Podcast
Questions and Answers
Which of the following is the most variable component of Total Energy Expenditure (TEE)?
Which of the following is the most variable component of Total Energy Expenditure (TEE)?
- Basal Metabolic Rate (BMR)
- Resting Energy Expenditure (REE)
- Physical activity (correct)
- Diet-Induced Thermogenesis (DIT)
What is the approximate contribution of Basal Metabolic Rate (BMR) to Total Energy Expenditure (TEE) in most individuals?
What is the approximate contribution of Basal Metabolic Rate (BMR) to Total Energy Expenditure (TEE) in most individuals?
- 60-70% (correct)
- 80-90%
- 40-50%
- 25-35%
Which factor has the greatest effect on diet-induced thermogenesis?
Which factor has the greatest effect on diet-induced thermogenesis?
- Protein (correct)
- Fiber
- Fat
- CHO
Which condition is NOT essential for accurately measuring Basal Metabolic Rate (BMR)?
Which condition is NOT essential for accurately measuring Basal Metabolic Rate (BMR)?
If conditions for measuring BMR are not fully met, what is the measurement properly termed?
If conditions for measuring BMR are not fully met, what is the measurement properly termed?
Which set of organs contributes the most to BMR, despite their small percentage of body weight?
Which set of organs contributes the most to BMR, despite their small percentage of body weight?
In a healthy individual, what is the approximate contribution of physical activity to total energy expenditure?
In a healthy individual, what is the approximate contribution of physical activity to total energy expenditure?
Which of the following methods measures total energy expenditure (TEE) over a period of several weeks?
Which of the following methods measures total energy expenditure (TEE) over a period of several weeks?
What is a key principle underlying the PENG guidelines (2011) for estimating BMR in individuals with illness?
What is a key principle underlying the PENG guidelines (2011) for estimating BMR in individuals with illness?
Within the PENG guidelines, what adjustments should be made after estimating BMR using the Henry equation?
Within the PENG guidelines, what adjustments should be made after estimating BMR using the Henry equation?
The Harris-Benedict equations were developed using data from which patient population?
The Harris-Benedict equations were developed using data from which patient population?
A key limitation of the Harris-Benedict equations related to BMR estimation is that they:
A key limitation of the Harris-Benedict equations related to BMR estimation is that they:
What specific factor is incorporated in the Harris-Benedict equation for calculating basal energy expenditure?
What specific factor is incorporated in the Harris-Benedict equation for calculating basal energy expenditure?
The Schofield equations for estimating BMR are based on:
The Schofield equations for estimating BMR are based on:
The Schofield equations are considered unreliable for estimating BMR in:
The Schofield equations are considered unreliable for estimating BMR in:
What is a major limitation of using BMR equations like Schofield for estimating energy requirements in sick individuals?
What is a major limitation of using BMR equations like Schofield for estimating energy requirements in sick individuals?
Which consideration is particularly important when using weight in BMR calculations?
Which consideration is particularly important when using weight in BMR calculations?
What is a common 'rule-of-thumb' range for estimating energy needs using body weight in kcal/kg?
What is a common 'rule-of-thumb' range for estimating energy needs using body weight in kcal/kg?
What is a primary limitation of using 'rule-of-thumb' formulas for estimating energy requirements?
What is a primary limitation of using 'rule-of-thumb' formulas for estimating energy requirements?
In clinical practice, what is one major consideration when adjusting energy requirements for individuals with amputations?
In clinical practice, what is one major consideration when adjusting energy requirements for individuals with amputations?
What is the purpose of using 'adjusted' body weight in BMR calculations for obese patients?
What is the purpose of using 'adjusted' body weight in BMR calculations for obese patients?
According to ESPEN guidelines, what is used in addition to the ideal body weight when estimating energy requirements for obese individuals?
According to ESPEN guidelines, what is used in addition to the ideal body weight when estimating energy requirements for obese individuals?
What is a significant concern associated with overfeeding, especially with excess carbohydrates?
What is a significant concern associated with overfeeding, especially with excess carbohydrates?
What is a key strategy for managing re-feeding syndrome in malnourished patients?
What is a key strategy for managing re-feeding syndrome in malnourished patients?
Why is it necessary to have dietary protein?
Why is it necessary to have dietary protein?
What conditions are the requirements for protein increased?
What conditions are the requirements for protein increased?
Which of the following can interfere with the accurate measurement of nitrogen balance?
