Podcast
Questions and Answers
Which of the following statements accurately describes the pathophysiology of gout?
Which of the following statements accurately describes the pathophysiology of gout?
- Gout is characterized by the excessive excretion of uric acid, causing irritation and swelling in the joints.
- Gout is caused by an overproduction of allantoin, leading to its deposition in joints.
- Gout is primarily caused by a deficiency in purine metabolism, leading to joint inflammation.
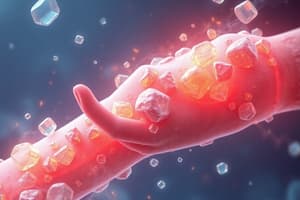
- Gout results from the deposition of monosodium urate crystals in joints and cartilage, triggering an inflammatory response. (correct)
A patient experiencing an acute gout flare in their great toe (podagra) also has a history of hypertension and hyperlipidemia. Which medication should be avoided for pain relief due to its potential to exacerbate one of the patient's existing conditions?
A patient experiencing an acute gout flare in their great toe (podagra) also has a history of hypertension and hyperlipidemia. Which medication should be avoided for pain relief due to its potential to exacerbate one of the patient's existing conditions?
- Colchicine
- Hydrochlorothiazide, a diuretic (correct)
- Naproxen, an NSAID
- Prednisone, a corticosteroid
Which of the following mechanisms explains how allopurinol reduces uric acid levels in the body?
Which of the following mechanisms explains how allopurinol reduces uric acid levels in the body?
- Increasing the renal excretion of uric acid.
- Enhancing the conversion of uric acid to allantoin.
- Inhibiting the xanthine oxidase enzyme. (correct)
- Promoting the breakdown of uric acid crystals in the joints.
A patient with a history of gout and chronic kidney disease (CKD) presents with an acute gout flare. Considering their CKD, which of the following medications requires careful dose adjustment to minimize the risk of adverse effects?
A patient with a history of gout and chronic kidney disease (CKD) presents with an acute gout flare. Considering their CKD, which of the following medications requires careful dose adjustment to minimize the risk of adverse effects?
Which of the following factors contributes most significantly to the crystallization of uric acid in peripheral joints?
Which of the following factors contributes most significantly to the crystallization of uric acid in peripheral joints?
A patient with gout is prescribed allopurinol. What monitoring parameter is most crucial to assess regularly in the initial stages of therapy?
A patient with gout is prescribed allopurinol. What monitoring parameter is most crucial to assess regularly in the initial stages of therapy?
Which of the following risk factors is most directly associated with secondary gout?
Which of the following risk factors is most directly associated with secondary gout?
A 60-year-old male with a history of cardiovascular disease and gout is prescribed febuxostat. What is a primary concern when using febuxostat in this patient population?
A 60-year-old male with a history of cardiovascular disease and gout is prescribed febuxostat. What is a primary concern when using febuxostat in this patient population?
A patient with recurrent gout flares despite being on allopurinol is considered for additional therapy. Which medication would be most appropriate to add if the patient is known to be an underexcretor of uric acid?
A patient with recurrent gout flares despite being on allopurinol is considered for additional therapy. Which medication would be most appropriate to add if the patient is known to be an underexcretor of uric acid?
Why is it recommended to avoid rapid lowering of serum uric acid levels during the initial management of an acute gout flare?
Why is it recommended to avoid rapid lowering of serum uric acid levels during the initial management of an acute gout flare?
A patient starting allopurinol for chronic gout management should also receive which of the following to prevent gout flares?
A patient starting allopurinol for chronic gout management should also receive which of the following to prevent gout flares?
Which of the following non-pharmacological interventions is LEAST likely to benefit a patient with gout?
Which of the following non-pharmacological interventions is LEAST likely to benefit a patient with gout?
What is the primary rationale for recommending a 'treat-to-target' approach in managing gout?
What is the primary rationale for recommending a 'treat-to-target' approach in managing gout?
A patient taking allopurinol develops a rash, fever, and elevated liver enzymes. Which of the following is the most appropriate immediate action?
A patient taking allopurinol develops a rash, fever, and elevated liver enzymes. Which of the following is the most appropriate immediate action?
A patient with gout is prescribed losartan for hypertension. How does losartan potentially benefit gout management?
A patient with gout is prescribed losartan for hypertension. How does losartan potentially benefit gout management?
