Podcast
Questions and Answers
What is the primary underlying cause of gouty arthritis?
What is the primary underlying cause of gouty arthritis?
- Autoimmune destruction of cartilage
- Bacterial infection in the joints
- Elevated levels of uric acid in the blood (correct)
- Decreased synovial fluid production
Monosodium urate (MSU) crystals form when serum urate levels exceed what threshold?
Monosodium urate (MSU) crystals form when serum urate levels exceed what threshold?
- 4-5 mg/dL
- 5-6 mg/dL
- 3-4 mg/dL
- 6-7 mg/dL (correct)
The deposition of monosodium urate (MSU) crystals in the synovial fluid and connective tissues leads directly to which of the following?
The deposition of monosodium urate (MSU) crystals in the synovial fluid and connective tissues leads directly to which of the following?
- Reduced joint mobility
- Intense inflammatory response (correct)
- Decreased inflammatory response
- Increased cartilage production
Which cells are primarily responsible for phagocytizing MSU crystals in gout?
Which cells are primarily responsible for phagocytizing MSU crystals in gout?
Which of the following is NOT a typical risk factor for gout?
Which of the following is NOT a typical risk factor for gout?
What is the term for the condition where the first metatarsophalangeal joint is affected in gout?
What is the term for the condition where the first metatarsophalangeal joint is affected in gout?
Why are lower extremities more vulnerable to gout?
Why are lower extremities more vulnerable to gout?
Which of the following is a common characteristic of acute gout attacks?
Which of the following is a common characteristic of acute gout attacks?
Which genetic factors are most closely associated with influencing serum urate levels and the likelihood of developing gout?
Which genetic factors are most closely associated with influencing serum urate levels and the likelihood of developing gout?
What is the term for firm, yellowish-white nodules of MSU crystals found under the skin in chronic gout?
What is the term for firm, yellowish-white nodules of MSU crystals found under the skin in chronic gout?
Which of these comorbidities is least associated with gout?
Which of these comorbidities is least associated with gout?
What is the likely outcome in patients that experience recurrent gout attacks without proper treatment?
What is the likely outcome in patients that experience recurrent gout attacks without proper treatment?
Besides the first metatarsophalangeal joint, which other joints are commonly affected by gout?
Besides the first metatarsophalangeal joint, which other joints are commonly affected by gout?
Which of the following best describes the role of inflammatory cytokines in the pathophysiology of gout?
Which of the following best describes the role of inflammatory cytokines in the pathophysiology of gout?
Men are at a higher risk of gout but after menopause, women's risk increases. What best explains this?
Men are at a higher risk of gout but after menopause, women's risk increases. What best explains this?
What is the significance of urolithiasis in the context of gout?
What is the significance of urolithiasis in the context of gout?
Considering the pathophysiology of gout, which of the following treatments would directly target the underlying cause of MSU crystal formation?
Considering the pathophysiology of gout, which of the following treatments would directly target the underlying cause of MSU crystal formation?
A patient with a history of recurrent gouty arthritis presents with elevated serum urate levels and impaired kidney function. Which of the following interventions would be LEAST appropriate?
A patient with a history of recurrent gouty arthritis presents with elevated serum urate levels and impaired kidney function. Which of the following interventions would be LEAST appropriate?
A researcher is investigating novel therapeutic targets for gout. Which of the following molecular pathways, if successfully inhibited, would MOST directly reduce MSU crystal-induced inflammation within the joint?
A researcher is investigating novel therapeutic targets for gout. Which of the following molecular pathways, if successfully inhibited, would MOST directly reduce MSU crystal-induced inflammation within the joint?
The fact that urate exists as monosodium urate in the body depends on what factor?
The fact that urate exists as monosodium urate in the body depends on what factor?
Flashcards
Gouty Arthritis
Gouty Arthritis
A metabolic inflammatory joint disease resulting from hyperuricemia.
Hyperuricemia
Hyperuricemia
Condition of elevated uric acid in the blood.
Uric Acid
Uric Acid
The final product of purine metabolism; high levels cause gout.