Which of the following can interfere with the accurate measurement of nitrogen balance?
The classification of this dietary need is not essential, but is derived from the metabolism of an aa or nitrogenous metabolite.
The classification of this dietary need is not essential, but is derived from the metabolism of an aa or nitrogenous metabolite.
Which value is the recommended nutrient intake(RNI) for protein in adults?
Which value is the recommended nutrient intake(RNI) for protein in adults?
What is the generally recommended fluid intake for adults aged 18-60 if taking oral fluids?
What is the generally recommended fluid intake for adults aged 18-60 if taking oral fluids?
A patient has a fever, for each rise in body temperature (°C) above 37°C, what addition fluid is recommended?
A patient has a fever, for each rise in body temperature (°C) above 37°C, what addition fluid is recommended?
What is the daily recommendation for administering sodium via intravenous infusion?
What is the daily recommendation for administering sodium via intravenous infusion?
Blood measurements for this category are not reliable markers of status.
Blood measurements for this category are not reliable markers of status.
According to the slide, what types of patients might demonstrate particularly low energy requirements?
According to the slide, what types of patients might demonstrate particularly low energy requirements?
Generally, in patients categorized as hypermetabolic, what percentage above BMR is indicated?
Generally, in patients categorized as hypermetabolic, what percentage above BMR is indicated?
When is a combined factor of activity and diet-induced thermogenesis added when calculating a patient's energy requirements?
When is a combined factor of activity and diet-induced thermogenesis added when calculating a patient's energy requirements?
When assessing nutritional needs, what is the correct order of the steps?
When assessing nutritional needs, what is the correct order of the steps?
Which of the following is the primary purpose of comparing and contrasting predictive equations for calculating energy requirements?
Which of the following is the primary purpose of comparing and contrasting predictive equations for calculating energy requirements?
In clinical nutrition, what is the main advantage of using Resting Energy Expenditure (REE) over Basal Metabolic Rate (BMR)?
In clinical nutrition, what is the main advantage of using Resting Energy Expenditure (REE) over Basal Metabolic Rate (BMR)?
The differences in metabolically active organs and tissues refers to which component within TEE?
The differences in metabolically active organs and tissues refers to which component within TEE?
If a patient does not adhere to any of the conditions essential for accuratley measuring BMR, how is it properly termed?
If a patient does not adhere to any of the conditions essential for accuratley measuring BMR, how is it properly termed?
What is a practical implication of the finding that metabolically active organs contribute disproportionately to BMR?
What is a practical implication of the finding that metabolically active organs contribute disproportionately to BMR?
In what scenario might the energy expenditure related to physical activity be higher in a hospitalized patient, compared to a healthy individual?
In what scenario might the energy expenditure related to physical activity be higher in a hospitalized patient, compared to a healthy individual?
What is a key difference in how energy expenditure is typically measured using indirect calorimetry versus the doubly-labeled water technique?
What is a key difference in how energy expenditure is typically measured using indirect calorimetry versus the doubly-labeled water technique?
What factor makes accelerometers and multi-sensor monitors suitable for assessing energy expenditure?
What factor makes accelerometers and multi-sensor monitors suitable for assessing energy expenditure?
What modification to the initial BMR estimation is recommended by the PENG guidelines?
What modification to the initial BMR estimation is recommended by the PENG guidelines?
Which of the following statements accurately describes a limitation of using regression equations such as Ireton-Jones (2002) for estimating energy requirements?
Which of the following statements accurately describes a limitation of using regression equations such as Ireton-Jones (2002) for estimating energy requirements?
What is the primary issue with using a 'rule-of-thumb' approach (e.g., kcal/kg body weight) to estimate energy requirements in a clinical setting?
What is the primary issue with using a 'rule-of-thumb' approach (e.g., kcal/kg body weight) to estimate energy requirements in a clinical setting?
Which factor should be carefully considered when estimating energy requirements for an individual with significant edema or ascites?
Which factor should be carefully considered when estimating energy requirements for an individual with significant edema or ascites?
When calculating BMR for amputees, what is the most important consideration related to body weight?
When calculating BMR for amputees, what is the most important consideration related to body weight?
According to ESPEN guidelines for estimating energy requirements in obese individuals, what adjustment is made to the ideal body weight?
According to ESPEN guidelines for estimating energy requirements in obese individuals, what adjustment is made to the ideal body weight?