When is combination therapy most appropriate for treating acute gouty arthritis?
When is combination therapy most appropriate for treating acute gouty arthritis?
Which factor is LEAST likely to influence the choice of treatment for acute gouty arthritis?
Which factor is LEAST likely to influence the choice of treatment for acute gouty arthritis?
Why are opioids generally NOT considered appropriate for treating acute gouty arthritis?
Why are opioids generally NOT considered appropriate for treating acute gouty arthritis?
Which population is at the highest risk for developing Allopurinol Hypersensitivity Syndrome (AHS)?
Which population is at the highest risk for developing Allopurinol Hypersensitivity Syndrome (AHS)?
Which of the following best describes the role of uricase in the human body?
Which of the following best describes the role of uricase in the human body?
A patient with a history of gout is prescribed a new medication for hypertension. Which of the following antihypertensive medications is LEAST likely to increase the risk of gout flares?
A patient with a history of gout is prescribed a new medication for hypertension. Which of the following antihypertensive medications is LEAST likely to increase the risk of gout flares?
What is a key difference in the mechanism of action between allopurinol and febuxostat?
What is a key difference in the mechanism of action between allopurinol and febuxostat?
A patient with a history of gout and peptic ulcer disease requires pain relief during an acute flare. Which of the following is the most appropriate analgesic choice?
A patient with a history of gout and peptic ulcer disease requires pain relief during an acute flare. Which of the following is the most appropriate analgesic choice?
A patient with newly diagnosed gout is found to be positive for the HLA-B*5801 allele. What is the clinical significance of this finding?
A patient with newly diagnosed gout is found to be positive for the HLA-B*5801 allele. What is the clinical significance of this finding?
A patient with well-controlled gout on allopurinol presents with a new diagnosis of hypertension. Which of the following antihypertensive medications should be used with caution due to its potential to interact with allopurinol?
A patient with well-controlled gout on allopurinol presents with a new diagnosis of hypertension. Which of the following antihypertensive medications should be used with caution due to its potential to interact with allopurinol?
What dietary recommendation is most appropriate for a patient with gout to help manage their condition?
What dietary recommendation is most appropriate for a patient with gout to help manage their condition?
A patient with severe tophaceous gout who has failed other therapies is being considered for pegloticase. What is a crucial factor to consider before initiating pegloticase?
A patient with severe tophaceous gout who has failed other therapies is being considered for pegloticase. What is a crucial factor to consider before initiating pegloticase?
A 55-year-old male presents with an acute gout flare. He is currently taking low-dose aspirin (81 mg daily) for cardiovascular protection. What is the recommended course of action regarding his aspirin use?
A 55-year-old male presents with an acute gout flare. He is currently taking low-dose aspirin (81 mg daily) for cardiovascular protection. What is the recommended course of action regarding his aspirin use?
A patient has been diagnosed with gout and has a creatinine clearance of 25 mL/min. Which of the following medications should generally be avoided?
A patient has been diagnosed with gout and has a creatinine clearance of 25 mL/min. Which of the following medications should generally be avoided?
A patient with long-standing gout develops tophi in multiple joints. What is the primary goal of treatment in this scenario?
A patient with long-standing gout develops tophi in multiple joints. What is the primary goal of treatment in this scenario?
A patient is started on allopurinol for gout. Which of the following instructions is most important to provide regarding potential side effects?
A patient is started on allopurinol for gout. Which of the following instructions is most important to provide regarding potential side effects?
Which of the following statements best describes the prevalence of gout?
Which of the following statements best describes the prevalence of gout?
A patient with a history of gout and kidney stones is being considered for urate-lowering therapy. Which of the following medications requires careful consideration due to the potential to increase the risk of kidney stones?
A patient with a history of gout and kidney stones is being considered for urate-lowering therapy. Which of the following medications requires careful consideration due to the potential to increase the risk of kidney stones?
A patient is experiencing a gout flare and reports taking levodopa for Parkinson's disease. How might levodopa contribute to the gout flare?
A patient is experiencing a gout flare and reports taking levodopa for Parkinson's disease. How might levodopa contribute to the gout flare?
Which of the following statements best describes tophi?
Which of the following statements best describes tophi?
Why is it important to check serum uric acid levels after each dose titration of uric acid-lowering therapy?
