Podcast
Questions and Answers
What is the primary cause of unstable angina?
What is the primary cause of unstable angina?
- High cholesterol levels alone
- Obstruction and/or spasm of the coronary arteries (correct)
- Increased physical activity without prior conditioning
- Low blood pressure during exercise
What is the main risk factor leading to in-stent restenosis?
What is the main risk factor leading to in-stent restenosis?
- Poor diet following stent insertion
- Excessive weight gained after the procedure
- Neointimal hyperplasia due to injury from stent placement (correct)
- Inadequate medication adherence post-procedure
What treatment may be used for an ischaemic stroke to counteract its adverse effects?
What treatment may be used for an ischaemic stroke to counteract its adverse effects?
- Surgical bypass grafting
- Tissue plasminogen activator (tPA) (correct)
- Anticoagulant therapy alone
- Beta-blockers for heart rate control
What is a serious consequence of untreated peripheral vascular disease (PVD)?
What is a serious consequence of untreated peripheral vascular disease (PVD)?
What critical symptom may indicate a need for carotid endarterectomy?
What critical symptom may indicate a need for carotid endarterectomy?
What is associated with an increased risk of abdominal aortic aneurysm (AAA) rupture?
What is associated with an increased risk of abdominal aortic aneurysm (AAA) rupture?
Which of the following is NOT a typical symptom of angina?
Which of the following is NOT a typical symptom of angina?
What factor is significant in diagnosing acute myocardial infarction?
What factor is significant in diagnosing acute myocardial infarction?
What age group is invited for ultrasound screening for abdominal aortic aneurysms in the UK?
What age group is invited for ultrasound screening for abdominal aortic aneurysms in the UK?
Which of the following best describes claudication associated with peripheral vascular disease?
Which of the following best describes claudication associated with peripheral vascular disease?
What is the primary function of endothelial cells in blood vessels?
What is the primary function of endothelial cells in blood vessels?
How is pulse wave velocity relevant to vascular health?
How is pulse wave velocity relevant to vascular health?
Which of the following best describes atherosclerosis?
Which of the following best describes atherosclerosis?
What role does shear stress play in endothelial cell function?
What role does shear stress play in endothelial cell function?
Which of the following statements about vascular calcification is true?
Which of the following statements about vascular calcification is true?
What consequence can atherosclerosis lead to in blood vessels?
What consequence can atherosclerosis lead to in blood vessels?
What indicates high velocities in a carotid artery plaque scan?
What indicates high velocities in a carotid artery plaque scan?
What is a potential impact of vascular calcification in older adults?
What is a potential impact of vascular calcification in older adults?
Flashcards
Endothelium
Endothelium
The inner lining of blood vessels, only one cell thick. It's sensitive to blood flow and regulates vessel width.
Pulse Wave Velocity
Pulse Wave Velocity
The speed at which pressure waves travel through arteries, an indicator of arterial stiffness. Measured by ultrasound.
Atherosclerosis
Atherosclerosis
A buildup of fatty deposits (plaques) in artery walls, leading to narrowing and increased risk of blood clots.
Shear stress
Shear stress
Signup and view all the flashcards
Vascular Calcification
Vascular Calcification
Signup and view all the flashcards
Laminar flow
Laminar flow
Signup and view all the flashcards
Disturbed flow
Disturbed flow
Signup and view all the flashcards
Vascular Tone
Vascular Tone
Signup and view all the flashcards
Ischaemic heart disease
Ischaemic heart disease
Signup and view all the flashcards
Acute myocardial infarction (MI)
Acute myocardial infarction (MI)
Signup and view all the flashcards
In-stent restenosis
In-stent restenosis
Signup and view all the flashcards
Coronary Artery Bypass Graft (CABG)
Coronary Artery Bypass Graft (CABG)
Signup and view all the flashcards
Ischaemic Stroke
Ischaemic Stroke
Signup and view all the flashcards
Tissue Plasminogen Activator (tPA)
Tissue Plasminogen Activator (tPA)
Signup and view all the flashcards
Carotid Endarterectomy
Carotid Endarterectomy
Signup and view all the flashcards
Carotid Duplex
Carotid Duplex
Signup and view all the flashcards
Peripheral Vascular Disease (PVD)
Peripheral Vascular Disease (PVD)
Signup and view all the flashcards
Aortic Aneurysm
Aortic Aneurysm
Signup and view all the flashcards
Study Notes
Endothelial Cells and Vascular Function
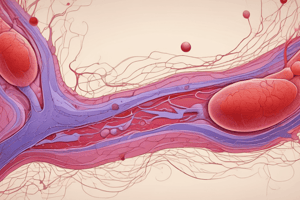
- Endothelial cells line blood vessels, forming a single cell layer.
