Podcast
Questions and Answers
During a female genital exam, what specific instruction should be given to empower the patient?
During a female genital exam, what specific instruction should be given to empower the patient?
- "I need you to hold perfectly still."
- "Relax, this will only hurt for a moment."
- "I'm almost finished with the examination."
- "This is the speculum I will use." (correct)
When positioning a patient for a female genital exam, which of the following is the MOST important?
When positioning a patient for a female genital exam, which of the following is the MOST important?
- Hips abducted and externally rotated, head supported with a pillow (correct)
- Hips extended, head unsupported
- Hips adducted, head unsupported
- Hips flexed, head unsupported
During the external examination of the labia majora, what specific characteristics should be inspected?
During the external examination of the labia majora, what specific characteristics should be inspected?
- Lumps, bumps, and crepitus
- Color, symmetry, moisture, scarring, inflammation, and swelling (correct)
- Temperature, sensitivity, and elasticity
- Size, shape, and texture
In a focused note, which element is LEAST likely to be included?
In a focused note, which element is LEAST likely to be included?
What is the potential consequence of using excessive lubricant during a speculum examination?
What is the potential consequence of using excessive lubricant during a speculum examination?
When documenting a patient encounter using a problem-focused note, which of the following sections should contain information gathered through direct questioning of the patient?
When documenting a patient encounter using a problem-focused note, which of the following sections should contain information gathered through direct questioning of the patient?
In the subjective portion of a patient note, especially when evaluating a general medical complaint, which four body systems should always be reviewed in the Review Of Systems?
In the subjective portion of a patient note, especially when evaluating a general medical complaint, which four body systems should always be reviewed in the Review Of Systems?
A patient presents with knee pain. During the history taking, which of the following questions would be MOST important to include in the HPI to guide your differential diagnosis?
A patient presents with knee pain. During the history taking, which of the following questions would be MOST important to include in the HPI to guide your differential diagnosis?
Which of the following best describes the correct order of a physical exam (PE) as it should be documented in the objective portion of a patient note?
Which of the following best describes the correct order of a physical exam (PE) as it should be documented in the objective portion of a patient note?
What is the primary purpose of 'clustering information' when building an assessment for a patient's medical record?
What is the primary purpose of 'clustering information' when building an assessment for a patient's medical record?
In a psychiatric note, the acronym 'Sig E CAPS' is used to assess various symptoms. What does the 'E' in 'Sig E CAPS' stand for?
In a psychiatric note, the acronym 'Sig E CAPS' is used to assess various symptoms. What does the 'E' in 'Sig E CAPS' stand for?
You are seeing a 28-year-old female patient who is 12 weeks pregnant. She has a history of one full-term pregnancy, one spontaneous abortion, and one elective abortion. How would you document this patient's obstetric history using the GTPAL system?
You are seeing a 28-year-old female patient who is 12 weeks pregnant. She has a history of one full-term pregnancy, one spontaneous abortion, and one elective abortion. How would you document this patient's obstetric history using the GTPAL system?
During a focused physical exam, particularly when evaluating a musculoskeletal complaint, which sequence of examination techniques is recommended to be documented in a top-down fashion?
During a focused physical exam, particularly when evaluating a musculoskeletal complaint, which sequence of examination techniques is recommended to be documented in a top-down fashion?
In a focused note, where should pre-morbid conditions and harmful habits like alcohol use (ETOH) be documented?
In a focused note, where should pre-morbid conditions and harmful habits like alcohol use (ETOH) be documented?
Which of the following is the MOST appropriate way to document a patient's complaint in the Chief Complaint (CC) section?
Which of the following is the MOST appropriate way to document a patient's complaint in the Chief Complaint (CC) section?
A patient reports, "I've had a terrible headache for the past three days." How should this be documented in the Chief Complaint (CC)?
A patient reports, "I've had a terrible headache for the past three days." How should this be documented in the Chief Complaint (CC)?
Which of the following components of the HPI focuses on what makes the symptoms better or worse?
Which of the following components of the HPI focuses on what makes the symptoms better or worse?