Monosodium Urate (MSU) Crystals
Monosodium Urate (MSU) Crystals
Signup and view all the flashcards
Neutrophils and Macrophages
Neutrophils and Macrophages
Signup and view all the flashcards
Inflammatory Cytokines
Inflammatory Cytokines
Signup and view all the flashcards
Genetic and Epigenetic Factors
Genetic and Epigenetic Factors
Signup and view all the flashcards
Gout Risk Factors
Gout Risk Factors
Signup and view all the flashcards
Kidney Dysfunction
Kidney Dysfunction
Signup and view all the flashcards
Chronic Gouty Arthritis
Chronic Gouty Arthritis
Signup and view all the flashcards
Tophi Formation
Tophi Formation
Signup and view all the flashcards
Acute Gout Attack
Acute Gout Attack
Signup and view all the flashcards
Metatarsophalangeal Joint
Metatarsophalangeal Joint
Signup and view all the flashcards
Podagra
Podagra
Signup and view all the flashcards
Tophi
Tophi
Signup and view all the flashcards
Urolithiasis
Urolithiasis
Signup and view all the flashcards
Study Notes
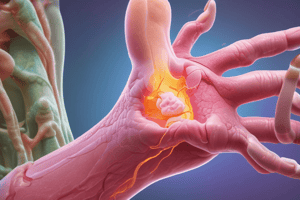
Pathophysiology of Gouty Arthritis
- Gouty arthritis is a metabolic inflammatory joint disease
- Hyperuricemia, or elevated uric acid in the blood, is the primary cause of gout
- Uric acid is the final product of purine metabolism
- When serum urate levels surpass 6–7 mg/dL, monosodium urate (MSU) crystals form and deposit in joints and tissues
- The deposition of MSU crystals in synovial fluid and connective tissues results in an intense inflammatory response
Role of Immune Cells and Cytokines
- Neutrophils and macrophages attempt to phagocytize the crystals
- Phagocytosis leads to the release of inflammatory cytokines like IL-1 and TNF-α, amplifying the inflammatory cascade
Genetic and Risk Factors
- Genetic factors, like variants in urate transporter genes (SLC2A9, URAT1), and epigenetics, influence serum urate levels and gout development
- Risk factors include obesity, metabolic syndrome, hypertension, type 2 diabetes, and renal disease
- Diets rich in purines (red meats, seafood), alcohol (especially beer), and fructose are risk factors
- Using medications affecting serum urate levels like diuretics increases risk
Impact of Kidney Dysfunction
- Kidney dysfunction reduces uric acid excretion, contributing to hyperuricemia
Development of Chronic Gout
- A chronic state may develop, leading to chronic gouty arthritis, tophi formation (MSU crystal aggregates in soft tissues), and joint erosion and deformity
Clinical Manifestations of Gout
- Acute gout attacks usually occur suddenly, often at night
- Acute gout is characterized by severe joint pain, warmth, redness, swelling, and tenderness
- The first metatarsophalangeal joint (big toe) is commonly affected in a condition known as podagra
- Lower extremities are more vulnerable due to cooler temperatures, decreasing MSU solubility
Commonly Affected Joints and Tophi Formation
- Other commonly affected joints include the ankles, knees, wrists, fingers, and elbows
- Tophi, or firm, yellowish-white nodules of MSU crystals, may form under the skin in chronic gout, around joints, bursae, or cartilage
Risk and Complications
- Men are at higher risk, especially with urate levels >420 μmol/L
- Women rarely experience gout before menopause
- Attacks are recurrent
- Without proper treatment, joint destruction and disability can occur
- Patients may have a history of urolithiasis (kidney stones), especially if uric acid levels are persistently elevated
Summary Table: Gouty Arthritis
- Gout is a metabolic inflammatory arthritis caused by hyperuricemia and monosodium urate (MSU) crystal deposition in joints
- Elevated serum uric acid levels can be caused by increased production, decreased excretion, or both
- Pathophysiology involves hyperuricemia leading to MSU crystal formation, followed by crystal deposition in joints, activation of the innate immune system (neutrophils), and an inflammatory cascade triggered by cytokines (IL-1, TNF-α, etc.)
- Lifestyle-related risk factors: high-purine diet, alcohol (esp. beer), fructose. Medical risk factors: obesity, metabolic syndrome, hypertension, and renal disease. Medication risk factors: diuretics, low-dose ASA
- Genetic/environmental factors include urate transporter gene variants (e.g., SLC2A9, URAT1), cell death, lactic acidosis, chemotherapy, and psoriasis
- Common sites affected: first metatarsophalangeal joint (big toe, podagra), ankles, knees, elbows, wrists, fingers
- Clinical manifestations include acute attacks with severe joint pain, redness, swelling, and warmth (usually at night) and tophi (firm nodules from chronic MSU crystal deposits)
- Men are six times more likely to develop gout, while women are usually affected post-menopause Progression:
- Initial stage involves asymptomatic hyperuricemia progressing to acute intermittent gout, which later develops into chronic tophaceous gout with joint damage
- Management involves treating acute attacks with NSAIDs, corticosteroids, or colchicine, and preventing further attacks through lifestyle changes and serum urate-lowering therapy such as allopurinol
- Comorbidities include metabolic syndrome, type 2 diabetes, cardiovascular disease, and urolithiasis
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.