Podcast
Questions and Answers
What movement involves bending a limb at a joint?
What movement involves bending a limb at a joint?
- Flexion (correct)
- Extension
- Adduction
- Eversion
Which action is NOT permitted by the temporomandibular joint (TMJ)?
Which action is NOT permitted by the temporomandibular joint (TMJ)?
- Gliding action for side-to-side movement
- Rotational action for chewing (correct)
- Gliding action for protrusion and retraction
- Hinge action to open and close jaws
How does the intervertebral disc function as a shock absorber?
How does the intervertebral disc function as a shock absorber?
- By reinforcing vertebrae against fractures
- By providing stability without movement
- By allowing movement and cushioning through elasticity (correct)
- By absorbing impact through compression only
What is the correct definition of supination?
What is the correct definition of supination?
Which condition can occur if the intervertebral discs experience excessive compression?
Which condition can occur if the intervertebral discs experience excessive compression?
What aspect of health history should be assessed regarding bones?
What aspect of health history should be assessed regarding bones?
Which of the following best assesses limitations in Activities of Daily Living (ADLs)?
Which of the following best assesses limitations in Activities of Daily Living (ADLs)?
Which type of information is least relevant when conducting a patient-centered care assessment?
Which type of information is least relevant when conducting a patient-centered care assessment?
What symptom characteristic should be evaluated when assessing back pain?
What symptom characteristic should be evaluated when assessing back pain?
Which neurological symptoms should be monitored during a health assessment?
Which neurological symptoms should be monitored during a health assessment?
What should be observed when testing muscle strength of prime mover muscle groups?
What should be observed when testing muscle strength of prime mover muscle groups?
What does a grading of 2/5 indicate in muscle strength testing?
What does a grading of 2/5 indicate in muscle strength testing?
What should be taken into account when palpating the temporomandibular joint (TMJ)?
What should be taken into account when palpating the temporomandibular joint (TMJ)?
When testing the integrity of cranial nerve V, which motion is expected?
When testing the integrity of cranial nerve V, which motion is expected?
What indicates a muscle strength grading of 0/5?
What indicates a muscle strength grading of 0/5?
What type of curvature do the cervical and lumbar regions of the spine exhibit?
What type of curvature do the cervical and lumbar regions of the spine exhibit?
Which movement is NOT associated with the shoulder joint?
Which movement is NOT associated with the shoulder joint?
How many cervical vertebrae are present in the human body?
How many cervical vertebrae are present in the human body?
What is the primary function of the rotator cuff muscles?
What is the primary function of the rotator cuff muscles?
Which of the following is a movement type of the elbow joint?
Which of the following is a movement type of the elbow joint?
What type of joint action does the hip joint predominantly perform?
What type of joint action does the hip joint predominantly perform?
What characterizes the thoracic and sacrococcygeal curves of the spine?
What characterizes the thoracic and sacrococcygeal curves of the spine?
What type of joint action is allowed at the radiocarpal joint of the wrist?
What type of joint action is allowed at the radiocarpal joint of the wrist?
What is the most common motion dysfunction found in hip disease?
What is the most common motion dysfunction found in hip disease?
When inspecting the hip joint, which feature is NOT typically assessed?
When inspecting the hip joint, which feature is NOT typically assessed?
What indicates an abnormal alignment of the lower leg during a knee examination?
What indicates an abnormal alignment of the lower leg during a knee examination?
Which test is NOT part of the knee examination?
Which test is NOT part of the knee examination?
During the palpation of the foot, which area is typically assessed?
During the palpation of the foot, which area is typically assessed?
What is indicated by the presence of calluses on the foot during inspection?
What is indicated by the presence of calluses on the foot during inspection?
Which condition is characterized by a pronounced lumbar curve?
Which condition is characterized by a pronounced lumbar curve?
Which observation is a sign of a healthy spinal alignment during inspection?
Which observation is a sign of a healthy spinal alignment during inspection?
What is the primary cause of osteoporosis in postmenopausal women?
What is the primary cause of osteoporosis in postmenopausal women?
Which of the following is a characteristic joint feature of osteoarthritis?
Which of the following is a characteristic joint feature of osteoarthritis?
Which factor is NOT typically associated with an increased risk of developing osteoporosis?
Which factor is NOT typically associated with an increased risk of developing osteoporosis?
What symptom is commonly observed in gouty arthritis?