In which section of a focused note would you document a patient's temperature of 97.5°F, heart rate of 100 bpm, respiratory rate of 28, blood pressure of 160/80 mmHg, oxygen saturation of 99%, weight of 180 lbs, and height of 5’10’’?
In which section of a focused note would you document a patient's temperature of 97.5°F, heart rate of 100 bpm, respiratory rate of 28, blood pressure of 160/80 mmHg, oxygen saturation of 99%, weight of 180 lbs, and height of 5’10’’?
Which of the following historical information is considered subjective?
Which of the following historical information is considered subjective?
A patient's EKG shows sinus tachycardia. Where should this information be documented?
A patient's EKG shows sinus tachycardia. Where should this information be documented?
Which question MOST directly addresses the 'Character' component of the OLDCARTS mnemonic when taking a patient's history?
Which question MOST directly addresses the 'Character' component of the OLDCARTS mnemonic when taking a patient's history?
A 30-year-old female is being seen for a well-woman exam. She has been pregnant twice, has one living child, and had one elective abortion. How would you document her obstetric history using GTPAL?
A 30-year-old female is being seen for a well-woman exam. She has been pregnant twice, has one living child, and had one elective abortion. How would you document her obstetric history using GTPAL?
A 35-year-old female patient presents to the clinic. She reports three pregnancies. She carried one pregnancy to term, resulting in a live birth. Another pregnancy ended in a miscarriage at 10 weeks. She also has a set of twins that were born prematurely but are currently living. How would you accurately record her obstetric history using the GTPAL system?
A 35-year-old female patient presents to the clinic. She reports three pregnancies. She carried one pregnancy to term, resulting in a live birth. Another pregnancy ended in a miscarriage at 10 weeks. She also has a set of twins that were born prematurely but are currently living. How would you accurately record her obstetric history using the GTPAL system?
A clinician notes 'Vaginal mucosa and cervix coated with white homogenous discharge with mild odor.' In the context of a focused note, where would this information be primarily documented?
A clinician notes 'Vaginal mucosa and cervix coated with white homogenous discharge with mild odor.' In the context of a focused note, where would this information be primarily documented?
Why is it generally recommended to use lubricant sparingly, or not at all, when collecting a specimen for a Papanicolaou (Pap) test?
Why is it generally recommended to use lubricant sparingly, or not at all, when collecting a specimen for a Papanicolaou (Pap) test?
Which of the following instruments is NOT typically used during a standard pelvic examination?
Which of the following instruments is NOT typically used during a standard pelvic examination?
Metrorrhagia is best defined as:
Metrorrhagia is best defined as:
According to current guidelines, at what age is it recommended that routine cervical cancer screening should commence for most women?
According to current guidelines, at what age is it recommended that routine cervical cancer screening should commence for most women?
In the context of medical documentation, the primary rationale for thorough and accurate record-keeping is to:
In the context of medical documentation, the primary rationale for thorough and accurate record-keeping is to:
When constructing a focused note, the organization of pertinent positives and negatives within the History of Present Illness (HPI), Review of Systems (ROS), and Physical Exam (PE) sections is crucial for:
When constructing a focused note, the organization of pertinent positives and negatives within the History of Present Illness (HPI), Review of Systems (ROS), and Physical Exam (PE) sections is crucial for:
After collecting subjective and objective information, the subsequent step in developing a focused note is to:
After collecting subjective and objective information, the subsequent step in developing a focused note is to:
A patient has had 3 pregnancies. The first resulted in a single full-term birth. The second pregnancy resulted in the birth of twins at 35 weeks gestation. The third pregnancy ended in a miscarriage at 10 weeks. What is her GTPAL?
A patient has had 3 pregnancies. The first resulted in a single full-term birth. The second pregnancy resulted in the birth of twins at 35 weeks gestation. The third pregnancy ended in a miscarriage at 10 weeks. What is her GTPAL?
In the context of a focused note, the 'Assessment' section is most analogous to what was traditionally known as the:
In the context of a focused note, the 'Assessment' section is most analogous to what was traditionally known as the:
Which of the following elements is typically included in the 'Social History' section of a patient's medical history?