Which of these statements reflects a key concept regarding energy requirements in obese individuals?
Which of these statements reflects a key concept regarding energy requirements in obese individuals?
What is the primary concern regarding the long-term, excessive provision of carbohydrates in nutritional support?
What is the primary concern regarding the long-term, excessive provision of carbohydrates in nutritional support?
What is the underlying principle for addressing protein needs when energy intake is inadequate?
What is the underlying principle for addressing protein needs when energy intake is inadequate?
Conditionally essential amino acids are essential under which condition?
Conditionally essential amino acids are essential under which condition?
What does the Dietary Reference Value use to determine BMR?
What does the Dietary Reference Value use to determine BMR?
What is the primary concern regarding using the Harris-Benedict equations for estimating energy expenditure in contemporary clinical practice?
What is the primary concern regarding using the Harris-Benedict equations for estimating energy expenditure in contemporary clinical practice?
A key inclusion criterion for studies when developing the Henry equations (2005) was:
A key inclusion criterion for studies when developing the Henry equations (2005) was:
What is the most important reason to use 'dry' weight when estimating energy needs for BMR calculations?
What is the most important reason to use 'dry' weight when estimating energy needs for BMR calculations?
What is a key point of difference between the Schofield and Henry equations?
What is a key point of difference between the Schofield and Henry equations?
Which set of patients might show particularly low energy requirements?
Which set of patients might show particularly low energy requirements?
According to the WHO, what are the levels that the RNI should meet?
According to the WHO, what are the levels that the RNI should meet?
Which parameter requires close consideration when adjusting for clinical condition?
Which parameter requires close consideration when adjusting for clinical condition?
When should increased energy stores be required?
When should increased energy stores be required?
Why do ill requirements have increased requirements for micronutrients?
Why do ill requirements have increased requirements for micronutrients?
What is a common sign in a metabolically stressed patient?
What is a common sign in a metabolically stressed patient?
How is protein used in the body?
How is protein used in the body?
What range is the normal ammount if administering Sodium via IV?
What range is the normal ammount if administering Sodium via IV?
What type of measure should be made for a person if assessing the adequacy of intake?
What type of measure should be made for a person if assessing the adequacy of intake?
What is the purpose of integrating data from multiple sources when assessing micronutrient adequacy?
What is the purpose of integrating data from multiple sources when assessing micronutrient adequacy?
What is the major factor that differentiates the Henry equations from the Schofield equations?
What is the major factor that differentiates the Henry equations from the Schofield equations?
Which group of equations estimates BMR specifically for ventilator-dependent patients?
Which group of equations estimates BMR specifically for ventilator-dependent patients?
What adjustment to overall energy predictions in nutrition is recommended by PENG guidelines?
What adjustment to overall energy predictions in nutrition is recommended by PENG guidelines?
What factor may result in inaccurate weight measurements and introduce error in basal metabolic rate calculations?
What factor may result in inaccurate weight measurements and introduce error in basal metabolic rate calculations?
When is measuring REE most appropriate?
When is measuring REE most appropriate?
In clinical practice, what can affect the amount of nutritional support that is required?
In clinical practice, what can affect the amount of nutritional support that is required?
In devising nutritional support for a patient struggling with anorexia and showing inflammation, what is the most important goal?
In devising nutritional support for a patient struggling with anorexia and showing inflammation, what is the most important goal?
What parameter contributes to the greatest level of variance when estimating total energy expenditure (TEE)?
What parameter contributes to the greatest level of variance when estimating total energy expenditure (TEE)?
The most appropriate method for estimating the energy requirements for an overweight patient who has a BMI over 30 is:
The most appropriate method for estimating the energy requirements for an overweight patient who has a BMI over 30 is:
When should the clinician develop an evidence-based approach?
When should the clinician develop an evidence-based approach?
When would it be most appropriate to prescribe >0.2g of Nitrogen/kg?
When would it be most appropriate to prescribe >0.2g of Nitrogen/kg?
When estimating BMR, which of these factors could influence the validity of the result?
When estimating BMR, which of these factors could influence the validity of the result?
What is the main determinant of diet-induced thermogenesis (DIT)?
What is the main determinant of diet-induced thermogenesis (DIT)?
When estimating the BMR for an amputee, which factors are important?
When estimating the BMR for an amputee, which factors are important?
RNI for protein in healthy adults is
RNI for protein in healthy adults is
How is a stress factor identified?