What symptom is commonly observed in gouty arthritis?
Which of the following is a common contributor to muscle atrophy?
Which of the following is a common contributor to muscle atrophy?
Which condition is associated with a loss of mineralized bone mass?
Which condition is associated with a loss of mineralized bone mass?
What is a common feature of acute rheumatoid arthritis?
What is a common feature of acute rheumatoid arthritis?
Which of the following symptoms is associated with fibromyalgia syndrome?
Which of the following symptoms is associated with fibromyalgia syndrome?
Which factor can contribute to secondary osteoporosis?
Which factor can contribute to secondary osteoporosis?
What physical change occurs in a shoulder affected by a torn rotator cuff?
What physical change occurs in a shoulder affected by a torn rotator cuff?
Flashcards
Spine curves
Spine curves
The vertebral column's shape, characterized by four curves (double-S). Cervical and lumbar curves are concave, while thoracic and sacrococcygeal curves are convex.
Spine motions
Spine motions
The vertebral column can move in several ways; including flexion, extension, abduction (lateral flexion), and rotation.
Vertebrae types
Vertebrae types
The spine consists of 7 cervical, 12 thoracic, 5 lumbar, 5 sacral, and 3-4 coccygeal vertebrae.
Shoulder girdle
Shoulder girdle
Signup and view all the flashcards
Shoulder movements
Shoulder movements
Signup and view all the flashcards
Elbow joint
Elbow joint
Signup and view all the flashcards
Elbow movements
Elbow movements
Signup and view all the flashcards
Wrist joint
Wrist joint
Signup and view all the flashcards
Hip joint
Hip joint
Signup and view all the flashcards
Flexion
Flexion
Signup and view all the flashcards
Extension
Extension
Signup and view all the flashcards
Abduction
Abduction
Signup and view all the flashcards
Adduction
Adduction
Signup and view all the flashcards
Pronation
Pronation
Signup and view all the flashcards
Supination
Supination
Signup and view all the flashcards
Circumduction
Circumduction
Signup and view all the flashcards
Inversion
Inversion
Signup and view all the flashcards
Eversion
Eversion
Signup and view all the flashcards
Rotation
Rotation
Signup and view all the flashcards
Protraction
Protraction
Signup and view all the flashcards
Retraction
Retraction
Signup and view all the flashcards
Elevation
Elevation
Signup and view all the flashcards
Depression
Depression
Signup and view all the flashcards
TMJ (Temporomandibular Joint)
TMJ (Temporomandibular Joint)
Signup and view all the flashcards
Intervertebral discs
Intervertebral discs
Signup and view all the flashcards
Nucleus pulposus
Nucleus pulposus
Signup and view all the flashcards
Herniated disc
Herniated disc
Signup and view all the flashcards
Muscle Strength Testing
Muscle Strength Testing
Signup and view all the flashcards
Bilateral Muscle Strength
Bilateral Muscle Strength
Signup and view all the flashcards
Muscle Strength Grading Scale
Muscle Strength Grading Scale
Signup and view all the flashcards
Full ROM against gravity, full resistance
Full ROM against gravity, full resistance
Signup and view all the flashcards
TMJ Inspection
TMJ Inspection
Signup and view all the flashcards
TMJ Palpation
TMJ Palpation
Signup and view all the flashcards
TMJ Movement Testing
TMJ Movement Testing
Signup and view all the flashcards
Cranial Nerve V (Trigeminal)
Cranial Nerve V (Trigeminal)
Signup and view all the flashcards
TMJ Pain/Swelling
TMJ Pain/Swelling
Signup and view all the flashcards
Osteoarthritis
Osteoarthritis
Signup and view all the flashcards
Osteoporosis
Osteoporosis
Signup and view all the flashcards
Atrophy
Atrophy
Signup and view all the flashcards
Joint Effusion
Joint Effusion
Signup and view all the flashcards
Rotator Cuff Tear
Rotator Cuff Tear
Signup and view all the flashcards
Gouty Arthritis
Gouty Arthritis
Signup and view all the flashcards
Carpal Tunnel Syndrome
Carpal Tunnel Syndrome
Signup and view all the flashcards
Scoliosis
Scoliosis
Signup and view all the flashcards
Spina Bifida
Spina Bifida
Signup and view all the flashcards
Osteoporosis Risks
