Podcast
Questions and Answers
What is the definition of atmospheric pressure according to the presentation?
What is the definition of atmospheric pressure according to the presentation?
- The contribution of one gas in a mixture.
- The pressure gradient that causes gases to travel.
- The sum of the pressures exerted by all gases in a mixture. (correct)
- The pressure exerted by a single gas at sea level.
According to Dalton's Law, what determines the partial pressure of a gas in a mixture?
According to Dalton's Law, what determines the partial pressure of a gas in a mixture?
- The contribution of that individual gas to the total pressure. (correct)
- The atmospheric pressure at sea level.
- The gas's molecular weight relative to other gases.
- The pressure gradient of all gases combined.
At sea level, what is the approximate partial pressure ($PO_2$) of oxygen, given that it constitutes 20.9% of the atmospheric pressure?
At sea level, what is the approximate partial pressure ($PO_2$) of oxygen, given that it constitutes 20.9% of the atmospheric pressure?
- 159 mm Hg (correct)
- 597 mm Hg
- 20.9 mm Hg
- 760 mm Hg
How does altitude affect atmospheric pressure and the partial pressure of oxygen?
How does altitude affect atmospheric pressure and the partial pressure of oxygen?
What condition must be met for oxygen to diffuse from the alveolar air into the blood?
What condition must be met for oxygen to diffuse from the alveolar air into the blood?
In alveolar gas exchange, what is the relationship between the partial pressure of gases and their movement across the respiratory membrane?
In alveolar gas exchange, what is the relationship between the partial pressure of gases and their movement across the respiratory membrane?
Why is it essential for oxygen to dissolve in the water film lining the alveoli?
Why is it essential for oxygen to dissolve in the water film lining the alveoli?
Which of the following is true regarding the partial pressures of oxygen ($O_2$) and carbon dioxide ($CO_2$) in the alveoli compared to the blood entering the lungs?
Which of the following is true regarding the partial pressures of oxygen ($O_2$) and carbon dioxide ($CO_2$) in the alveoli compared to the blood entering the lungs?
What is the primary function of the pulmonary circuit?
What is the primary function of the pulmonary circuit?
What factors affect the efficiency of gas exchange in the lungs?
What factors affect the efficiency of gas exchange in the lungs?
Why is carbon dioxide ($CO_2$) more soluble in water than oxygen ($O_2$)?
Why is carbon dioxide ($CO_2$) more soluble in water than oxygen ($O_2$)?
How does membrane thickness affect gas exchange?
How does membrane thickness affect gas exchange?
What is the role of carbonic anhydrase in red blood cells (RBCs) during gas exchange?
What is the role of carbonic anhydrase in red blood cells (RBCs) during gas exchange?
What happens to most of the carbon dioxide that enters red blood cells?
What happens to most of the carbon dioxide that enters red blood cells?
What is the 'chloride shift' that occurs in red blood cells, and why is it important?
What is the 'chloride shift' that occurs in red blood cells, and why is it important?
In the pulmonary capillaries, what changes occur to facilitate the unloading of $CO_2$ and the loading of $O_2$?
In the pulmonary capillaries, what changes occur to facilitate the unloading of $CO_2$ and the loading of $O_2$?
What is the sequence of blood flow through the pulmonary circuit starting from deoxygenated blood entering the heart?
What is the sequence of blood flow through the pulmonary circuit starting from deoxygenated blood entering the heart?
Which of the following represents the correct order of events in the systemic circuit, starting with oxygenated blood leaving the lungs?
Which of the following represents the correct order of events in the systemic circuit, starting with oxygenated blood leaving the lungs?
Ventilation-perfusion coupling is essential for efficient gas exchange. How does local vasoconstriction in the lungs contribute to this coupling?
Ventilation-perfusion coupling is essential for efficient gas exchange. How does local vasoconstriction in the lungs contribute to this coupling?
In a scenario where an individual is at high altitude, which compensatory mechanism would the body primarily employ to facilitate oxygen delivery to tissues?
In a scenario where an individual is at high altitude, which compensatory mechanism would the body primarily employ to facilitate oxygen delivery to tissues?
What is the significance of the water film on the surface of the alveolar epithelium in the context of gas exchange?
What is the significance of the water film on the surface of the alveolar epithelium in the context of gas exchange?
