Podcast
Questions and Answers
What is the primary function of the glomeruli in the kidneys?
What is the primary function of the glomeruli in the kidneys?
- To regulate blood pressure
- To produce hormones
- To filter waste and excess fluids from the blood (correct)
- To maintain electrolyte balance
Which of the following is a consequence of damage to the glomeruli?
Which of the following is a consequence of damage to the glomeruli?
- Proteinuria (correct)
- Hyperfiltration
- Fluid retention in the bladder
- Urinary incontinence
What is a significant characteristic of primary glomerular disease?
What is a significant characteristic of primary glomerular disease?
- It usually affects multiple organs
- It leads to immediate kidney failure
- It is always caused by diabetes
- It primarily affects the kidneys only (correct)
Which of the following diseases is classified as a secondary glomerular disease?
Which of the following diseases is classified as a secondary glomerular disease?
What is the significance of early detection of glomerular diseases?
What is the significance of early detection of glomerular diseases?
Which type of microscope is used to examine the structure of glomeruli and tubules in a renal biopsy?
Which type of microscope is used to examine the structure of glomeruli and tubules in a renal biopsy?
What can chronic glomerular diseases potentially lead to?
What can chronic glomerular diseases potentially lead to?
Which of the following is NOT seen as a complication of glomerular diseases?
Which of the following is NOT seen as a complication of glomerular diseases?
What type of microscopy is used to detect the site of immune complex in the glomeruli?
What type of microscopy is used to detect the site of immune complex in the glomeruli?
What is the primary pathological change observed in minimal change disease?
What is the primary pathological change observed in minimal change disease?
Which of the following is associated with post-streptococcal glomerulonephritis?
Which of the following is associated with post-streptococcal glomerulonephritis?
Which feature is NOT typically found in minimal change disease under light microscopy?
Which feature is NOT typically found in minimal change disease under light microscopy?
What is a common clinical presentation of post-streptococcal glomerulonephritis?
What is a common clinical presentation of post-streptococcal glomerulonephritis?
What typically happens to proteinuria in patients with minimal change disease after corticosteroid treatment?
What typically happens to proteinuria in patients with minimal change disease after corticosteroid treatment?
What type of immune deposits are typically observed in post-streptococcal glomerulonephritis under immunofluorescence?
What type of immune deposits are typically observed in post-streptococcal glomerulonephritis under immunofluorescence?
Which of these is a possible fate of minimal change disease?
Which of these is a possible fate of minimal change disease?
What is the most common age group for the occurrence of Nephroblastoma (Wilms tumor)?
What is the most common age group for the occurrence of Nephroblastoma (Wilms tumor)?
Which genetic alteration is implicated in the tumorigenesis of Nephroblastoma?
Which genetic alteration is implicated in the tumorigenesis of Nephroblastoma?
What is a common clinical presentation of Nephroblastoma?
What is a common clinical presentation of Nephroblastoma?
Which syndrome is associated with aniridia in Nephroblastoma patients?
Which syndrome is associated with aniridia in Nephroblastoma patients?
What is the estimated percentage of Nephroblastoma cases that are familial?
What is the estimated percentage of Nephroblastoma cases that are familial?
What is indicated by an increase in alkaline phosphatase in Nephroblastoma patients?
What is indicated by an increase in alkaline phosphatase in Nephroblastoma patients?
Which of the following is NOT a symptom associated with Nephroblastoma?
Which of the following is NOT a symptom associated with Nephroblastoma?
Nephroblastoma has a slight female preponderance. What could this imply?
Nephroblastoma has a slight female preponderance. What could this imply?
Which risk factor is commonly associated with both low-grade and high-grade non-invasive papillary urothelial carcinoma?
Which risk factor is commonly associated with both low-grade and high-grade non-invasive papillary urothelial carcinoma?
What histopathological feature distinguishes high-grade non-invasive papillary urothelial carcinoma from low-grade?
What histopathological feature distinguishes high-grade non-invasive papillary urothelial carcinoma from low-grade?
What is the typical age group for patients diagnosed with high-grade non-invasive papillary urothelial carcinoma?
What is the typical age group for patients diagnosed with high-grade non-invasive papillary urothelial carcinoma?
Which of the following IHC markers would be positive in high-grade non-invasive papillary urothelial carcinoma?
Which of the following IHC markers would be positive in high-grade non-invasive papillary urothelial carcinoma?
What is the prognosis for patients with high-grade non-invasive papillary urothelial carcinoma regarding progression to invasive urothelial carcinoma?
What is the prognosis for patients with high-grade non-invasive papillary urothelial carcinoma regarding progression to invasive urothelial carcinoma?