Osteoporosis Risks
Signup and view all the flashcards
Osteoporosis Prevention
Osteoporosis Prevention
Signup and view all the flashcards
Post-Polio Muscle Atrophy
Post-Polio Muscle Atrophy
Signup and view all the flashcards
Acute Gout
Acute Gout
Signup and view all the flashcards
Fibromyalgia Syndrome
Fibromyalgia Syndrome
Signup and view all the flashcards
Muscle Characteristics
Muscle Characteristics
Signup and view all the flashcards
Symptom Onset/Duration
Symptom Onset/Duration
Signup and view all the flashcards
Bone Pain
Bone Pain
Signup and view all the flashcards
Deformity/Trauma History
Deformity/Trauma History
Signup and view all the flashcards
ROM Limitations
ROM Limitations
Signup and view all the flashcards
Back Pain Characteristics
Back Pain Characteristics
Signup and view all the flashcards
Neurological Deficits
Neurological Deficits
Signup and view all the flashcards
ADLs Assessment
ADLs Assessment
Signup and view all the flashcards
Occupational Hazards
Occupational Hazards
Signup and view all the flashcards
Dietary Review
Dietary Review
Signup and view all the flashcards
Medications
Medications
Signup and view all the flashcards
Supplements
Supplements
Signup and view all the flashcards
Smoking History
Smoking History
Signup and view all the flashcards
Impact on ADLs
Impact on ADLs
Signup and view all the flashcards
Psychological Impact
Psychological Impact
Signup and view all the flashcards
Exercise Patterns
Exercise Patterns
Signup and view all the flashcards
Phalen Test
Phalen Test
Signup and view all the flashcards
Tinel Sign
Tinel Sign
Signup and view all the flashcards
Hip Inspection
Hip Inspection
Signup and view all the flashcards
Hip Palpation
Hip Palpation
Signup and view all the flashcards
Hip ROM
Hip ROM
Signup and view all the flashcards
Knee Inspection
Knee Inspection
Signup and view all the flashcards
Knee ROM
Knee ROM
Signup and view all the flashcards
Ballottement of the Patella
Ballottement of the Patella
Signup and view all the flashcards
Bulge Sign
Bulge Sign
Signup and view all the flashcards
McMurray Test
McMurray Test
Signup and view all the flashcards
Ankle & Foot Inspection
Ankle & Foot Inspection
Signup and view all the flashcards
Ankle & Foot Palpation
Ankle & Foot Palpation
Signup and view all the flashcards
Spine Inspection
Spine Inspection
Signup and view all the flashcards
Spine Palpation
Spine Palpation
Signup and view all the flashcards
Kyphosis
Kyphosis
Signup and view all the flashcards
Lordosis
Lordosis
Signup and view all the flashcards
Study Notes
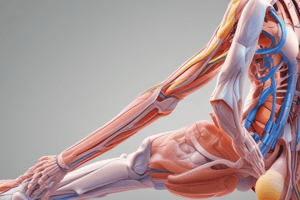
Musculoskeletal System
- The musculoskeletal system comprises bones, joints, and muscles.
- It provides support, allowing an upright stance.
- It's essential for movement.
- It encases and protects vital internal organs.
- It produces red blood cells (RBCs) within bone marrow.
- It stores essential minerals.
Musculoskeletal Components
- Bones and cartilage are specialized connective tissues.
- Fibrous, cartilaginous, and synovial joints are articulation points of two or more bones.
- Joints are places where bones connect.
- Ligaments are fibrous bands connecting bones, strengthening and preventing unwanted movement.
- Bursae are fluid-filled sacs cushioning and reducing friction between tissues.
- Muscles are skeletal, voluntary muscles controlled by conscious thought/action; they are connected to bones by tendons.
Types of Joints
- Fibrous joints are connected by fibrous tissue or cartilage, offering no movement. Sutures in the skull are an example.
- Cartilaginous joints are separated by fibrocartilaginous discs, permitting limited movement. Vertebrae are an example.
- Synovial joints are freely movable, separated by a cavity lined with a synovial membrane that releases synovial fluid. This fluid lubricates the joint and helps to nourish the cartilage; ligaments surround and stabilize the joint.
Terminology
- Articular disease: affecting the joints
- Extra-articular disease: affecting tissues outside the joints
- Crepitation: A crackling or grating sound that may occur during movement, particularly in joints.