Which of the following elements is typically included in the 'Social History' section of a patient's medical history?
Which of the following best describes the relationship between the 'Assessment' and 'Plan' components of a focused note?
Which of the following best describes the relationship between the 'Assessment' and 'Plan' components of a focused note?
Which of the following is the MOST appropriate action to ensure patient comfort during a pelvic exam?
Which of the following is the MOST appropriate action to ensure patient comfort during a pelvic exam?
What equipment is essential to assemble when preparing for a pelvic exam?
What equipment is essential to assemble when preparing for a pelvic exam?
A 20-year-old patient presents for a routine physical exam and reports no specific complaints or symptoms. According to the guidelines, what is the MOST appropriate course of action regarding a pelvic exam?
A 20-year-old patient presents for a routine physical exam and reports no specific complaints or symptoms. According to the guidelines, what is the MOST appropriate course of action regarding a pelvic exam?
Which of the following is the MOST important reason for a male examiner to have a female chaperone present during a female genitalia exam?
Which of the following is the MOST important reason for a male examiner to have a female chaperone present during a female genitalia exam?
A patient's chart indicates 'G4 T2 P1 A1 L3'. Which of the following is the MOST accurate interpretation of this information?
A patient's chart indicates 'G4 T2 P1 A1 L3'. Which of the following is the MOST accurate interpretation of this information?
During the preparation for a female genitalia exam, what is the purpose of utilizing water-soluble lubricant on the vaginal speculum?
During the preparation for a female genitalia exam, what is the purpose of utilizing water-soluble lubricant on the vaginal speculum?
A patient with a history of which of the following conditions should prompt the examiner to consider a chaperone for a clinical breast exam, even if not explicitly requested?
A patient with a history of which of the following conditions should prompt the examiner to consider a chaperone for a clinical breast exam, even if not explicitly requested?
Which of the following is an accurate GTPAL for a woman who has been pregnant 5 times, had three term deliveries, one preterm delivery, and one spontaneous abortion; three children are living?
Which of the following is an accurate GTPAL for a woman who has been pregnant 5 times, had three term deliveries, one preterm delivery, and one spontaneous abortion; three children are living?
Flashcards
Differential Diagnosis
Differential Diagnosis
A list of possible conditions that could explain a patient's symptoms.
Patient Positioning
Patient Positioning
Positioning the patient for a female genital exam involves flexing and abducting the hips, ensuring external rotation, and providing head support with a pillow.
Patient Communication
Patient Communication
Giving the patient power through your words involves informing the patient on what you are doing, asking for patient permission, and informing the patient where you will touch them during the exam.
VINDICATE Mnemonic
VINDICATE Mnemonic
Signup and view all the flashcards
Subjective Information
Subjective Information
Signup and view all the flashcards
External Genitalia Exam
External Genitalia Exam
Signup and view all the flashcards
Labia Majora Inspection
Labia Majora Inspection
Signup and view all the flashcards
Objective Information
Objective Information
Signup and view all the flashcards
SIG E CAPS Mnemonic
SIG E CAPS Mnemonic
Signup and view all the flashcards
Bartholin Glands Palpation
Bartholin Glands Palpation
Signup and view all the flashcards
Psych Exam Key Components
Psych Exam Key Components
Signup and view all the flashcards
Assessment
Assessment
Signup and view all the flashcards
Plan
Plan
Signup and view all the flashcards
Gravidity (G)
Gravidity (G)
Signup and view all the flashcards
Term (T)
Term (T)
Signup and view all the flashcards
Pre-term (P)
Pre-term (P)
Signup and view all the flashcards
History (Medical)
History (Medical)