What is one of the distinguishing features of urothelial carcinoma in-situ compared to non-invasive papillary tumors?
What is one of the distinguishing features of urothelial carcinoma in-situ compared to non-invasive papillary tumors?
Which mutation is a significant part of the pathogenesis of high-grade non-invasive papillary urothelial carcinoma?
Which mutation is a significant part of the pathogenesis of high-grade non-invasive papillary urothelial carcinoma?
Which of the following features would NOT be expected in the morphology of low-grade non-invasive papillary urothelial carcinoma?
Which of the following features would NOT be expected in the morphology of low-grade non-invasive papillary urothelial carcinoma?
What is the characteristic cellular infiltrate associated with Acute Interstitial Nephritis (AIN)?
What is the characteristic cellular infiltrate associated with Acute Interstitial Nephritis (AIN)?
Which symptom is NOT typically associated with cystitis?
Which symptom is NOT typically associated with cystitis?
What can potentially reverse Acute Interstitial Nephritis (AIN)?
What can potentially reverse Acute Interstitial Nephritis (AIN)?
What is the minimum bacterial count in urine that is considered significant for diagnosing a urinary tract infection (UTI)?
What is the minimum bacterial count in urine that is considered significant for diagnosing a urinary tract infection (UTI)?
Which factor does NOT normally protect against urinary tract infections?
Which factor does NOT normally protect against urinary tract infections?
Which type of cystitis is characterized by inflammation not resulting from an infection?
Which type of cystitis is characterized by inflammation not resulting from an infection?
What is one of the major manifestations of interstitial cystitis commonly seen in women aged 20 to 30?
What is one of the major manifestations of interstitial cystitis commonly seen in women aged 20 to 30?
In terms of urine characteristics, what symptom may indicate a urinary tract infection?
In terms of urine characteristics, what symptom may indicate a urinary tract infection?
What is a defining characteristic of nephrotic syndrome related to protein levels?
What is a defining characteristic of nephrotic syndrome related to protein levels?
Which statement about the pathophysiology of nephrotic syndrome is correct?
Which statement about the pathophysiology of nephrotic syndrome is correct?
Which of the following is NOT considered a primary cause of nephrotic syndrome?
Which of the following is NOT considered a primary cause of nephrotic syndrome?
Which complication is commonly associated with nephrotic syndrome?
Which complication is commonly associated with nephrotic syndrome?
What type of oedema is commonly observed in nephrotic syndrome?
What type of oedema is commonly observed in nephrotic syndrome?
Which of the following is a secondary cause of minimal change disease?
Which of the following is a secondary cause of minimal change disease?
What is a potential differential diagnosis for nephrotic syndrome?
What is a potential differential diagnosis for nephrotic syndrome?
Which of the following clinical signs is associated with nephrotic syndrome?
Which of the following clinical signs is associated with nephrotic syndrome?
Flashcards
Glomerular Diseases
Glomerular Diseases
A group of conditions that damage the glomeruli – the kidney's filtration units. This damage impairs kidney function, leading to problems like proteinuria, hematuria, and reduced GFR.
Proteinuria
Proteinuria
The presence of excess protein in the urine, often a sign of glomerular damage, as it indicates that the filtering system is not working properly.
Hematuria
Hematuria
Blood in urine, often indicating damage to the glomeruli or other parts of the urinary tract.
Reduced Glomerular Filtration Rate (GFR)
Reduced Glomerular Filtration Rate (GFR)
Signup and view all the flashcards
Minimal Change Glomerular Disease (Lipoid Nephrosis)
Minimal Change Glomerular Disease (Lipoid Nephrosis)
Signup and view all the flashcards
Acute Diffuse Proliferative Glomerulonephritis (GN)
Acute Diffuse Proliferative Glomerulonephritis (GN)
Signup and view all the flashcards
Rapidly Progressive Glomerulonephritis (GN)
Rapidly Progressive Glomerulonephritis (GN)
Signup and view all the flashcards
Systemic Lupus Erythematosus (SLE)
Systemic Lupus Erythematosus (SLE)
Signup and view all the flashcards
IF (Immunofluorescent microscopy)
IF (Immunofluorescent microscopy)
Signup and view all the flashcards
EM (Electron microscopy)
EM (Electron microscopy)
Signup and view all the flashcards
Minimal Change Disease
Minimal Change Disease
Signup and view all the flashcards
Podocyte Foot Processes
Podocyte Foot Processes
Signup and view all the flashcards
Post-streptococcal Glomerulonephritis
Post-streptococcal Glomerulonephritis
Signup and view all the flashcards
Immune Complex Deposition
Immune Complex Deposition
Signup and view all the flashcards
Subepithelial Immune Complex Deposit
Subepithelial Immune Complex Deposit
Signup and view all the flashcards
Humps
Humps
Signup and view all the flashcards
Nephrotic Syndrome
Nephrotic Syndrome
Signup and view all the flashcards
Podocyte Damage
Podocyte Damage
Signup and view all the flashcards
Hypoalbuminemia
Hypoalbuminemia
Signup and view all the flashcards
Oedema
Oedema
Signup and view all the flashcards
Minimal Change Disease (MCD)
Minimal Change Disease (MCD)
Signup and view all the flashcards
Focal Segmental Glomerulosclerosis
Focal Segmental Glomerulosclerosis
Signup and view all the flashcards
Membranous Nephropathy
Membranous Nephropathy
Signup and view all the flashcards
Secondary Causes of Nephrotic Syndrome
Secondary Causes of Nephrotic Syndrome
Signup and view all the flashcards
Acute Interstitial Nephritis (AIN)
Acute Interstitial Nephritis (AIN)
Signup and view all the flashcards
What characterizes AIN?