In the context of alveolar gas exchange, what is the role of the relatively low concentration of protein within the interstitial fluid that surrounds the alveoli?
In the context of alveolar gas exchange, what is the role of the relatively low concentration of protein within the interstitial fluid that surrounds the alveoli?
How does the process of oxygen unloading at the systemic capillaries facilitate the return of carbon dioxide to the lungs?
How does the process of oxygen unloading at the systemic capillaries facilitate the return of carbon dioxide to the lungs?
Upon reaching the alveoli, how is the process of oxygen uptake influenced by the affinity of hemoglobin and the surrounding conditions?
Upon reaching the alveoli, how is the process of oxygen uptake influenced by the affinity of hemoglobin and the surrounding conditions?
Which specific characteristic of the alveolar type I cells directly facilitates efficient gas exchange?
Which specific characteristic of the alveolar type I cells directly facilitates efficient gas exchange?
Consider a scenario where a patient exhibits impaired diffusion due to alveolar thickening from pulmonary fibrosis. Which of the following compensatory mechanisms is most likely to initially improve gas exchange efficiency?
Consider a scenario where a patient exhibits impaired diffusion due to alveolar thickening from pulmonary fibrosis. Which of the following compensatory mechanisms is most likely to initially improve gas exchange efficiency?
If a patient is diagnosed with a pulmonary embolism that blocks blood flow to a segment of the lung, how would the local alveolar environment respond to maintain efficient ventilation-perfusion matching?
If a patient is diagnosed with a pulmonary embolism that blocks blood flow to a segment of the lung, how would the local alveolar environment respond to maintain efficient ventilation-perfusion matching?
In the context of extreme physical exertion, indicate the most immediate physiological response that optimizes oxygen supply to skeletal muscles.
In the context of extreme physical exertion, indicate the most immediate physiological response that optimizes oxygen supply to skeletal muscles.
Considering pulmonary hypertension's effects on pulmonary capillary dynamics, which of the following adaptations would likely occur to maintain gas exchange in affected individuals?
Considering pulmonary hypertension's effects on pulmonary capillary dynamics, which of the following adaptations would likely occur to maintain gas exchange in affected individuals?
If an individual with chronic bronchitis develops hypoxemia, which of the following is the most likely underlying cause?
If an individual with chronic bronchitis develops hypoxemia, which of the following is the most likely underlying cause?
Given a patient with a significantly decreased level of carbonic anhydrase, which of the following blood gas parameters would you expect to see altered most significantly?
Given a patient with a significantly decreased level of carbonic anhydrase, which of the following blood gas parameters would you expect to see altered most significantly?
How might the presence of significant scar tissue or fibrosis within the lungs primarily compromise gas exchange efficiency?
How might the presence of significant scar tissue or fibrosis within the lungs primarily compromise gas exchange efficiency?
A mountain climber ascends rapidly to a very high altitude. How would this sudden change in altitude likely affect the climber's alveolar and arterial oxygen levels immediately?
A mountain climber ascends rapidly to a very high altitude. How would this sudden change in altitude likely affect the climber's alveolar and arterial oxygen levels immediately?
Under conditions of hypothermia, how is the oxygen-hemoglobin dissociation curve affected, and what is the result on oxygen delivery?
Under conditions of hypothermia, how is the oxygen-hemoglobin dissociation curve affected, and what is the result on oxygen delivery?
If a doctor injects a medication that causes bronchodilation, it is likely that?
If a doctor injects a medication that causes bronchodilation, it is likely that?
A person has lost a significant amount of blood. How would this impact gas exchange?
A person has lost a significant amount of blood. How would this impact gas exchange?
The rate of diffusion of a gas across a permeable membrane is NOT affected by
The rate of diffusion of a gas across a permeable membrane is NOT affected by
Flashcards
Atmospheric Pressure
Atmospheric Pressure
The sum of the pressures exerted by each gas in a gaseous mixture.
Partial Pressure
Partial Pressure
The pressure exerted by a single gas in a mixture of gases.
Gas Pressure Gradient
Gas Pressure Gradient
Gases move from areas of high concentration to low concentration.