Signup and view all the flashcards
Physical Exam Components
Physical Exam Components
Signup and view all the flashcards
Pelvic Exam: Under 21
Pelvic Exam: Under 21
Signup and view all the flashcards
Chaperone Policy
Chaperone Policy
Signup and view all the flashcards
Pelvic Exam - Supplies
Pelvic Exam - Supplies
Signup and view all the flashcards
Lithotomy Position
Lithotomy Position
Signup and view all the flashcards
Pulmonary exam
Pulmonary exam
Signup and view all the flashcards
Vaginal Discharge Description
Vaginal Discharge Description
Signup and view all the flashcards
Lubricant and Pap Smears
Lubricant and Pap Smears
Signup and view all the flashcards
Pelvic Exam Instruments
Pelvic Exam Instruments
Signup and view all the flashcards
Metrorrhagia
Metrorrhagia
Signup and view all the flashcards
Cervical Cancer Screening Age
Cervical Cancer Screening Age
Signup and view all the flashcards
Documentation Importance
Documentation Importance
Signup and view all the flashcards
Focused Note
Focused Note
Signup and view all the flashcards
Assessment Section
Assessment Section
Signup and view all the flashcards
Plan (Documentation)
Plan (Documentation)
Signup and view all the flashcards
Oral Case Presentation
Oral Case Presentation
Signup and view all the flashcards
Chief Complaint (CC)
Chief Complaint (CC)
Signup and view all the flashcards
OLDCARTS (HPI)
OLDCARTS (HPI)
Signup and view all the flashcards
HPI
HPI
Signup and view all the flashcards
Identifying Information
Identifying Information
Signup and view all the flashcards
Additional Subjective Info
Additional Subjective Info
Signup and view all the flashcards
Pending Labs
Pending Labs
Signup and view all the flashcards
Numbered Labs
Numbered Labs
Signup and view all the flashcards
Study Notes
- These study notes cover female genitalia, focused notes, and pulmonology.
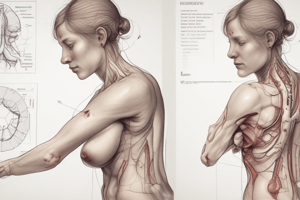
Female Genitalia
- Instructional objectives include describing the anatomy, taking patient history, describing risk factors for cancer/STDs/HIV, and understanding pelvic exam principles.
Helpful Definitions
- Menarche refers to the onset of menses.
- Dysmenorrhea refers to pain with menses, often with bearing down, aching, or cramping in the lower abdomen or pelvis.
- Premenstrual syndrome (PMS) includes emotional, behavioral, and physical symptoms occurring 5 days before menses for three consecutive cycles.
- Abnormal uterine bleeding is bleeding between menses, including infrequent, excessive, prolonged, or postmenopausal bleeding.
- Menopause indicates the absence of menses for 12 consecutive months, usually occurring between 48 and 55 years.
- Postmenopausal bleeding is bleeding occurring after menopause.
- Menorrhagia refers to periods where the bleeding is heavier, or the duration is longer than usual.
- Metrorrhagia refers to bleeding or spotting in between menstruation.
- Menometrorrhagia is a combination of moth menorrhagia and metrorrhagia.
- Polymenorrhea indicates less than 21-day intervals between menses.
- Oligomenorrhea refers to infrequent bleeding.
- Amenorrhea indicates the absence of menses.
- Gravidity refers to the # of times a woman has been pregnant.
- Primigravida indicates a woman who is pregnant now or has been pregnant once.
- Multigravida indicates pregnant more than once.
- Nulligravida indicates never been pregnant more than once.
- Parity is the # of times a woman has given birth to a baby of viable age (≥24 weeks) regardless of birth outcome.
- Primipara (Primip) indicates pregnant for the first time (and has made it beyond viable age) OR has given birth to only 1 child.
- Multipara (Multip) indicates having given birth 2 or more times.
- Nullipara (Nullip) indicates a woman who has never given birth or who has never had a pregnancy progress beyond viability.
- Miscarriage (spontaneous abortion) refers to fetal demise before the 20th week of gestation.
Chief Complaints
- Yearly well-woman visits
- Menarche and menstruation issues are common chief complaints.
- Premenstrual syndrome (PMS) is a key complaint, with criteria including symptoms in the 5 days before menses, symptom cessation within 4 days of menses onset, and interference with daily activities.