Synovial Joint (Diagram)
- Includes cartilage, synovial membrane, synovial cavity, and capsular ligaments
- Facilitates smooth movement
- Exhibits a cushioning function through bursae.
Muscles
- Muscles account for 40-50% of body weight.
- Muscle contractions facilitate movements.
- Muscles are classified as skeletal, smooth, and cardiac.
- This study focuses on voluntary (skeletal) muscles.
- Skeletal muscles contain fasciculi (bundles of muscle fibers).
Skeletal Muscle Movements
- Flexion: bending a limb at a joint
- Extension: straightening a limb at a joint
- Abduction: moving a limb away from the body's midline
- Adduction: moving a limb toward the body's midline
- Pronation: turning the forearm so the palm faces downwards
- Supination: turning the forearm so the palm faces upwards
- Circumduction: moving an arm in a circular motion around the shoulder
- Inversion: moving the sole of the foot inwards towards the midline
- Eversion: moving the sole of the foot outwards away from the midline
- Rotation: movement around a central axis
- Protraction: moving a body part forward, parallel to the ground
- Retraction: moving a body part backward, parallel to the ground
- Elevation: raising a body part
- Depression: lowering a body part
Temporomandibular Joint (TMJ)
- Articulation of mandible and temporal bone.
- Located anterior to the tragus of the ear.
- Three motions:
- Hinge action for opening and closing jaws
- Gliding for protrusion/retraction
- Gliding for side-to-side movement of the lower jaw
Spine and Vertebrae
- Vertebrae are 33 connecting bones vertically stacked
- Intervertebral discs act as shock absorbers.
- Each disc has a soft, semiliquid nucleus pulposus.
- Spinal movement causes compression on one side, with expansion on the other.
- Excessive compression can lead to disc rupture and herniation of the nucleus pulposus into the spinal column.
- It potentially compresses the spinal nerves and causes pain.
Spinal Curvatures
- Spine has a double-S shape with four curves.
- Cervical and lumbar curves are concave (inward)
- Thoracic and sacrococcygeal curves are convex (outward).
Surface Landmarks of Spine
- Vertebrae number in the human body:
- 7 cervical
- 12 thoracic
- 5 lumbar
- 5 sacral
- 3-4 coccygeal
Shoulder Girdle
- Includes humerus, scapula, and clavicle and their associated muscles and tendons
- Provides high mobility to the upper limb (more than in other joint combinations)
- The rotator cuff comprises four important muscles that support the shoulder joint.
Shoulder Joint (Diagram)
- Shows various parts of the shoulder joint including muscles, bursae, and the glenohumeral joint
Rotator Cuff Tear (Diagram)
- Anatomical visual of normal and torn rotator cuff tendons
Elbow and Carpals
- The elbow joint connects the humerus, radius, and ulna.
- Includes the medial and lateral epicondyles, for example.
- The elbow's movement occurs through flexion and extension, with radioulnar joints also present.
- The wrist joint (radiocarpal joint) connects the radius to the carpal bones (in 2 planes).
- Its motions include flexion, extension, rotation, radial, and ulnar deviation.
- The midcarpal joint allows further motion.
Trivia
- Over half the bones in the human body are located in the hands and feet.
Hip
- The hip joint combines the acetabulum and the head of the femur.
- Provides ball-and-socket action.
- Offers stability for weight bearing and enhances movement.
- Important bony landmarks for examination include the iliac crest and the greater trochanter of the femur.
Knee
- The knee joint is an articulation of the femur, tibia, and patella
- Hinge joint: motion occurs in a single plane, with flexion and extension of lower leg on a single plane.
- Contains wedge-shaped cartilages (medial and lateral menisci) to act as cushions.
- Stabilizers of the knee include collateral ligaments (medial and lateral) and cruciate ligaments (anterior and posterior).
Ankle and Foot
- The ankle (tibiotalar) joint comprises the tibia, fibula, and talus.
- A hinge joint that permits flexion (dorsiflexion) and extension (plantar flexion)
- Important landmarks include the medial malleolus and the lateral malleolus.
- Joints below the ankle allow inversion and eversion.
Subjective Data
- Collect information on pain, stiffness, swelling, heat, redness, and limited movement in body joints, muscles, and bones.
- Evaluate knee injuries if present.
Health History Questions
- Joints:
- Pain (location, quality, and severity, onset, duration, frequency).