What characterizes AIN?
Signup and view all the flashcards
UTI
UTI
Signup and view all the flashcards
Significant bacteriuria
Significant bacteriuria
Signup and view all the flashcards
Cystitis
Cystitis
Signup and view all the flashcards
Non-bacterial Cystitis
Non-bacterial Cystitis
Signup and view all the flashcards
Ureterovesical Junction (UVJ)
Ureterovesical Junction (UVJ)
Signup and view all the flashcards
Clinical features of UTI
Clinical features of UTI
Signup and view all the flashcards
What is CD10?
What is CD10?
Signup and view all the flashcards
What are the common markers for RCC?
What are the common markers for RCC?
Signup and view all the flashcards
What are some negative stains for RCC?
What are some negative stains for RCC?
Signup and view all the flashcards
What are some common sites of RCC metastasis?
What are some common sites of RCC metastasis?
Signup and view all the flashcards
What is a pathological fracture?
What is a pathological fracture?
Signup and view all the flashcards
What is Nephroblastoma?
What is Nephroblastoma?
Signup and view all the flashcards
What is the typical age group for Wilms tumor?
What is the typical age group for Wilms tumor?
Signup and view all the flashcards
What are some common Wilms tumor syndromes?
What are some common Wilms tumor syndromes?
Signup and view all the flashcards
Non-invasive Papillary Urothelial Carcinoma (LGPUC)
Non-invasive Papillary Urothelial Carcinoma (LGPUC)
Signup and view all the flashcards
Non-invasive Papillary Urothelial Carcinoma (HGPUC)
Non-invasive Papillary Urothelial Carcinoma (HGPUC)
Signup and view all the flashcards
What are the differences between LGPUC and HGPUC?
What are the differences between LGPUC and HGPUC?
Signup and view all the flashcards
What is the prognosis of LGPUC?
What is the prognosis of LGPUC?
Signup and view all the flashcards
What is the prognosis of HGPUC?
What is the prognosis of HGPUC?
Signup and view all the flashcards
Urothelial Carcinoma In-Situ (CIS)
Urothelial Carcinoma In-Situ (CIS)
Signup and view all the flashcards
How do you distinguish CIS from LGPUC and HGPUC?
How do you distinguish CIS from LGPUC and HGPUC?
Signup and view all the flashcards
What are the risks associated with CIS?
What are the risks associated with CIS?
Signup and view all the flashcards
Study Notes
Glomerular Diseases
- Glomerular diseases are a group of conditions that damage the glomeruli, the kidney's microscopic filtration units.
- Damage to the glomeruli impairs kidney function, causing issues like proteinuria, hematuria, reduced glomerular filtration rate (GFR), and chronic kidney disease or failure.
- Glomerular diseases can result in significant morbidity and mortality. Complications include hypertension, nephrotic syndrome, and end-stage renal disease, necessitating dialysis or kidney transplantation.
- Early detection and appropriate management are crucial to prevent progression and improve patient outcomes.
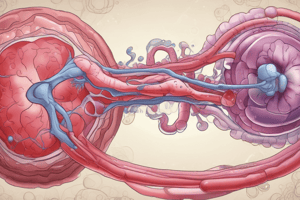
Human Kidney Anatomy
- The kidney has an external and internal view. Diagrams of both are shown. Cortical blood vessels, interlobular blood vessels, renal artery, renal vein, ureter, minor calyx, major calyx, medulla, and capsule are depicted.