Why is it important to check serum uric acid levels after each dose titration of uric acid-lowering therapy?
Which of the following is a typical clinical presentation of gout in elderly populations?
Which of the following is a typical clinical presentation of gout in elderly populations?
Flashcards
Hyperuricemia
Hyperuricemia
Elevated serum urate (uric acid) > 6.8 mg/dL.
Tophi
Tophi
Aggregate deposits of sodium urate crystals.
Gout
Gout
Elevated serum urate resulting in recurrent acute arthritis attacks, caused by deposits of monosodium urate crystals.
Primary Gout
Primary Gout
Signup and view all the flashcards
Secondary Gout
Secondary Gout
Signup and view all the flashcards
Purine Metabolism Disorder
Purine Metabolism Disorder
Signup and view all the flashcards
Purine Overproduction
Purine Overproduction
Signup and view all the flashcards
Uric Acid Underexcretion
Uric Acid Underexcretion
Signup and view all the flashcards
Acute Gout Attack
Acute Gout Attack
Signup and view all the flashcards
Tophaceous Gout
Tophaceous Gout
Signup and view all the flashcards
Asymptomatic Hyperuricemia
Asymptomatic Hyperuricemia
Signup and view all the flashcards
Gout Treatment Goals
Gout Treatment Goals
Signup and view all the flashcards
Nonpharmacologic Gout Treatment
Nonpharmacologic Gout Treatment
Signup and view all the flashcards
Acute Gout Attack Medications
Acute Gout Attack Medications
Signup and view all the flashcards
Gout Preventative Medications
Gout Preventative Medications
Signup and view all the flashcards
Xanthine Oxidase Inhibitors (XOIs)
Xanthine Oxidase Inhibitors (XOIs)
Signup and view all the flashcards
Uricosurics
Uricosurics
Signup and view all the flashcards
Allopurinol Mechanism of Action
Allopurinol Mechanism of Action
Signup and view all the flashcards
Febuxostat Mechanism of Action
Febuxostat Mechanism of Action
Signup and view all the flashcards
Probenecid Mechanism of Action
Probenecid Mechanism of Action
Signup and view all the flashcards
Study Notes
- Gout is the most common inflammatory arthritis in the US and western Europe.
- Incidence increases with age, and men are three times more likely to be affected than women due to estrogen's role in uric acid elimination.
- Historically, gout was known as "the disease of kings."
Definitions
- Hyperuricemia: Serum urate (uric acid) level > 6.8 mg/dL.
- Tophi: Aggregate deposits of sodium urate.
- Gout: Recurrent acute arthritis attacks caused by monosodium urate crystal deposits, resulting from elevated serum urate.
- Primary Gout: No identifiable cause, often associated with obesity, alcohol consumption, hypertension, and hypertriglyceridemia.
- Secondary Gout: Result of specific drugs, disorders, lead intoxication, or renal failure.
Gout Risk Factors
- Diet: Purine-rich foods (processed meats, fried foods, high sodium content), high fructose corn syrup.
- Demographics and history: Age, male gender, obesity, family history, elevated uric acid.
- Chemotherapy
- Impaired renal function: Up to 70% of gout patients have CKD.
- Conditions: Renal transplantation, hypertension, hyperlipidemia, congestive heart failure.
Drugs That Can Cause Hyperuricemia
- Diuretics: Thiazide, thiazide-like, loop, mineralocorticoid/potassium-sparing (rare).
- Nicotinic acid
- Salicylates: < 2g/day (low dose ASA).
- Guidelines advise to continue low-dose ASA if patient has gout.
- Ethanol
- Beta-Blockers
- ACE/ARBs: Except losartan.
- Pyrazinamide
- Levodopa
- Ethambutol
- Cyclosporine
- Cytotoxic medications
- Tacrolimus
Pathophysiology
- Purine Metabolism Disorder: The terminal step involves uric acid formation.
- Humans lack uricase, which converts uric acid to water-soluble allantoin.
- Purine Production: Dietary consumption or de novo synthesis.
- Overproduction: Excessive purine amounts overwhelm excretion mechanisms.
- Underexcretion: Affects 90% of patients; 2/3 is removed by kidneys, 1/3 by GI bacteria.
- Crystal Deposition: Monosodium urate crystals deposit in joints and cartilage.
- Uric acid is relatively insoluble; increased levels increase crystallization risk.