- Aggravating or precipitating factors
- Associated clinical presentations (limitations of motion, swelling, or erythema)
- Impact on ADLs
- Muscles:
- Location of pain or cramping
- Pain during walking versus rest (consider claudication) if related to peripheral arterial disease (PAD)
- Associated clinical presentations
- Muscle characteristics (weakness, etc)
- Symptom patterns (onset and duration)
- Bones:
- Pain (at rest and/or with movement, associated with posture).
- Deformities or trauma history with impacts on ROM
- History of accidents or trauma & impact on bones
- Medical/surgical treatment (residual deficits)
- Neurological or physical deficits (numbness, tingling, limping, etc.)
Functional Assessment (ADLs)
- Determine the impact of joint, muscle, or bone problems on everyday activities (bathing, dressing, eating, toileting etc).
Patient-Centered Care
- Gather data on occupational hazards, exercise patterns, diet, medications, supplements, smoking history, and impact on activities of daily living (ADLs), psychosocial stressors, pain, depression.
- Explore the impact of acute/chronic disability or self-esteem disturbances.
- Investigate relevant questions about functional abilities and safety risks.
Aging Adult
- Assess for new onset weakness, falls, use of mobility devices.
- Recommend DXA screening as appropriate based on age and risk factors
Physical Examination Preparation
- The aim of musculoskeletal examinations is to gauge function and identify abnormalities related to daily activities.
- Record observations, and note any age-specific abnormalities.
- Begin examination with an orderly approach (head to toe, proximal to distal, & midline outwards).
- Comparative observations between body sides (left and right) helps identify asymmetries and potential problems.
Order of Examination
- Inspection is the initial step. Note joint size, contour, skin color, swelling, and any masses for identification of abnormalities.
- Palpation involves feeling the joint, skin tissues for temperature, tenderness, swelling, bony areas, muscles and the joint capsule for identification of abnormalities.
- Range of motion (ROM) assessment is next. Involves observing active & passive motion, including any limitations.
- Muscle Testing involves probing areas related to prime mover muscle groups and their strengths.
Muscle Grading Scale
- A standardized system grading muscle strength from 0-5.
Temporomandibular Joint (TMJ) - palpation
- Assess for palpation of contracted muscles, especially in relation to teeth clenching.
- Look for clicks/snaps.
- Compare strength and size between both sides of the jaw.
- Utilize resistance to test movement functions, including side-to-side and forward movements
- Note swelling, movement limits, and associated pain or other relevant issues
Cervical Spine
- Observe and document posture & spinal alignment.
- Palpate spinous processes, sternomastoid and trapezius muscle to search for tenderness - especially in relation to muscle spasms
- Check ROM (range of motion), and observe for symmetry in movement.
- Use resistance method for full range of motion testing.
- Note any related neurological or other problems.
Shoulder
- Observe and document shoulder alignment in a posterior and anterior view.
- Test for underlying neck trauma.
- Identify areas of reported discomfort to ensure no related problems to the area.
- Palpate for atrophy, swelling, tenderness, and any muscle spasms.
- Use methodical methods evaluating strength and ROM.
- Ensure appropriate assessment methods for cranial nerve XI, specifically, in relation to the shoulder shrug.
Elbow
- Assess size and contour of elbow joint in both flexed and extended positions.
- Examine for deformity, redness, and swelling; also, palpate the olecranon bursa
- Assess the normally present hollows to check for abnormal swelling
- Palpate with elbow flexed at 70° in relaxed position, using stabilizing techniques to assess ROM and muscle strength accurately.
Wrist and Hand
- Inspect both dorsal and palmar surfaces and look for position, contour, swelling, nodules, redness, deformity.
- Palpate each joint in wrist and hands for assessment of strength and ROM, and examine muscle function
- Use stabilizing techniques for muscle testing, to precisely assess their strength and range of motion.
Testing for Carpal Tunnel Syndrome:
- Phalen Test: Assess median nerve palmaris function.
- Tinel Sign: Assesses median nerve function (used in conjunction with the Phalen test).
Hip
- Simultaneously examine the hip and spine; observe posture alignment of iliac crests, gluteal folds, and buttocks during stance.
- Observe gait for evenness and symmetric movements, as well as range of motion (ROM).
- Examine and palpate hip joints for tenderness or crepitation in a supine posture.
