Podcast
Questions and Answers
What is the primary method by which hormones are transported throughout the body in the endocrine system?
What is the primary method by which hormones are transported throughout the body in the endocrine system?
- The bloodstream (correct)
- Lymphatic system
- Direct nerve pathways
- Diffusion across cell membranes
Which of the following is NOT a primary function of the endocrine system?
Which of the following is NOT a primary function of the endocrine system?
- Controlling bone remodeling and calcium deposition. (correct)
- Coordinating reproductive systems, including maturation and gamete production.
- Regulating development of the reproductive system and the central nervous system in the fetus.
- Adjusting responses to stress, injuries and emergency situations.
Which of the following is a paired endocrine gland?
Which of the following is a paired endocrine gland?
- Thyroid gland
- Adrenal gland (correct)
- Pituitary gland
- Pancreas
Which of the following structures is NOT a gland of the endocrine system?
Which of the following structures is NOT a gland of the endocrine system?
Besides the reproductive system, what other system does the endocrine system influence during fetal development?
Besides the reproductive system, what other system does the endocrine system influence during fetal development?
Which of the following is a risk factor for thyroid cancer?
Which of the following is a risk factor for thyroid cancer?
What is the most common cause of primary hyperparathyroidism?
What is the most common cause of primary hyperparathyroidism?
What is the primary function of parathyroid hormone (PTH)?
What is the primary function of parathyroid hormone (PTH)?
Which of the following is NOT a symptom of hypercalcemia?
Which of the following is NOT a symptom of hypercalcemia?
What is the most common type of thyroid cancer?
What is the most common type of thyroid cancer?
Which of the following is a treatment option for thyroid cancer?
Which of the following is a treatment option for thyroid cancer?
What is the recommended treatment for hyperparathyroidism?
What is the recommended treatment for hyperparathyroidism?
Which of the following conditions can lead to secondary hyperparathyroidism?
Which of the following conditions can lead to secondary hyperparathyroidism?
What is the primary function of the endocrine system in relation to the musculoskeletal system?
What is the primary function of the endocrine system in relation to the musculoskeletal system?
Which of the following is a common effect of catecholamines released during a stress response?
Which of the following is a common effect of catecholamines released during a stress response?
What is a typical effect of cortisol release from the adrenal cortex during stress?
What is a typical effect of cortisol release from the adrenal cortex during stress?
A patient presents with bilateral carpal tunnel syndrome. What other condition should a physical therapist consider in their differential diagnosis?
A patient presents with bilateral carpal tunnel syndrome. What other condition should a physical therapist consider in their differential diagnosis?
Which hormone is secreted by the anterior lobe of the pituitary gland that stimulates the adrenal cortex?
Which hormone is secreted by the anterior lobe of the pituitary gland that stimulates the adrenal cortex?
A patient with a pituitary tumor reports headaches and visual disturbances. Why might this be?
A patient with a pituitary tumor reports headaches and visual disturbances. Why might this be?
What is a characteristic feature of acromegaly in adults due to hyperpituitarism?
What is a characteristic feature of acromegaly in adults due to hyperpituitarism?
Which of the following conditions is associated with an over-secretion of ACTH, a hormone of the anterior pituitary gland?
Which of the following conditions is associated with an over-secretion of ACTH, a hormone of the anterior pituitary gland?
What is a common cause of Cushing's Disease?
What is a common cause of Cushing's Disease?
What is a potential effect of increased prolactin levels due to hyperpituitarism?
What is a potential effect of increased prolactin levels due to hyperpituitarism?
What is the most common treatment for benign pituitary tumors causing hyperpituitarism?
What is the most common treatment for benign pituitary tumors causing hyperpituitarism?
What are some signs of increased intracranial pressure that a physical therapist should be aware of?
What are some signs of increased intracranial pressure that a physical therapist should be aware of?
What is a common cause of hypopituitarism?
What is a common cause of hypopituitarism?
What is one of the roles of Human Growth Hormone (HGH) in the body?
What is one of the roles of Human Growth Hormone (HGH) in the body?
Which symptom is a common manifestation of hypopituitarism?
Which symptom is a common manifestation of hypopituitarism?
What is a primary cause of Type I hypothyroidism?
What is a primary cause of Type I hypothyroidism?
Which of the following is NOT a common symptom of hypothyroidism?