How is a stress factor identified?
When must amino acids be supplied in the diet?
When must amino acids be supplied in the diet?
Requirements differ in health due to differences in
Requirements differ in health due to differences in
When should weight loss not be the goal?
When should weight loss not be the goal?
Flashcards
Energy Requirements
Energy Requirements
The amount of energy an individual needs to meet their daily energy expenditure and maintain a healthy weight range.
Basal Metabolic Rate (BMR)
Basal Metabolic Rate (BMR)
The rate of energy expenditure measured under specific, very restrictive conditions, including after a 12-hour fast and complete rest.
Resting Metabolic Rate (RMR)
Resting Metabolic Rate (RMR)
The rate of energy expenditure measured under less restrictive conditions than BMR; typically measured after a shorter fasting period and during relaxed rest.
Resting Energy Expenditure (REE)
Resting Energy Expenditure (REE)
Signup and view all the flashcards
Total Energy Expenditure (TEE)
Total Energy Expenditure (TEE)
Signup and view all the flashcards
Diet Induced Thermogenesis (DIT)
Diet Induced Thermogenesis (DIT)
Signup and view all the flashcards
BMR Predictive Equations
BMR Predictive Equations
Signup and view all the flashcards
Indirect Calorimetry
Indirect Calorimetry
Signup and view all the flashcards
PENG Guidelines (2011)
PENG Guidelines (2011)
Signup and view all the flashcards
Harris-Benedict Equation
Harris-Benedict Equation
Signup and view all the flashcards
Schofield Equations (1985)
Schofield Equations (1985)
Signup and view all the flashcards
Rule-of-Thumb Formulae
Rule-of-Thumb Formulae
Signup and view all the flashcards
Stress Factors
Stress Factors
Signup and view all the flashcards
Physical Activity Level (PAL)
Physical Activity Level (PAL)
Signup and view all the flashcards
Amino Acid Requirements
Amino Acid Requirements
Signup and view all the flashcards
Nitrogen Balance
Nitrogen Balance
Signup and view all the flashcards
Refeeding Syndrome
Refeeding Syndrome
Signup and view all the flashcards
Weight in BMR: Obesity
Weight in BMR: Obesity
Signup and view all the flashcards
Guidelines
Guidelines
Signup and view all the flashcards
Study Notes
- Energy requirements estimation plays a vital role in nutritional management in clinical practice.
Model and Process
- Nutritional Screening
- Nutritional assessment (ABCDEF)
- Setting Aims and Objectives
- Estimating Requirements
- Planning and Delivering Intervention
- Monitoring patient
- Evaluating Outcomes
Objectives of Estimating Energy Expenditure: Predictive Equations
- Compare and contrast predictive equations to calculate energy requirements.
- Discuss the strengths and drawbacks of various predictive equations used in clinical practice.
- Describe the role of indirect calorimetry (IC) in assessing energy expenditure.
Terminology Review
- Basal Metabolic Rate (BMR)
- Resting Metabolic Rate (RMR)
- Resting Energy Expenditure (REE)
- Estimated Energy Expenditure (EEE)
- Total Energy Expenditure (TEE)
Components of Total Energy Expenditure (TEE)
- Physical activity is the most variable component of TEE, accounting for 25-50% and rarely exceeding 75%.
- Basal Metabolic Rate (BMR) accounts for 60-70% of TEE and is highly reproducible in individuals.
- BMR varies by 5-10% among individuals due to height, weight, body composition, metabolically active organs and tissues, thyroid function, and circadian rhythms.
- Diet-induced thermogenesis (DIT) contributes approximately 10% to TEE, with protein having a greater effect than fat or carbohydrates.
- For measuring BMR, conditions include a 12-hour fast, physical and mental rest, a thermo-neutral environment (27–29°C), and no tea, coffee, nicotine, or alcohol in the previous 12 hours. Furthermore, there should be no heavy physical activity on the previous day. Gases must be calibrated, and steady-state should be established within about 30 minutes.
- Any deviation from the BMR measuring conditions results in measuring Resting Energy Expenditure (REE).
- Liver, brain, heart, and kidney make up 6% of body weight but contribute to 60-70% of BMR. While skeletal muscle makes up 40% of body weight, it only accounts for 18% of BMR.
- In healthy individuals, BMR represents 60-70%, physical activity 20-40%, and diet-induced thermogenesis around ~10% of the total energy expenditure.
