Podcast
Questions and Answers
What type of fracture allows for normal movement greater than 50% of the normal range and remains stable upon reduction?
What type of fracture allows for normal movement greater than 50% of the normal range and remains stable upon reduction?
- Undisplaced fracture (correct)
- Complete transverse translation
- Comminuted fracture
- Oblique fracture
Which fracture type is kept apart by muscle pull, making it unstable?
Which fracture type is kept apart by muscle pull, making it unstable?
- Avulsion fracture (correct)
- Undisplaced fracture
- Complete fracture
- Comminuted fracture
Which type of fracture requires complex splinting due to translational or rotational displacement?
Which type of fracture requires complex splinting due to translational or rotational displacement?
- Stable fracture
- Avulsion fracture
- Oblique/spiral fracture (correct)
- Incomplete fracture
What classification is used to describe the location of a diaphyseal fracture?
What classification is used to describe the location of a diaphyseal fracture?
What is the primary characteristic of complete transverse translation fractures?
What is the primary characteristic of complete transverse translation fractures?
What largely characterizes metaphyseal fractures compared to diaphyseal fractures?
What largely characterizes metaphyseal fractures compared to diaphyseal fractures?
What is the primary mechanism causing oblique fractures?
What is the primary mechanism causing oblique fractures?
What is a common management strategy for extra-articular metaphyseal fractures with minimal displacement?
What is a common management strategy for extra-articular metaphyseal fractures with minimal displacement?
What is the typical timeline for metaphyseal fracture consolidation?
What is the typical timeline for metaphyseal fracture consolidation?
Which statement about the healing process of metaphyseal fractures is accurate?
Which statement about the healing process of metaphyseal fractures is accurate?
What is the recommended treatment for a posterior sternoclavicular dislocation?
What is the recommended treatment for a posterior sternoclavicular dislocation?
What is the primary concern with a posterior sternoclavicular dislocation?
What is the primary concern with a posterior sternoclavicular dislocation?
In the case of a Monteggia fracture, what is the standard treatment approach?
In the case of a Monteggia fracture, what is the standard treatment approach?
What is the typical management for recurrent shoulder dislocations?
What is the typical management for recurrent shoulder dislocations?
What is a key characteristic of anterior shoulder dislocations?
What is a key characteristic of anterior shoulder dislocations?
What is the primary objective of reduction in operative procedures?
What is the primary objective of reduction in operative procedures?
Which condition is NOT contraindicated for operative intervention?
Which condition is NOT contraindicated for operative intervention?
What is the main purpose of stabilization after reduction?
What is the main purpose of stabilization after reduction?
Which scenario indicates the use of operative fixation?
Which scenario indicates the use of operative fixation?
Which method of reduction is preferred when attempting to avoid damage to the blood supply?
Which method of reduction is preferred when attempting to avoid damage to the blood supply?
What is one reason closed reduction may be challenging in babies?
What is one reason closed reduction may be challenging in babies?
What is a common misconception about intra-articular fractures when performing reduction?
What is a common misconception about intra-articular fractures when performing reduction?
Which of the following is NOT a method of reduction?
Which of the following is NOT a method of reduction?
What type of treatment is recommended for a femur shaft fracture with nerve palsy?
What type of treatment is recommended for a femur shaft fracture with nerve palsy?
Which option is indicated when dealing with a femoral neck and proximal shaft fracture?
Which option is indicated when dealing with a femoral neck and proximal shaft fracture?
What is the suggested approach for treating a metastatic fracture?
What is the suggested approach for treating a metastatic fracture?
What complication is associated with femoral shaft or tibial fractures that necessitates immediate concern?
What complication is associated with femoral shaft or tibial fractures that necessitates immediate concern?
Which treatment option is appropriate for a comminuted open fracture classified as IIIB or IIIC?
Which treatment option is appropriate for a comminuted open fracture classified as IIIB or IIIC?
What intervention is necessary to address knee stiffness after a knee injury?
What intervention is necessary to address knee stiffness after a knee injury?
What is a potential consequence of delayed treatment for femoral shaft fractures?
What is a potential consequence of delayed treatment for femoral shaft fractures?
The appropriate treatment for a supracondylar fracture in children is typically?
The appropriate treatment for a supracondylar fracture in children is typically?
Flashcards are hidden until you start studying
Study Notes
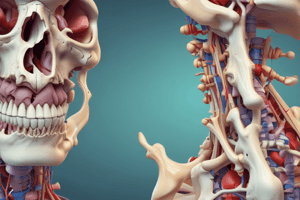
General Principles
- Causes of fractures: Trauma, overuse, and underlying medical conditions
- Mechanisms of fractures: Direct impact, twisting, bending, or pulling forces
- Assessing injury: History, physical examination, and imaging
- Fracture emergencies: Open fracture, vascular injury, nerve injury, compartment syndrome
- Metaphyseal vs Diaphyseal Fractures:
- Metaphyseal fracture: Located in the end of a bone near a growth plate (epiphyseal plate)
- Healing: Occurs by bone ingrowth with little motion
- Movement: Limited as the metaphysis has lots of cancellous bone (spongy bone)
- Rapid Repair: Fracture consolidates in 3 weeks
Stability of Fractures
- Stable Fracture: Stays reduced with simple splintage, allowing good movement
- Unstable Fracture: Requires complex splinting to reduce and hold, as fragments translate/rotate
- Types of fractures:
- Oblique/spiral: Unstable due to translational/rotational displacement
- Avulsion: Unstable due to muscle pull keeping fragments separate
- Complete transverse translation: Unstable, may require operative or non-operative treatment
Treatment of Fractures
- Non-operative treatment: Analgesia, splints, protection, restoration of function
- Operative treatment: Reduction, fixation, arthroplasty, amputation
- Contraindications to operative treatment: Severe osteoporosis, active infection, severe comminution, severe soft tissue injury, poor general condition, undisplaced fracture
- Objectives of treatment: Restore function, prevent osteoarthritis
Reduction of Fractures
- Objective: Adequate apposition (touching) and normal alignment of fracture ends
- Imperfect apposition (touching) is sometimes acceptable, but imperfect alignment rarely is
- Methods: Manipulation, mechanical traction, open reduction
- Closed Reduction:
- Minimizes damage to soft tissue
- Relies on soft tissue attachments
- Rarely adequate for intra-articular fractures
- Difficult in infants whose bones are hard to visualize on X-ray
- Contraindications:
- Little or no displacement
- Displacement does not matter (e.g. clavicle, fibula)
- Reduction unlikely to succeed (e.g. compressed vertebral fracture)
Specific Fracture Examples
- Shoulder dislocation:
- Anterior: Conservative treatment
- Posterior: Operative ORIF
- Monteggia's: ORIF (Ulnar plating, reduce radial head), long arm cast at 90 degrees flexion
- Galeazzi's: ORIF (Radial plating, reduce ulnar head), long arm cast in supination
- Femur shaft fracture:
- Traction to overcome pull of quadriceps and hamstrings
- Intra-medullary nail
- Alternatives: External fixation (Ilizarov), plating
- Femur supracondylar, unicondylar, T and Y condylar fractures:
- Children: Plaster
- Other cases: Internal fixation for good reduction with early mobilization
Complications of Fractures
- Hypovolemic shock
- Fat embolism
- Delayed union, non-union
- Mal-union
- Limb shortening
- Knee stiffness
- Infection
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.