- These cells are mechanosensitive, reacting to blood flow and pressure.
- They actively regulate vascular tone (dilation and constriction).
- They are key regulators of vascular homeostasis, responding to various physical and chemical signals.
Pulse Wave Velocity (PWV)
- PWV measures arterial stiffness via ultrasound.
- It assesses the speed of pressure waves traveling through arteries.
- Calculated by dividing distance by pressure wave transit time.
Atherosclerosis
- Atherosclerosis involves lipoprotein buildup in artery walls, forming plaques.
- This process involves endothelial activation, inflammation, necrosis, fibrosis, and calcification.
- Plaque formation narrows vessels, increasing risk of thrombi and rupture.
- Obstructs blood flow to vital organs (heart, brain, extremities).
- Carotid artery plaque scans (ultrasound) use color-coded flow for visualization (red=normal, yellow=high, blue=very high).
Endothelial Response to Shear Stress
- Endothelial cells respond to shear stress (blood flow friction).
- Shear stress influences endothelial health, preventing or promoting cardiovascular disease (CVD).
- Response changes depending on blood flow type (laminar, disturbed).
Vascular Calcification
- Calcium deposits are common in arterial walls for individuals aged 60+.
- Calcification can occur within the intima or media layer.
- Increasingly recognized as a serious problem.
- Leads to vessel stiffness and increased blood pressure.
Consequences of Atherosclerosis: Coronary Artery Disease
- Ischemic Heart Disease (Angina):
- Coronary artery blockage or spasm reduces myocardial oxygen supply.
- Symptoms: triggered by exercise, stress, cold.
- Treatment: nitrates, calcium channel blockers, beta-blockers.
- Acute Myocardial Infarction (Heart Attack):
- Blocked coronary artery by an embolus leads to myocardial ischemia.
- Severity varies based on blockage size.
- Symptoms: chest pain, shortness of breath, weakness, anxiety.
- Diagnosis aid: elevated serum troponin (cardiac muscle damage).
- In-Stent Restenosis:
- Re-narrowing of an artery after stent placement.
- Caused by neointimal hyperplasia (new tissue growth).
- Treatment: drug-eluting stents (reduce proliferation).
- Coronary Artery Bypass Graft (CABG):
- Surgical procedure for patients with advanced atherosclerosis.
- Bypasses blocked coronary arteries using grafts (saphenous vein, internal mammary artery).
Consequences of Atherosclerosis: Stroke
- Ischemic Stroke: Compromised brain blood supply.
- Caused by local thrombus or distant plaque rupture (often internal carotid artery).
- Variable symptoms based on affected brain region.
- Treatment: tissue plasminogen activator (tPA), anticoagulants, carotid endarterectomy.
- Carotid Artery Imaging:
- Ultrasound assesses carotid artery condition, including stenosis (narrowing).
- Severe stenosis (>70%) may necessitate carotid endarterectomy surgery.
Consequences of Atherosclerosis: Peripheral Vascular Disease (PVD)
- Atherosclerosis obstructs large arteries outside coronary & aortic arch vasculature.
- Primarily affects lower extremities, causing ischemia.
- Symptoms: intermittent claudication (leg pain), color changes, wounds that don't heal.
- Severe cases involve limb loss.
- Increased mortality after foot ulcer development in PVD patients.
Consequences of Atherosclerosis: Aortic Aneurysms
- Pro-atherogenic factors (high blood pressure, cholesterol, smoking, inflammation) contribute to aortic stiffening.
- Weakening and bulging of aortic wall.
- Often asymptomatic, but may present as a pulsating abdominal mass.
- Aortic aneurysm rupture is life-threatening.
- UK screening for men over 65 via ultrasound.
- At-risk patients may receive surgical grafting.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.