- For an individual with illness or disease, BMR and disease process account for 75-90% and physical activity and diet-induced thermogenesis contributes 10-25%.
- Energy requirements are the amount of energy needed to meet energy expenditure and maintain weight in a healthy range.
- The energy requirements can be measured or estimated from calculations.
Measurement of Energy Expenditure (MEE)
- It can involve measuring BMR and estimating additional requirements for physical activity, and diet-induced thermogenesis.
- Another method is the measurement of total energy expenditure. Direct measurement cannot measure habitual energy expenditure of a free-living individual.
- Indirect calorimetry (BMR or REE): Is short-term, up to 24 hours and requires hood/ventilator modes establishing steady state. It can measure total energy expenditure - TEE.
- Doubly-labelled water technique (TEE): Is long-term, several weeks and it has cost and technical considerations.
- Accelerometers, multi-sensor monitors are used to measure physical activity.
Methods for Estimating Energy Requirements in Disease
- Indirect calorimetry
- Factorial method e.g. PENG (2011)
- Regression equations e.g. Ireton-Jones (2002)
- Rule-of-thumb e.g. kcal/kg body weight or kcal/kg fat free mass
Factors Affecting Energy Requirements in Disease
- Age
- Gender
- Weight
- Type of illness (acute/chronic)
- Severity and phase of illness (acute/recovery)
- Metabolic state (catabolic, normal, anabolic)
- Nutritional status
- Interventions (medical, surgical, pharmacological)
- Physical activity (including the effect of any disabilities)
- Psychological state
- Aims and likely duration of nutritional support
PENG Guidelines (2011)
- It follows the underlying principle of using BMR equations derived for healthy populations and adjusting for illness in individuals
- To estimate BMR using Henry (2005).
- Adjust for metabolic stress, activity, and DIT.
- Consider additions or subtractions for weight change.
Predictive Equations
- Equations estimating BMR in health & disease.
- Equations using weight, Harris Benedict Equations (1919), Schofield Equations (1985) and Oxford (Henry) equations (2005).
- For disease-specific implementation, refer to dietary reference values (DoH, 1991) which are currently changing.
- Dietary Reference Values: Are based on the Schofield equation to calculate BMR and additions for physical activity. (DoH 1991).
- The values are average requirements for populations not individuals based on healthy free living individuals including for elderly population.
Criticisms of the PENG Recommendations - BMR Equations
- BMR equations are derived for healthy populations and not sick individuals.
- Clinical studies compare MEE with Harris-Benedict equations.
- More recently MEE is compared with other equations e.g. Schofield (1985) or Mifflin St Joer (1990).
Harris Benedict (HB) Equations (1919)
- They are based on 239 healthy subjects (data from 1909-1917).
- In the study, 136 men had a mean age of 27 ± 9 years, with a mean BMI of 21.4 ± 2.8 kg/m². While 103 women with a mean age 31 ± 14 years, with a mean BMI of 21.5 ± 4.1 kg/m².
- Considerations: Accuracy is +10-15% in healthy individuals (Daly 1985).
- Conditions reflect REE rather than BMR.
- There is a tendency to overestimate in healthy individuals (Daly 1985, Owen 1986, Owen 1987).
Harris-Benedict Equation - in clinical practice
- The equation calculates the basal energy expenditure.
- Men: BEE= 66.47 + 13.75(W) + 5(H) – 6.75(A).
- Women: BEE = 655.09+9.56(W)+1.85(H)-4.68(A).
- Activity factors and Stress/injury factors must be accounted for, where W=weight in kg, H=height in cm, A=age in years.
Schofield Equations (1985)
- Equations developed in the 1980s for WHO/FAO expert consultation and only use weight.
- The original Database contained 114 studies and 7,173 subjects with studies carried out from 1914 to 1980
- The gender split was Men (67%) and women (33%) with an ethnic background consisting of 87% North European and American (47% Italian) and few subjects from other ethnic groups (13%).
- In clinical practice, the Schofield equations are as follows:
- 15 – 18 years 13.3 W + 690 17.6 W + 656
- 18 – 30 years 14.8 W + 485 15.0 W + 690
- 30 – 60 years 8.1 W + 842 11.4 W + 870
-
60 years 9.0 W + 656 11.7 W + 585, where W = weight (kg)
- These equations are also used in COMA 1991 and FAO/WHO/UNU (FAO 2004) reports.