- Assess range of abduction (ability to take the hip away from the body midline) and evaluate any common motion dysfunctions.
Knee
- Ensure the patient is in either a supine or sitting position.
- Observe lower leg alignment, assessing knee shape and contour.
- Screen the quadriceps muscle in the anterior thigh.
- Assess the ROM for limitations and any present pain.
- Perform relevant exams such as ballottement of the patella, bulge sign, and McMurray tests.
Ankle and Foot
- Examine ankles and feet while the patient is standing and during walking, noting joint positions, contour, and any relevant issues.
- Observe the long and longitudinal arches (flat feet status).
- Take note for any calluses or unusual friction patterns present.
- Review any relevant shoes for signs of abnormal wear or accommodation.
- Assess the plantar (pointing downwards) and dorsiflexion (pointing upwards) motions against resistance.
- Palpate metatarsophalangeal joints (between thumbs and fingers).
Spine
- Assess if the patient is standing, draped, and upright.
- Assess and document spinal alignment, posture and relevant abnormalities (kyphosis or lordosis), especially associated with aging
- Evaluate for tenderness and any associated pain as required.
- Assess range of motion (including flexibility, spinal curves, and any problems) to discover any limitations.
Straight Leg Raise (Lasègue's) Test
- Assess back and leg pain, potentially linked to herniated nucleus pulposus.
- Elevate the affected leg (with the knee extended) to just before pain emerges (or to where pain occurs).
- Dorsiflex the foot (flex the foot upward).
- Positive findings would demonstrate sciatic pain.
- The unaffected leg remains flat. Observe the affected leg and inquire into any involved side issues.
Genetics and Environment
- Bone mineral density (BMD): Higher BMD signifies denser bone, while lower BMD predicts hip and vertebral fractures/osteoporosis.
- Racial/ethnic differences: Non-Hispanic Black adults exhibit higher BMD. However, they also face higher mortality after hip fracture.
- Gender differences: Women generally have earlier peak BMD and undergo a more rapid decline compared to men. This is associated with higher fracture risk in post-menopausal white women.
Developmental Competence (Infants, Adolescents, Pregnancy, Aging Adults)
- Infants & Adolescents: Methods of musculoskeletal examination for infants/adolescents are similar to adults. Adolescents commonly experience kyphosis due to prolonged poor posture, but scoliosis is also important to detect.
- Pregnancy: Hormonal changes commonly increase mobility in pregnancy, impacting joints and posture. Progressive lordosis (an exaggerated curve) in the lumbar spine is a common finding.
- Aging adult: Bone remodeling (resorption/deposition) is involved in bone health in aging patients and potentially impacted by factors like low bone mass. Age-related posture changes (e.g., kyphosis) and loss of muscle mass (atrophy) contribute to musculoskeletal issues among the elderly.
Common Musculoskeletal Abnormalities
- Rheumatoid arthritis: Systemic, chronic inflammatory joint disease manifesting with heat, redness, swelling, and especially morning stiffness improving with movement.
- Osteoarthritis: Degenerative, non-inflammatory joint affliction that gradually involves cartilage destruction, frequently accompanied by pain and stiffness.
- Osteoporosis: Bone disease due to reduced bone density/mineral content, rising the risk of fractures. Factors like lack of physical activity contribute to its development in women and older individuals.
- Common abnormalities include joint effusion(fluid build up), torn rotator cuff, gouty arthritis, carpal tunnel syndrome, and scoliosis (abnormal spinal curvature).
Health Promotion and Patient Teaching
- Diet: Maintain a diet rich in calcium & vitamin D to support bone health.
- Smoking Cessation: Important for overall and musculoskeletal health.
- Alcohol Intake: Recommend moderation of alcohol intake for musculoskeletal health.
- Exercise Promotion: Encourage suitable exercise levels (weight-bearing, etc).
- Osteoporosis Screening: Promote screening appropriate for the population based on factors like age.
- Fall prevention: Important for elderly persons (to reduce the risk of fractures).
Additional History Questions related to Aging Adult
- Assess for any losses of function, self-care deficits, or potential safety risks.
- Investigate whether they have had new onset weakness, falls or any stumbling issues.
- Note whether the patient uses a mobility device, which suggests potential concerns with mobility.
- Consider recommendations for DXA screening (for females age 65 or older and/or postmenopausal, younger women).
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.