- Deposited crystals trigger an acute inflammatory response.
- Crystallization Factors: Low temperature favors crystallization in peripheral regions.
Uric Acid Consequences
- Cardiovascular Risk: Uric acid is an emerging risk factor for cardiovascular diseases.
- Associated conditions: Hypertension, stroke, metabolic disorder, diabetes, kidney disease
- Increased cardiovascular risk is linked to rising uric acid levels due to societal changes.
Clinical Presentation
- Asymptomatic Hyperuricemia: 10- 15% of patients.
- Acute Gout: Rapid onset, usually at night; intense pain, swelling, erythema, warmth; possible mild fever.
- Podagra (great toe): Initial attack site in 50% of cases.
- Untreated attacks last 3-14 days.
- Uncommon clinical presentation
- More common in the elderly
- Chronic polyarticular arthritis
- Multiple small joints in hand, potentially misdiagnosed as rheumatoid arthritis (RA)
- Tophaceous Gout: Urate crystal deposits in soft tissue (cartilage, tendons, synovial membranes).
- Common locations: Ear helix, wrists, hands, elbows, knees, Achilles tendon, base of great toe.
- Complications: Pain, tissue/joint damage/deformity, nerve compression syndromes (e.g., carpal tunnel syndrome).
Provocation of Gout
- Triggers: Infection, stress, trauma/surgery, alcohol ingestion, rapid serum lowering by uric acid-lowering agents, medications increasing serum uric acid.
Diagnosis
- Evaluation: Clinical diagnosis (symptoms and physical exam), elevated uric acid, rule out other forms of arthritis, possibly radiographic imaging.
- Uric Acid Levels: May be normal during an acute attack.
- Gold Standard: Presence of crystals in synovial fluid analysis.
Treatment Goals
- Immediate Goals: Rapid and effective pain relief to terminate acute attacks.
- Intermediate Goals: Prevention of recurrent attacks.
- Target serum UA < 6 mg/dL to improve renal outcomes and reduce acute attack risk.
- Monitor levels post-dose titration.
- Long Term Goals: Prevents complications from chronic urate crystal deposition.
- Overall Goals: Cost-effective therapy while avoiding treatment-related adverse effects.
Nonpharmacologic Treatment
- Acute attacks: Joint rest (1-2 days), ice application.
- Medications: Eliminate non-essential prescriptions causing hyperuricemia. It is conditionally recommended to switch hydrochlorothiazide.
- Hydration: Drink greater than 2L water daily.
- Weight Loss: Recommended in obese/overweight patients.
- Diet Changes: Limit high-fructose corn syrup, purine intake, and alcohol.
- Men ≤ 2 drinks/day; Women ≤ 1 drink/day.
- Guidelines conditionally advise against vitamin C supplementation.
Treatment Types
- Used for acute attacks: NSAIDs, corticosteroids, colchicine, IL-1 inhibitors.
- Opioids are not recommended.
- Used for preventative treatment: Xanthine Oxidase Inhibitors (XOI), Uricosurics, and Pegylated Recombinant Uricase Enzyme.
Acute Gouty Arthritis Treatment
- Monotherapy: Recommended for mild-moderate attacks in few small joints or one large joint.
- Combination Therapy: Recommended for severe pain, especially with multiple small joints or >1 large joint.
Chronic Management of Gout
- Used when 1 flare but infrequent flares, serum urate > 9 mg/dL.
- Not Indicated For:
- Asymptomatic hyperuricemia, even with CKD, urolithiasis, or radiographic changes.
- First “uncomplicated” flare.
- Long-term use, not treating the acute flare.
- Can be started during a flare, and continued during flares.
- Initiate anti-inflammatory therapy during ULT initiation.
Three mechanisms to decrease uric acid
- Decrease synthesis: Xanthine Oxidase Inhibitors (XOI): allopurinol, febuxostat.
- Increase renal excretion: Uricosurics: probenecid.
- Drugs with uricosuric properties: fenofibrate, losartan, SGLT-2 inhibitors.
- Enzymatically degrade: Pegloticase.
American College of Rheumatology (ACR) Recommendations
- First-Line Agent: Allopurinol is the preferred first-line agent.
- Start with a low dose and titrate to reduce flare risk.
- Allopurinol: 50-100 mg daily.