Schofield Equation
- It is used to estimate BMR for a healthy individual.
- In illness or disease a factor is added on.
- For a given individual, the 95% confidence limits of the BMR predicted from the Schofield equation is equal to + 15%.
- It is unreliable in very obese and very thin subjects (Tverskaya R, 1998).
Henry Equations (2005)
- Based on database of 10,552 BMR values (1914 – 2005) in which a more rigorous examination of methodology was used and measurement conditions met criteria for BMR.
- There was 55% men, 45% women.
- The proportion of ethnic minorities and elderly also increased.
- Excluded Italian/military (higher BMR), malnourished/sick and outliers e.g. Burmese hill dwellers.
- Recommended by SACN (2011) for healthy populations.
SACN (2011) Report on Energy Requirements
- It recommended the use of Henry's BMR equations for healthy populations (and individuals?).
- No specific recommendations are made for energy requirements in illness and injury.
- It also used additional data [US DRI DLW database] and found better predictive accuracy using Height + Weight.
- PENG recommends the Henry (2005) equations for predicting BMR using weight alone and Height + Weight equations.
- Height can be difficult to obtain in the clinical setting so the use of surrogates may introduce sufficient error to negate the advantage of including height.
- Schofield tends to overestimate due mainly to the Italian data (47% of Schofield database) as the higher BMR/kg than any other group.
Weight in BMR Calculations
- There many situations when weight is inaccurate as a variable.
- This will introduce error. Use estimated "dry" weight.
- In the case of amputees, legs contribute 37% of body weight and contain little metabolically active tissue so that Amputation may reduce body weight by 8-15% but will not reduce BMR by the same amount.
Rule-of-Thumb Formulae
- These are Generic equations Based on the energy value per kg body weight, fat free mass or lean body mass.
- Examples NICE, 2006, 25 - 35 kcal/kg body weight/day and ASPEN, 2002), 20 - 35 kcal/kg body weight/day.
- Originally derived for ICU patients yet no references to original work explaining how values were derived.
- Guidelines lack a defined criteria for when to use 20, 25, 30 or 35 kcal/kg/day or validation studies.
Simplistic Weight-Based Equations
- These can be imprecise
- 11-14 kcal/kg (obesity)
- 15-18 kcal/kg (obese/overweight)
- 22-25 kcal/kg (normal, healthy weight)
- 25-30 kcal/kg (underweight, or have increased needs)
- 30-35 kcal/kg (underweight, higher degree of increased needs, hematologic malignancy)
- 40+ kcal/kg (increased needs, weight gain)
Criticisms of Rule-of-Thumb Formulae
- REE (or TEE) is not always clearly stated
- There is a lack of clatiry for people who are obese or underweight whether requirements should be calculated using actual or ideal body weight.
- Guidelines that do not account for changes in energy expenditure with age, gender or metabolic state
Case Study
- 70 year old male, Weight 65 kg, BMI: 20 kg/m²
- Hospitalised with acute exacerbation of COPD on day 5 to be discharged.
Estimation of Energy Requirements for this patient
- BMR + stress + activity/DIT1 (kcal/day) = 1,960 kcal/day using PENG guidelines (2011)
- 25 - 35 kcal/kg/day² = 1,625 – 2,275 kcal/day using NICE guidelines (2006)
- 20 - 35 kcal/kg/day³ = 1,300 - 2,276 kcal/day using ASPEN guidelines (2002)
- Males = 11.5 x wt [kg] + 9524 = 1,700 kcal/day using Moore & Angelilo (1988)
Process to Calculate Energy Requirements
- Decide on the aim of the nutritional intervention from the results of nutrition assessment
- Is the patient in the acute phase and requires extra energy due to stress? Or Is the patient stable but under/overweight?
- Calculate approximate BMR then add on factors for: Disease state (Elia normogram), physical activity and diet induced thermogenesis.
Case Study - Mrs Maria Borg
- Maria is a 62 year old woman with leukaemia admitted to hospital for 3rd cycle of chemotherapy.
- On admission nurses have noted that Maria was looking much thinner than at her previous appointments.
- Nutritional assessment shows following results Weight 40kg, Height 1.68m, BMI 14.2kg/m², Pre-illness weight 60kg, % weight loss 33.3%.
Case Study - Mrs Borg
- Aim: is to Minimise further losses in and maintain nutritional status.