- Amenorrhea; primary is the absence of ever initiating periods and secondary is the cessation of periods after initiation
- Abnormal bleeding includes menorrhagia, metrorrhagia, menometrorrhagia, polymenorrhea, oligomenorrhea, and post-coital bleeding.
- Dysmenorrhea is considered abnormal when interfering with ADLs (activities of daily living).
- Primary dysmenorrhea is linked to increased prostaglandin production during the luteal phase of the menstrual cycle.
- Secondary dysmenorrhea can result from endometriosis, adenomyosis, pelvic inflammatory disease (PID), and endometrial polyps.
- Pelvic pain, menopause, vulvovaginal symptoms, STIs, sexual health, pregnancy, and urinary symptoms are also chief complaints.
History
- HPI uses OLDCARTS (Onset, Location, Duration, Character, Aggravating/Alleviating factors, Radiation, Timing, Severity).
- Pertinent positives/negatives.
- Past Medical History:
- Reproductive health history/STI's.
- Assess impact on fertility, risk for ectopic pregnancy, the best contraceptive to prescribe, etc.
- History of UTIs and glomerulonephritis
- Previous urinary catheterization/dilation
- History spina bifida (risk factor for recurrent UTI)
- History of trauma/spinal cord injury
- Medications/form of birth controls
- Surgical history.
- Reproductive History:
- Onset of Menarche
- LNMP
- Obstetric History:
- #Pregnancies
- #Losses/Abortions
- Delivery hx- vaginal vs c-section
- Gyn History:
- Ovarian cyst
- Endometriosis
- Infertility/treatments
- Fibroids
- Salpingitis
- Tubo-ovarian
- Screenings:
- Last pap smear and mammogram
- Sexual History:
- Partners (The 5 "Ps+")
- Genders of sexual partners, recent sexual intercourse, # of partners in the last 6 months, 5 years, and lifetime, any new partners in the last 6 months
- Practices
- Types of sex (oral, vaginal, anal, etc)
- Protection from STIs, Use of condoms.
- Past history of STIs
- What kind, when, what treatment, last screening
- Pregnancy Plans
- Any plans or desire to have (more) children?
- Discuss concerns, birth control, etc
- Plus
- Encompasses an assessment of trauma, violence, sexual satisfaction, sexual health concerns/problems, and support for sexual orientation and gender identity (SOGI)
Gravidity and Parity
- Can be documented succinctly as G and P
- Example woman that is gravida 2, para 2 (G2P2) that has had 2 pregnancies and 2 deliveries after 24 weeks.
- Example woman that is gravida 2, para 0 (G2P0) has had 2 pregnancies and neither survived to a gestational age of 24 weeks.
- G,P(TPAL):
- Gravidity# of pregnancies
- T-Term- # of term pregnancies/deliveries
- 37-40 weeks
- P-Premature- # of premature pregnancies/deliveries
- 20-36 weeks
- A-Abortions/miscarriages
- Elective abortions and spontaneous abortions
- L-Living children
- Example: A woman with two spontaneous losses prior to 20 weeks gestation, 3 living children who were delivered at term, and currently pregnant: G6P3023
- Gravidity: It's about the number of pregnancies, not number of babies.
- P (term and pre-term pregnancies).
History and Physical Exam
- Family History includes history of renal disease, Polycystic Kidney dz, Renal failure, Cancer.
- Sexual history includes history of renal disease, Polycystic Kidney dz, Renal failure, Cancer.
- Review of Systems includes general, skin, pulm, cardiac, GI, GU.
- The physical exam includes vitals, general, skin, pulm, cardiac, GI, rectal when indicated, GU, and pelvic exam.
Female Anatomy
- Key anatomical structures include the mons pubis, labia majora and minora, clitoris, urethral meatus, vaginal introitus, perineum, anus, ovaries, uterus, fallopian tubes, and cervix.
Pelvic Exam
- Pelvic exams should only be performed on patients under 21 years old if indicated by the medical history, such as menstrual disorders, pelvic pain, discharge
- Male and female examiners should be accompanied by a chaperone.