Alveolar Gas Exchange
Alveolar Gas Exchange
Signup and view all the flashcards
Water Film on Alveoli
Water Film on Alveoli
Signup and view all the flashcards
Partial pressure & diffusion
Partial pressure & diffusion
Signup and view all the flashcards
Anastomosis
Anastomosis
Signup and view all the flashcards
High O2 in lungs
High O2 in lungs
Signup and view all the flashcards
Solubility of Gases in Alveoli
Solubility of Gases in Alveoli
Signup and view all the flashcards
Pulmonary Circulation
Pulmonary Circulation
Signup and view all the flashcards
Pulmonary Artery
Pulmonary Artery
Signup and view all the flashcards
Pulmonary vein
Pulmonary vein
Signup and view all the flashcards
Right atrium
Right atrium
Signup and view all the flashcards
The creation of Bicarbonate
The creation of Bicarbonate
Signup and view all the flashcards
Study Notes
- Gas exchange and pulmonary circulation are key components of the respiratory system.
Partial Pressure
- The atmospheric pressure refers to the sum of the pressure of all the gases in a mixture.
- Dalton's Law states that partial pressure is the pressure contributed by a single gas.
- At sea level, atmospheric pressure is 760 mm Hg.
- Oxygen constitutes 20.9% of atmospheric pressure, with a partial pressure of 159 mm Hg.
- Gases travel down a pressure gradient.
- Atmospheric pressure is affected by altitude, decreasing as altitude increases
- Altitude impacts the pressure gradients in the body.
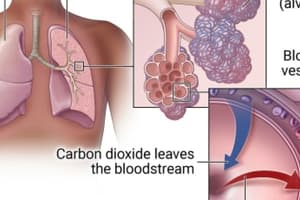
Alveolar Gas Exchange
- A water film lines the lumen of the epithelium found on the surface of the alveoli.
- Oxygen must be dissolved to enter tissues and blood.
- Oxygen moves from alveolar air across the water film, through the respiratory membrane, and into the blood.
- Partial pressure must be greater in water than in the gases for diffusion to occur.
Efficiency of Gas Exchange
- Gas Exchange depends on:
- Pressure gradients.
- Gas solubility, which is higher in carbon dioxide than in oxygen.
- Membrane thickness.
- Membrane area.
- An example of an issue with the membrane area is emphysema.
- Efficiency is dependent on ventilation-perfusion coupling to ensure blood flow matches oxygen supply.
- Low oxygen levels cause vasoconstriction, and high oxygen levels allow vasodilation.
Gas Exchange
- The alveoli consist of thin, simple squamous cells.
- Blood vessels surround the alveoli.
Inspiration
- There is high oxygen and low carbon dioxide in the alveoli.
- Conversely, blood returning to the lungs has low oxygen and high carbon dioxide.
- Oxygen diffuses from air through water, then through the epithelium into the blood.
- Oxygen enters red blood cells and binds to hemoglobin for transport to other body tissues.
- Once blood reaches tissues, oxygen concentration is high.
- Many tissues aerobically metabolize using oxygen, producing carbon dioxide and water.
- Blood has high oxygen levels, while tissues have low oxygen levels.
- Similarly, blood has low carbon dioxide levels, while tissues have high carbon dioxide levels.
- Oxygen unbinds from hemoglobin and diffuses into tissue cells.
- Carbon dioxide enters red blood cells and binds to hemoglobin.
- In red blood cells, carbon dioxide and water form carbonic acid, which dissociates into hydrogen ions and bicarbonate.
- Carbonic anhydrase is key to this enzymatic reaction.
- Bicarbonate leaves the red blood cells by acting as chloride.
Oxygen Release
- Once back in the lungs, the blood is colder.
- The alveoli have high oxygen, while the blood has low oxygen.
- In contrast, alveoli have low carbon dioxide, while blood has high carbon dioxide.
- Bicarbonate re-enters red blood cells, while chloride leaves.
- The equation reverses to reform carbon dioxide and water.
- Carbon dioxide leaves red blood cells, diffuses out of blood, and is exhaled.
- Oxygen diffuses from alveoli into the blood approximately 3 times per minute.
Pulmonary Circulation
- Deoxygenated blood enters the heart through the right atrium via the superior vena cava, inferior vena cava, and coronary sinus.
- The atria contract, moving blood to the right ventricle.
- The ventricles contract, moving blood up the pulmonary trunk, then through the pulmonary arteries to the lungs.
- From the lungs, blood moves via pulmonary veins to the left atrium.
- The left atrium contracts, moving blood to the left ventricle and then the aorta.
- The aorta facilitates systemic and coronary circulation.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.