets/clotting factors which can lead to bleeding .
- Tissue ischemia then organ failure then death.
Assessment of the Patient with DIC
- Be aware and access those who are at risk to be able to see symptoms and signs of the overall conditions.
- Be able to see signs, symptoms and progression of thrombi, and bleeding.
Complications of DIC
- Include: Kidney injury, Gangrene and Pulmonary embolism or hemorrhage.
- Acute respiratory distress syndrome.
- Stroke.
Goals and Interventions for the Patient with DIC
- hemodynamic state, and maintain intact skin,
- Assessment for signs of damage within in target areas is critical.
- Monitoring and trauma prevention are necessary.
Question #3
- The question statement is true.
- DIC is caused by an alteration of normal homeostasis mechanisms
Chapter 30: Management of Patients with Hematologic Neoplasms
- This chapter deals with hematologic neoplasms.
Leukemia
- Leukemia is hematolymphoid cancer with irregular proliferation.
- The types of leukemia- Acute myeloid, chronic myeloid, acute lymphocytic, chronic lymphocytic.
- Acute Myeloid (AML) Acute Lymphatic (ALL) Chronic Myeloid (CLM) Chronic Lymphatic (CLL)
Assessment of the Patient with Leukemia
- Requires health history.
- Assesses for sign of leukemia and complications related to Anemia.
- Look for weaknesses, fatigue, low leukocytes.
- Culture tests need to be done as needed.
Symptoms of Leukemia
- Nose bleeds, weight loss, swollen lymph nodes, fever and night sweats.
- Can also cause, swollen lymph nodes and easily bleeding.
Complications of the Patient with Leukemia
- Infection along with bleeding/DIC
- Tumor lysis syndrome
- Leukemia can lead to renal failure.
- Tumor lysis syndrome
Acute Myeloid Leukemia (AML)
- This is stem cell defect that separates into all myeloid cells with monocytes, platelets.
- It's the most not common type of leukemia and the rate can peak from 67 and onwards.
- AML has variable to poor prognosis and the manifestations include fever and infection.
Acute Myeloid Leukemia (AML) Treatment
- Treatment can be aggressive with using Chemotherapy and also involves hematopoietic stem cell implementation.
- Treatment can be Antimicrobial combined along with Transfusions in death cases as those are a primary factor.
Chronic Myeloid Leukemia (CML)
- CML involves mutation in myeloid stem cells from Philadelphia chromosomes.
- Stages of CML- chronic, transformational phase and blast crisis.
- Patients over the age of 20 are uncommon, the higher rates are with patients from age 64 upwards.
- Patients may be asymptomatic, but others include malaise, loss of weight can also be caused by leukostasis.
Lymphadenopathy
- Displayed.
Acute Lymphocytic Leukemia (ALL)
- Stem cells have uncontrolled growth from lymphoid cells.
- This it quite common in boys from age 4 forward.
- Its good to note the rate for 3 year is a near 85% chance, that will drop from a lower rate till 45 % as the person gets older.
- Symptoms displayed include severe pain from the liver and CNS.
- Chemotherapy and monoclonal antibody therapy can be used.
Chronic Lymphocytic Leukemia (CLL)
- CLL is a common malignancy of aged adults and a large scale of leukimia.
- The survival rates vary from 2-14 years depending on stages of the disease.
- The "B Cell" stage is defined as a stage when the patient has constellation.
- A stage will include- "watch and wait chemotherapy, IVIG,HSCT.
Planning and Goals for the Patient with Leukemia
- Major goals include the absence of problems and pains.
- Activity tolerance and attainment, in maintenance to care are also necessary.
Interventions for the Patient with Leukemia #1
- Interventions for those at risk with risk of infection.
- Mucositis has Frequent gentle, oral hygiene and frequent dental care are necessary.
- Soft tooth brush is required.
Interventions for the Patient with Leukemia #2
- Improve nutritional intake
- Oral care before and after meals
- Manage and administer analgesics are required before meals.
Interventions for the Patient with Leukemia #3
- Ease pain and discomfort,
- Tylenol for fever and other body aches.
- Decrease fatigue and maintain activity.
Interventions for the Patient with Leukemia #4
- Maintain fluid and electrolytes balance,
- track input and output volumes.
- laboratory study, asses electrolytes.
- Help with self care to help boost confidence.
Myelodysplastic Syndromes (MDS)
- Disorder of the myeloid stem cell that lead to fatigue.
- Those with CBC or bone marrow, or with the mean of 65-70.
- The only cure is with HSCT. Other wise treatment are stem cells.
Autologous Stem Cell Transplantation
- Displayed.
Myeloproliferative Neoplasms
- Polycythemia vera
- Essential thrombocythemia
- Primary myelofibrosis
Polycythemia Vera
- Proliferative disorder of myeloid stem cells.
- Typically diagnosed by the age of 60 and survival of 14-20 years.
- Symptoms include ruddy complexion, and some pressure issues
- Testing done for elevated hematocrit and a acquired mutation.
Polycythemia Vera Treatment
- Initially use phlebotomy and follow with suppression.
- use aggressive management of atherosclerosis.
Essential Thrombocythemia
- Also called primary thrombocythemia.
- Some type of vascular occlusion and the average median age is 65.
- Treatment is for thrombosis or the presence of hemorrhage.
Primary Myelofibrosis
- Those with older age rates are more common of males for more then 14 years.
- It is common for myelopribilosis.
- Treatment is based on reducing the bone density and improving bone count.
Question #1 for Neoplasms
- The statement is false and does not link to the cancer.
- Its due to the number of platelets.
Lymphoma
- Neoplasm of lymphoid origin
- Usually start in lymph nodes but can involve lymphoid tissue in the spleen, GI tract, liver, or bone marrow
- Classified according to degree of cell differentiation and origin of predominant malignant cell
- Two major categories: Hodgkin and Non-Hodgkin lymphoma
Hodgkin Disease
- Rare that the cure is high
- Due to the viral family passing down the generation along family tree then by the age of 50's it comes about. Reed stern berg cells are abnormal that may contain more then 1 nucleas and is fond in folks.
Manifestations Hodgkin Disease
- painless lymph node enlargement;
- Treatment is determined by the stage of the disease
- Radiation and chemo may be required for more serious cases.
Non-Hodgkin Lymphoma Treatment
- Lymphoid tissues become infiltrated with malignant cells
- Treatment for those that are effected, can come down to autoimmune and high exposures
Manifestations non-Hodgkin
- B symptoms/weight loss.
- Radiation may be needed depending on the stage.
Clinical Differences Between Hodgkin
- Shown .
Lymphoma
- Shown.
Question #2
- Is the following statement true or false?
- Hodgkin lymphoma is characterized by highly malignant cells that arise from a variety of tissues?
- Answer here is No.
Question #2 Rationale
- The lymphomas are neoplasms of cells of lymphoid origin; these tumors usually start in lymph nodes.
Multiple Myeloma
- cells that are affecting the bones along with ribs. In time that will fail if you fail to treat your issues.
- Chemotherapy may be required.
Multiple Myeloma Treatment
- The drug consist of a high number of immunomodulatory.
Question #3:
- What should any older adult patient be evaluated for
- If back pain is a constant issue, that is not a good sign and must seek medical attention so it does not make the pain worse.
- Cancer is the answer.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.