- Patient should avoid intercourse, douching, or use of vaginal suppositories for 24 to 48 hrs before examination and empty her bladder before the examination
Physical Exam Prep
- Assemble equipment
- Moveable light source
- Gloves
- Vaginal speculum of appropriate size
- Water-soluble lubricant.
- The patient should be assisted into lithotomy position, they may feel warmer if they have socks on, ask for a patient to slide to the end of the table
- Touching the patient: "This is the speculum I will use" "We will begin the examination now with your permission "You will feel the back of my hand"
GU: Female Exam
- (and palpation if indicated) of the external genitalia.
- Mons pubis, labia majora and perineum.
- Labia minora, clitoris, urethral meatus, and introitus.
- Anus.
External Exam Inspection
- Pubic hair pattern/distribution on the mons pubis.
- Color, symmetry, moisture, scarring, inflammation, swelling of the labia majora; palpate for tenderness.
- Symmetry, moisture, inflammation, discharge, excoriations, lesions of the labia minora and palpate for tenderness
- Clitoris:
- Size, atrophy, inflammation, adhesions Urinary meatus
- Discharge, polyps, caruncles, inflammation Vaginal introitus
- Moisture, swelling, discoloration, discharge, lesions, fissure Skene and Bartholin glands
- Inspect -Discharge and swelling
- Palpate -Bartholin glands for tenderness
- Palpate each side of the Bartholin glands at approximate the 4- and 8-o'clock position between your finger and thumb.
Speculum Exam
- Need to understand mechanics of the speculum and make sure it's in good working order
- Preferable to lubricate with warm water
- May use lubricant sparingly
- Can prevent accurate pap/culture results so use with caution
Internal Exam-Speculum Exam
- Advise patient you will now place the speculum in the vagina
- Place 1-2 fingers in the posterior introitus and press downward
- if needed, locate the position of the cervix with your fingers to guide the direction of the the speculum
- With speculum closed, insert at an oblique angle and gradually rotate to horizontal position.
- Insert at a 30 degree downward angle towards the cervix.
- Gradually open the speculum, bring cervix into view, and Lock.
- If having difficulty finding the cervix, withdraw slightly and reposition on a different slope.
- If discharge obscures the view, wipe away gently with a large cotton swab.
- Note the color and symmetry of the cervix
- Note the surface characteristics
- Smooth, ectropion, Nabothian cysts, polyps, erythema
- Note the Shape of the os and the presence of any discharge.
- Odor, consistency.
- Obtain a pap smear and cultures if indicated
- Withdraw the speculum just until is clears the cervix and then inspect the vaginal walls.
- Inspect for color, surface characteristics, Lessions, secretions, Or bleeding
- Have the patient bear down and check for bulging in the vaginal wall or incontinence
- Ensured the speculum has cleared the cervix, close the speculum and remove slowly at the same oblique angle.
Papanicolaou (Pap) Smear
- Once the cervix is clearly visualized: Obtain one specimen from the endocervix and another from the. ectocervix
- if indicated/consented: then take cultures from the cervical os TAKE CUTUTRES LAST!!!
Bimanual Examination
- performed from standing position.
- Lubricate index and middle fingers and inform the patient ,you will insert fingers
- Insert fingers exerting pressure posteriorly, with the thumb abducted and 4th and 5th fingers flexed into the palm.
- note any lesions or tenderness
- palpate the cervix
- palpate the uterus
- Palm each ovary (right lower quadrant and abdominal hand)
- Try to identify the right ovary or any adjacent adnexal tissues.
- note the size, shape, consistency, mobility, and tenderness • DRE Note the sphincter tone and any scarring, fissures, lesions, rectal wall masses, polyps, tenderness, uterus position/size/tenderness, stool color, and presence of any blood.
Special Techniques
- Milking the urethra
- to evaluate the possible urethritis or inflammation the paraurethral glands. insert you index finger into the vagina and milk the urethra gently outward.
- Note any discharge from the urethral meatus.
- If discharge is present, culture it.