Renal Anatomy
- The functional unit of the kidney is the nephron; a diagram is provided. Components include the glomerulus, proximal convoluted tubule, distal convoluted tubule, collecting duct. Blood flow is depicted from renal artery to renal vein.
Glomerulus Structure
- Diagrams illustrating the microscopic structure of the glomerulus are present. Components include capillary loops, red blood cells, proximal tubule, urinary space, mesangium, mesangial cells, mesangial matrix, parietal epithelium, endothelium, foot processes, basement membrane and fenestrae in endothelium. All components are labeled directly.
Classification of Glomerular Diseases
- Primary Glomerular Diseases: affect only the kidneys.
- Minimal change disease (lipoid nephrosis)
- Acute diffuse proliferative GN (post-streptococcal and non-post-streptococcal)
- Rapidly progressive GN
- Membranous GN
- Membranoproliferative GN
- Chronic GN
- Secondary Glomerular Diseases: affect other organs and also affect the kidneys.
- Systemic lupus erythematosus (SLE)
- Polyarteritis nodosa (PAN)
- Wegener granulomatosis
- Diabetes mellitus (diabetic nephropathy)
- Goodpasture syndrome
- Amyloidosis
Minimal Change Glomerular Disease
- Etiology & Pathogenesis: Chemical change in glomerular basement membrane causing protein loss.
- Grossly: Mild bilateral kidney enlargement.
- LM (Light Microscope): No abnormalities.
- IF (Immunofluorescence): No immune deposits.
- EM (Electron Microscope): Fusion of foot processes of epithelial cells (podocytes).
- Clinical Picture (CP): Affects children and young adults; causes nephrotic syndrome.
- Fate: Excellent prognosis; most patients respond to corticosteroids with complete resolution of proteinuria.
Post-streptococcal Glomerular Nephritis
- Etiology & Pathogenesis: Immune complex reaction; nephrogenic strains of group A beta hemolytic streptococci + IgG, complex deposited in glomeruli with subsequent complement activation -> acute inflammation.
- Grossly: Mild bilateral kidney enlargement with petechial hemorrhages.
- LM (Light Microscope):
- Glomeruli: proliferation of endothelial and mesangial cells; glomerular capillaries containing neutrophils; Bowman's space shows neutrophils, RBCs, and some albumin.
- Tubules: lining cells swollen; lumens show casts (RBC casts, neutrophil casts, and hyaline casts).
- Interstitium: acute inflammatory reaction.
- IF (Immunofluorescence): Deposition of IgG and C3.
- EM (Electron Microscope): Subepithelial immune complex deposit (humps)
- Clinical Picture (CP): Young child abruptly develops malaise, fever, nausea, oliguria, and hematuria (smoky or cocoa-colored urine) 1-2 weeks after recovery from a sore throat.
- Fate: More than 95% recover with therapy. The rest may develop rapidly progressive glomerulonephritis or chronic glomerulonephritis. In adults, prognosis is bad.
Diagnosis of Glomerular Diseases
- A renal biopsy is taken and examined using three types of microscopes:
- Light microscope (LM): to examine the structure of glomeruli, tubules, and interstitium.
- Immunofluorescent microscope (IF): to identify the type of deposited immunoglobulin in the glomeruli.
- Electron microscope (EM): to determine the site of immune complexes (sub-epithelial, sub-endothelial, mesangial or basement membrane).
Other Glomerular Diseases (Brief Overviews)
- Presents information on both light and electron microscopy views for various aspects of kidney disease. Includes Membranous glomerulopathy, Membranoproliferative GN (Type 1), Diabetic glomerulosclerosis, Amyloidosis, Anti-GBM disease (Goodpasture's syndrome), IgA nephropathy, Henoch-Schönlein Purpura, SLE, Chronic Glomerulonephritis, and other, more general information.
Nephrotic and Nephritic Syndromes
- Nephrotic Syndrome: formed of: proteinuria (>3.5g/24 hrs), hypoproteinemia (<30g/L), edema, and hypercholesterolemia. Minimal change disease in children and membranous nephropathy in adults are common causes. Potential complications = infections, thromboembolism and hyperlipidaemia.
- Nephritic Syndrome: formed of: hematuria, oliguria, periorbital edema, and hypertension. Post-streptococcal GN is a common cause. Electrolyte imbalances and hypertension may be present possibly because of glomerular damage.
Pyelonephritis and Acute Interstitial Nephritis (AIN)
- Pyelonephritis: Inflammation of the tubules, interstitium, and renal pelvis. Two forms:
- Acute pyelonephritis: Often caused by bacterial infection.