- Objectives are to Calculate and meet estimated requirements for energy, nitrogen, fluid, electrolytes and micronutrients and Provide appropriate and adequate nutritional support
- Rationale of maintaining energy requirements although the Patient is undernourished is suggesting inflammatory response present.
- BMR = 9.0 x 40 + 656 = 1016kcal using Schofield.
- For 30 – 60 years of age, follow equation Male kcal/day = 8.1 W + 842. For > 60 years of age, follow equation Male kcal/day = 9.0 W + 656
- Next Adjust for stress using normogram (Elia normogram), or stress factors (The Elia normogram is used with Schofield to identify a stress factor although it not exhaustive, many clinical conditions are not included).
- Factors that affect stress: Air temperature, amount affect EE, Thermoneutral zone is 26-29°c, In stress the core temperature rises and patient may become pyrexial and In pyrexia energy must maintain body temperature in the thermoneutral zone for an increased rate of biochemical reactions.
- Sedation, anaesthesia and paralysing agents all decreaseenergy expenditure with reduced skeletal activity. Steroids or stimulants including e.g. dexamethasone, amphetamines, nicotine and caffeine all results in increasing energy expenditure.
- Many clinical guidelines and estimates are available for different disease states (Barak N, 2002). Be sure to follow clinical evidence (when factors are added, the clinician should develop an evidence based approach).
Metabolic State
- Increased CRP and decreased albumin.
- Increased white cell count
- Increased blood urea and glucose levels
- Increased body temperature.
- There is also an Increased Heart Rate, Poor appetite, oedema and fatigue .
- Next steps, how do indicators of metabolic state translate to "stress factors"?
- In the presence of an inflammatory response it is challenging to achieve weight gain and other clinical benefits with nutritional support alone
How to Apply this information
- In the Maria Borg case, we make BMR = 1016kcal and using a stress factor of 25% = 254kcal, that gives us an an Energy requirement of 1016 + 254Kcal.
- Now the additionof a Add a combined factor for activity and diet induced thermogenesis.
- Physical activity for Energy expended during active movement of skeletal muscle.
- It is unlikely to exceed ~ 20% total energy expenditure in hospitalized patients whereas it accounts more between 20-40% in fee living individuals or on intensity of exercise. Be aware that PALs include a factor for DIT and assumes normal neuro-muscular function.
- In hospitalised patients however, physical activity may be increased due to Abnormal neuro-muscular function e.g. brain injury, Parkinson's disease, cerebral palsy, motor neurone disease, Prolonged and active physical therapy. The increased effort involved in moving injured or painful limbs.
- Then select from combined activity factors: If a patient is Bedbound immobile add 10%, Bedbound mobile sitting add 15 -20, If they are mobile or on ward then add 25%.
To finish Estimation process:
- Account for Diet Induced Thermogenesis- energy expenditure due to ingestion of food. Energy used for digestion, absorption, transport and storage of ingested nutrients.
- Approximately 10% of energy intake from either an enteral or parenteral diet with slightly higher rate from when feeding protein that fat or carbohydrates.
Estimating Weight Gain
- If increased energy stores are required add 400 – 1000kcal per day.
- If decrease in energy stores is required reduce energy intake.
- Account for that a stressed patient is unlikely to gain weight therefore weight loss may not be the goal in overweight but stressed patient so a factor for weight gain or /loss is usually only added once the acute phase is over.
- In the Maria Borg case we were able to utilise additional energy provided due to inflammatory response so there are No additions for weight gain despite undernutrition..
- Energy Requirements in this case = 1500kcal
Critical Considerations
- Critisms of PENG: Inappropriate use of stress factors .
- A wide range of stress factors reported for some conditions exist(PENG have always recommended to start at the lower end, monitor and adjust if necessary)
- Changes in medications (Treatments and medical nursing practice).
- Also Inappropriate use of static variables such as weight.
- Weight can be be inaccurate and does not reflect changes in body’s physiology such as respiratory rate or temperature
- Therefore need to be careful about calculating appropriate weight as: that overweight patients have a higher proportion of adipose tissue, said adipose tissue is less metabolically active, leading to feeding to actual body weight may result in overfeeding (with this case follow equation to calculate for obese patients BMI > 30 for how suggested.
Useful Points
- ESPEN guidelines: ideal body weight + 25% excess or ideal body weight + 50% excess or MEE was 19kcal/ kg in obese critically ill patients (BMI >30) (Alberda 2002) and underweight patients (BMI < 19) have a higher proportion of lean body mass may be underfed
Which weight to use?