Abnormal vulvar vaginal lesions
- Herpes simplex- Vesicles/ulcers
- Syphilis
- Cancer
- Bartholin cysts
- HPV- Warts
- Vaginal Pruritus/Pain
- Candidiaisis
- Trichomoiasis
- Herpes simplex-Vesicles
Vaginal Abnormalities
- Vaginal discharge
- Urethritis/cervicitis
- Chlamydia/GC -Mucoprulent discharge -Bacterial Vaginosis- Homeogenous white discharge which coats everything + clue cells and fish odor +whiff -White clumped discharge - Trichomoniasis -Yellow/yellow green odorous and prutitus of vuvla
- Urethritis/cervicitis
-
Lesions
Urethrocele- prolapsed urethra protrudes into the anterior vaginal wall cystocele- buldge of the anterior vaginal wall due to the prolapsed bladder and can be Urethrocele or Cystocele -Rectocele Herniation of the rectum into the posterior wall of the vagina Urethral abnormalities Small read benign tumors visible at the posterior urethral metus. can be asymptomatic but important to rule out carcinoma of this area. Cervix- Can have mucopreulent discharge or cervical abnormalities due to the Fetal exposure of DES Nabothian cysts retention cyst on cervic Fibroids can change in number and size or cause some protusion
Common Abnormalities
- Adnexal masses and other causes of pelvic pain:
- Ovarian cancer
- Ovarian cysts/tumors
- Ectopic pregnancy
- PID
- Dysmenorrhea
- Endometriosis
- Renal Conditions:
- UTI and Pyelonephritis
- Nephrolithiasis
- Gross hematuria
- Glomerulonephritis
- Previous history of streptococcal infection
- Microscopic hematuria
- Nephrotic syndrome
Documentation
- "External genitalia without erythema, lesions, or masses. Vaginal mucosa pink. Cervix parous, pink, and without discharge. Uterus anterior, midline, smooth, and not enlarged. No adnexal tenderness. Pap smear obtained. Rectovaginal wall intact. Rectal vault without masses. Stool brown and negative for fecal blood."
- Or "External genitalia without erythema or lesions. Vaginal mucosa and cervix coated with white homogenous discharge with mild fishy odor. After swabbing cervix, no discharge visible in the cervical os. Uterus midline; no adnexal masses. Rectal vault without masses. Stool brown and negative for fecal blood."
Health Promotion and Education
- Cervical guidelines and cancer screenings
- Pap smears and HPV
Why should lubricant be used sparingly during a pap?
- Could cause inaccurate results
Which IS NOT used during a pelvic exam
- Cannula
Which of the following is metrorrhagia
- Bleeding between menses
At what age should cervical cancer screenings begin
- 21 years old
Writing Focused Notes
- Learning objectives include documentation principles, understanding a focused note's components, organizing HPI/ROS/PE data, analyzing subjective/objective information to develop a diagnosis, creating a differential diagnosis, and generating a patient management plan.
Principles of Documentation
- Notes must provide clear rationale for diagnostics and should have clearly inferred reasons
- They must also identify patients health risks
- Notes must support the reported diagnoses and treatment codes to health insurance.
Detailed Focused Note
- Subjective comes first which has the CC, HPI(full paragraph), PMH, FH, Social History , review of systems
- Objective information comes next which has the PE that is must match the review of systems and lab diagnostics if done by the time of the note, assestments, and plan
Chief Complaint
- Should include all possible information in the patients words that is from quotations.
- It also should has approximately how long the patient states then have been present.
Subjective Material
- Historical information from patient + CC through ROS Example:Mrs. G is a 54-year-old female who reports pain and pressure over the left chest. "It feels like an elephant is sitting on my chest" (for approx I hr).
Objective Material
- Information gathered through physically identifying, testing, lab, or diagnostics.
- General is the location, time, painscale, duration of the pain.