- Chronic pyelonephritis: More complex, infection plays a role, but reflux and obstruction are also factors. Symptoms of acute pyelonephritis: Fever, chills, tachycardia, tachypnea, flank pain, abdominal pain, nausea, vomiting, dysuria, nocturia, symptoms of recent cystitis or UTI treatment. Predisposing factors = Urinary tract obstruction, Instrumentation, Vesicoureteral reflex, Pregnancy, Preexisting renal lesions, Diabetes mellitus and Immunosuppression, possible complications = Papillary necrosis, Pyonephrosis, and Perinephric abscess.
- Acute Interstitial Nephritis (AIN): Inflammatory condition affecting kidney interstitium (area surrounding renal tubules). Causes = Medications (antibiotics, NSAIDs), Infections, Autoimmune Diseases. Histology = Presence of inflammatory cells (lymphocytes, eosinophils, and sometimes plasma cells) within the interstitium, possible damage to tubules and edema.
Lower Urinary Tract Infections
- Urinary Tract Infections (UTIs): Defined by the presence of microorganisms in bladder urine with or without symptoms or renal disease. Factors normally protecting against UTIs: Washing out bacteria, Low pH, High osmolarity, Tamm-Horsfall protein, Ureterovesical junction valve action.
- Cystitis: Inflammation of bladder; two forms:
- Bacterial (acute): common, predisposing factors = bladder calculi, urinary obstruction, diabetes mellitus, instrumentation, immune deficiency.
- Non-bacterial (Interstitial Cystitis): Chronic, non-infectious. Symptoms = Frequency, Urgency, Dysuria, Suprapubic Pain, Cloudy or foul-smelling urine. Etiology includes women, tuberculous cystitis, Candida albicans infections, Schistosomiasis, Chlamydia and Mycoplasma infections.
- Relevant other lower UTI's are also described.
Obstructive Uropathy
- Obstructive uropathy: Functional or anatomic obstruction of urinary tract flow.
- Causes = Calculus, Chronic infection, Pyogenic granulomatous, Ureter anomalies, Stricture stenosis, Neoplasm, Compression, Trauma.
- Location
- Completeness
- Involvement of one or both upper urinary tracts
- Duration
- Cause of any obstruction
- Physiologic view of urine flow.
- Pathophysiology (mechanisms) of obstruction related to causes.
- Lower Urinary Tract Obstruction: Urethral stricture, Prostate enlargement, pelvic organ prolapse, Low bladder wall compliance.
- Neurogenic bladder - Dyssynergia, Detrusor hyperreflexia-overactive, Detrusor areflexia-underactive and Overactive bladder syndrome (OBS) = Frequency, urgency, nocturia.
Urolithiasis (Renal Calculi)
- Definition: Masses of crystals, protein, or other substances forming within and obstructing the urinary tract.
- Types of Renal Stones:
- Calcium oxalate/phosphate (75%)
- Struvite (10-15%)
- Uric acid (6%)
- Cystine (1-2%)
- Unknown (?10%)
- Pathogenesis: Variables related to each type of stone.
- Risk Factors: Increased concentration of stone constituents (changes in urinary pH, low pH higher risk), Decrease in urine volume, and urinary tract infection.
- Sites: Unilateral in 80%; common sites = renal calyces, pelvis; stones can be small (2-3 mm), or large (Staghorn).
- Clinical Presentation: Symptoms may occur from obstruction, ulceration, and subsequent bleeding. Smaller stones = pain, hematuria, recurrent UTI. Asymptomatic can occur.
- Laboratory Diagnosis:
- UEC (Urinalysis shows hematuria, crystals, and pyuria).
- BUN
- Other modes of investigation = USS, X-rays, CT scans.
- Prognosis: Generally good; depends on the underlying cause.
Renal Tumors
-
Renal Cell Carcinoma: Most common malignant tumor. Epidemiology = Affects adults, 6th/7th decade. Risk factors = smoking, obesity, HTN, exposure to chemicals, estrogen therapy and secondary to dialysis. Clinical presentation = Silent, hematuria, flank pain.
-
Renal Oncocytoma: Rare, benign tumor. Epidemiology = More common in men. Clinical presentation = Asymptomatic, flank pain, and hematuria.
-
Nephroblastoma (Wilms Tumor): Malignant embryonal tumor occurring in children; common in 3-4 year-old children. Etiology = Genetic alterations. Clinical presentation = Abdominal mass, with sometimes associated pain/hematuria.
- Associated syndromes = WAGR, Denys-Drash, Beckwith-Wiedemann
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.