- Actual body weight (ABW), Ideal body weight (IBW) or Adjusted body weight e.g. 25 % (ABW x 0.25 + IBW). The best one to use reamins contentious as there is little evidence to support any particular method
- There is a risk of Adverse Effect in Over-Feeding as it leads to increased CO2 production and excess CHO can lead to respiratory problems in vulnerable patients . Aim not to exceed the glucose oxidation rate . Also leads to the issue of term excess carbohydrate leading to steatohepatosis or fatty liver
- Very low energy requireemnts exisit: Small proportion of patients on long term ANS may have much lower energy requirements than predicted for immobile patients with neuro-developmental disabilities or severe damage to the CNS receiving long term tube feeding.
Things to note when feeding patients with low energy levels
- REE range of 800 – 950 kcal/day, however when expressed as kcal/kg body weight, results for individuals were variable, from as low as 12.6 kcal/kg/d up to 34 kcal/kg/d
- Ask: "do low requirements for energy indicate low requirements for other nutrients?"
Other considerations
- Remember Re-feeding syndrome so that Key is successful management and prevention, Early identification of at-risk individuals and Monitor whilst re-feeding!
- The correct Appropriate feeding regimen of cautious re-introduction of energy/correction of biochemical abnormalities (Although Lack of randomized controlled trial evidence may require electrolyte adnormalities before starting)
Protein and Amino Acid Requirements
- Dietary protein is required: Maintaining protein turnover synthesis of products of amino acid metabolism and laying down new tissue. . Protein cannot be stored, and losses occur even if no protein is consumed.
So How is Protein requirements measured?
- Assuming energy intake is adequate, protein requirements is the amount to maintain N balance so this approach must have limitations (n balance can be difficult to measure accurately, N balance may be influenced by recent intake, N balance and equilibrium does not reflect requirements for individual amino acids).
- Aa requirement is the quantity of aa’s to support optimum health and must be classified to essential and non-essential. Conditionally essential is when: a AA derives from the metabolism of the other aa or nitrogenous metabolite or it's more complicated than simple transamination or Under certain circumstances dietary precursors may not be available in required amounts.
- Important fact, is that the RNI for protein in healthy adults is 0.75g/kg and requirements are increased. If there growth, sepsis and stress the proportion essential to non-essential aa’s might also alter requiring possible supplementation due to great losses in early catabolic phase for +ve N balance.
How is all this applied in practice?
- Normal requirements = 0.17/kg nitrogen (0.14-0.20 nitrogen) wherease Hypermetabolic accounts for more >0.20N/kg with depleted accounting for 0.3.
Consider the Case Study one last time
- Weight = 40kg, Stress factor = 25% using 0.8 protein
- Nitrogen requirements = 0.2 x 40 = 8g Nitrogen
- Protein requirements = 8 x 6.25 = 50g Protein
Fluid and Electrolyte Requirements
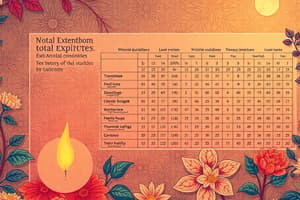
- See attached table for various electrolyte and fluid oral and IV requirements and remember when and why you use them (such as fevers, refeeding, other underlying issues)
In Maria Borg Case:
- Weight = 40kg
- Fluid requirements = 30ml x 40kg = 1200ml Fluid (although you do not give >1500ML to patients who have no other symptoms)
- Sodium 40mmol (minimum requirement 60mmol)
- Potassium 40mmol (minimum requirement 60mmol)
- Phosphate 12mmol, Magnesium 8mmol and Calcium 8mmol
Micronutrient Requirements and Considerations
- Follow Recommends intakes for to Prevent deficiency in both healthy diet and during and under artificial (intake). Also follow Micro-requirements levels (the drugs that supplements are given for different functions) and sub-optimal levels as they must impact normal defienecy sign (assessment as based on adequacy of signs).
PENG Guidelines: Energy
- Only data used where energy expenditure was measured in clinical settings using Validated equipment and standard conditions for measuring REE, TEE and physical activity in comparison to healthy controls Data reviewed on factors likely to impact requirement such Gender, age, weight ,body composition with Review of data on factors likely to impact requirements. Gender, age, weight , body composition and potential indicators of hypermetabolism
- Remember to find a balance*.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.