Subjective
- CC is the starting point
- Review of systems and list 3-5 pertinent negatives and positives
How to determine HPI make the Grade
- Determine is there is any infection. recent injuries, and any other health conditions
Steps to developing the differential diagnosis
- After the chief complaint
- List 5 conditions
- List the perimeters of the negative and positives
Things include in subjection information. review of systems. and PMH
Allergies, Cardiac, Gastrointesrtinal and other pertinent findings General system SkinPulmCardiac (These 4 should be included with every CC—then add 2-4more depending on the complaint)
Key PE and what to do
PE (These should be in a top-down fashion) Vital signs (linear fashion) PE ( Pertinent to the CC) ALWAYS perform Gen'l, Skin, Pulm, and Cardio exam (withpulses) Add additional systems according to the CC Labs/Diagnostics (numbered) Any lab/diagnostic that has been completed and RESULTEDgoes hereMust be DATED
Pearls and items of note
It is important to not address more pre-mordid conditions as primary
The plan
Includes all those that are non-medication related and what to be taken into factor such are patient education premodiibity and what issues they patient will likely experience.
Pulmonology
- Student will be to Obtain a thorough patient history specifically regarding complaints of chest pain, shortness of breath, wheezing, cough, and hemoptysis -Gather subjective and objective data for a problem-oriented case
- Provide health maintenance strategies for smoking cessation and proper adult immunizations against influenza and pneumonia
- Identify abnormal disease pattern characteristics during the examination of the thorax and lungs -Utilize the problem list to generate a working differential diagnosis for common pulmonary complaints.
Pulmanary Anatomy
- Describing abnormalities in two dimensions
- Vertical axis
- Circumference of the chest
- Verticle locations, count the ribs and interspaces; sternal angle is the best guide
Location of abnormalities
- To locate findings around the circumference of the chest, imagine a series of vertical lines
- Lungs is divided by lungs, fissure and lobes.
Pleurave
- The trachea bifurcates into its main stem bronchi at the levels of the sternal angle anteriorly and the T4 spinous process posteriorly The pleurae are serous membranes that cover the outer surface of each lung (visceral pleura), and also the inner rib cage and upper surface of the diaphragm (parietal pleura) T4
Common Pulmonary Chief Complaints
- Chesct pain, dyspnea, cough wheezing and hemoptysis.
- Try and have patients describe where the pain is and what type of pain there are having.
Different attributes in both
- sharp stabbing pain
- pressure is squeezing pain
- and Severe chest pain tearing pain
- Attempt to elicit all attributes of the patient's symptom
Dyspena and it effects
Dyspnea is a nonpainful but uncomfortable awareness of breathing that is inappropriate to the level of exertion
- Begin assessment with a broad question, such as, "Have you had any difficulty breathing?"
- Determine the severity of dyspnea based on the patient's daily activities
Different symptoms
- Slow progression of SOB, worse when lying down Heart Failure
- Acute illness, often productive cough Pneumonia
- Sudden onset, pleuritic pain, often young healthy adult Pneumothorax
- Sudden onset, pleuritic pain, risk factors! Pulmonary embolism HPI, past and family history are important to consider!
The examination for Physical and Pulmonary
- The patient should be able to have tachypnea or diaphragms , breathing issues, and cyanosis.
Inspection of Thoracic
- Look for anything abnormal like the pectus excavatum and an increased AP diameter in COPD
How measure Tactile Fremitus
- Consolidation Lobar pneumonia Heavy bronchial secretions Segmental atelectasis Pleural effusion, fibrosis or thickening Massive pulmonary edema Hemothorax
- Reduced vocal reason and how to tell.
Breath sounds
- The patient should be able to have tachypnea or diaphragms , breathing issues, and cyanosis.
The way to measure Health Promotion and Counseling
- Counsel patients
- Talk about lung issues and tobacco cessation.
Key facts
- 2dose series of updated (2023-2024 Formula) Moderna at 0, 4, 8 weeks\
- 3-dose series of updated (2023-2024 Formula) Pfizer- BioNTech at 0, 3, 7 weeks
2-dose series of updated (2023-2024 Formula) Novavax at 03 weeks The patient should have education so that they can benefit and continue to seek support if that area is needed.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Questions about female genital exams, positioning, and documentation with a problem-focused note. Includes key exam steps and important review of systems. Also covers HPI for knee pain.