- Febuxostat: 40 mg daily.
- Probenecid: 500 mg once-twice daily.
- Start with a low dose and titrate to reduce flare risk.
- Lower doses recommended for CKD Stage 3 or worse.
- Duration: ULT is recommended indefinitely.
- Initiation: Can start ULT during a gout flare if therapy is indicated.
- Switching Agents: Switch to a second XOI over adding a uricosuric for persistently high SUA despite maximized dose, frequent flares or unresolved tophi.
- Last-Line Treatment: Pegloticase.
Xanthine Oxidase Inhibitors
- First-line agents for decreasing uric acid.
- Recommended over probenecid for patients with CKD Stage 3 or worse.
- Allopurinol preferred due to cost and cardiovascular safety versus febuxostat.
- Efficacy: Similar rates in gout flares and reaching goal UA level.
Allopurinol [Zyloprim®, Aloprim®]
- MOA: Blocks xanthine oxidase enzyme to decrease UA production.
- Active metabolite, oxypurinol, inhibits xanthine oxidase; renally cleared.
- Dose: Initiate at 50-100 mg once daily and titrate every 2-5 weeks to UA < 6 mg/dL.
- Peak effect at 1 week after initiation.
- Doses > 300 mg should be divided for GI tolerability.
- Max dose: 800 mg/day.
- Reduce dose in renal impairment.
- Most patients not titrated to appropriate dose.
- Adverse Effects:
- Mild: Headache, GI problems, urticaria, skin rash, increased AST/ALT.
- Serious: Dose-dependent Stevens Johnson Syndrome(SJS)/Toxic Epidermal Necrolysis(TEN), interstitial nephritis, hepatitis.
- Drug Interactions:
- Thiazides decrease excretion.
- Dose reduction for azathioprine.
- Allopurinol Hypersensitivity Syndrome (AHS):
- Occurs in 1:1000 in the US; 20-25% mortality.
- Symptoms: SJS/TEN, eosinophilia, vasculitis, rash, end-organ damage.
- Pharmacogenetic Testing (HLA-b*5801):
- High-risk populations: Asian (Korean with Stage 3+ CKD, Han Chinese, Thai) and Black populations.
- Recommended testing prior to therapy in high-risk groups.
- Greatest predictor of AHS is initial starting dose; start low, go slow!
- Desensitization: Guidelines conditionally recommend if other oral ULT agents are not suitable.
Febuxostat [Uloric®]
- Role in Therapy:
- Use: May be useful in patients with allopurinol hypersensitivity/intolerance.
- Switch: Guidelines suggest switching patients to alternative oral ULT with CVD history/new CVD-related event.
- MOA: Non-purine selective XOI.
- Inhibits oxidized and reduced forms of xanthine oxidase.
- Dose: 40 mg once daily; increase to 80 mg daily after 2 weeks if UA > 6 mg/dL; can increase to 120 mg if clinically needed.
- No dosage adjustments for mild-moderate renal disease.
- Adverse Effects: Diarrhea, rash, nausea, blood dyscrasias, arthritis, eosinophilia.
- Liver enzyme elevations: Requires LFT monitoring: baseline, 2 months, 4 months.
- Excretion: Equal excretion into urine and feces after liver metabolism.
- Contraindications: Azathioprine, mercaptopurine.
- Precautions: High rate of cardiovascular events compared to allopurinol: MI, stroke, heart-related death.
- FDA Safety Alert:
- CARES study found febuxostat non-inferior to allopurinol for CV adverse events.
- All-cause and CV mortality higher in febuxostat group.
- Serum UA lowering may be less effective in patients with higher previous allopurinol dose, renal impairment, male gender.
Uricosurics
- Increases renal excretion of uric acid.
- Role in Therapy: May be useful as an add-on to XOI if XOI alone doesn't reach UA goal.
- Best for underexcretors, but guidelines don't recommend 24-hour urine before starting.
- Probenecid:
- MOA: Increases renal excretion by decreasing renal tubular reabsorption.
- Kidney Stones: May cause kidney stone formation (9-11%).
- Maintain adequate urine flow and alkalization.
- Dose: 250 mg BID for 1 week; may increase to 500 mg BID.
- Start at low dose and titrate.
- Max dose: 2 g/day.
- Contraindications: Avoid use if CrCl < 30 mL/min.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.