Which of the following is NOT a common symptom of hypothyroidism?
What diagnostic result is expected in a patient with hypothyroidism?
What diagnostic result is expected in a patient with hypothyroidism?
Which of the following is a potential complication of thyrotoxicosis?
Which of the following is a potential complication of thyrotoxicosis?
Which musculoskeletal effect is associated with hypothyroidism?
Which musculoskeletal effect is associated with hypothyroidism?
In women with rheumatoid arthritis, what condition is often observed?
In women with rheumatoid arthritis, what condition is often observed?
What treatment is commonly administered for hypothyroidism?
What treatment is commonly administered for hypothyroidism?
What effect does hypothyroidism have on cholesterol levels?
What effect does hypothyroidism have on cholesterol levels?
What is a common symptom of hyperthyroidism?
What is a common symptom of hyperthyroidism?
What is the main characteristic of diabetes insipidus?
What is the main characteristic of diabetes insipidus?
Which test is commonly used to evaluate hormonal levels in hypopituitary disorders?
Which test is commonly used to evaluate hormonal levels in hypopituitary disorders?
What condition can result from untreated hyperthyroidism?
What condition can result from untreated hyperthyroidism?
What hormonal treatment is primarily used for patients with hypopituitary disease?
What hormonal treatment is primarily used for patients with hypopituitary disease?
Which symptom is associated with Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH)?
Which symptom is associated with Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH)?
What is a likely effect of gonadotropin deficiency in males?
What is a likely effect of gonadotropin deficiency in males?
Which of the following is a treatment for diabetes insipidus?
Which of the following is a treatment for diabetes insipidus?
What is a common characteristic of thyroid disorders?
What is a common characteristic of thyroid disorders?
What age group is primarily affected by Graves disease?
What age group is primarily affected by Graves disease?
What is a common cause of iatrogenic hypoparathyroidism?
What is a common cause of iatrogenic hypoparathyroidism?
Which electrolyte imbalance is associated with hypoparathyroidism?
Which electrolyte imbalance is associated with hypoparathyroidism?
What systemic effect is associated with hypoparathyroidism?
What systemic effect is associated with hypoparathyroidism?
What is a primary function of cortisol released from the adrenal cortex?
What is a primary function of cortisol released from the adrenal cortex?
What potential consequence may occur if Addison's disease is untreated?
What potential consequence may occur if Addison's disease is untreated?
Which hormone's secretion decreases in Addison's disease leading to hypotension?
Which hormone's secretion decreases in Addison's disease leading to hypotension?
What is a common diagnostic method for Addison's disease?
What is a common diagnostic method for Addison's disease?
What effect does hypoparathyroidism have on respiratory muscles?
What effect does hypoparathyroidism have on respiratory muscles?
Which symptom is least likely associated with hypoparathyroidism?
Which symptom is least likely associated with hypoparathyroidism?
What treatment may be necessary in the event of tetany due to hypoparathyroidism?
What treatment may be necessary in the event of tetany due to hypoparathyroidism?
Flashcards
Endocrine System
Endocrine System
A group of glands that produce and release hormones into the bloodstream.
Hormones
Hormones
Chemical messengers that regulate various bodily functions by targeting specific organs or tissues.
Pituitary Gland
Pituitary Gland
The master gland of the endocrine system located at the base of the brain.
Thyroid Gland
Thyroid Gland
Signup and view all the flashcards
Thymus Gland
Thymus Gland
Signup and view all the flashcards
Hyperthyroidism
Hyperthyroidism
Signup and view all the flashcards
Graves' Disease
Graves' Disease
Signup and view all the flashcards
Goiter
Goiter
Signup and view all the flashcards
Diabetes Insipidus
Diabetes Insipidus
Signup and view all the flashcards
Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH)
Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH)
Signup and view all the flashcards
Hypothyroidism Type I
Hypothyroidism Type I
Signup and view all the flashcards
Hypopituitarism
Hypopituitarism
Signup and view all the flashcards
Gonadotropin deficiency
Gonadotropin deficiency
Signup and view all the flashcards
Hypothyroidism Type II
Hypothyroidism Type II
Signup and view all the flashcards
Proximal Hip Weakness
Proximal Hip Weakness
Signup and view all the flashcards
Hypoglycemia
Hypoglycemia
Signup and view all the flashcards
Hyponatremia
Hyponatremia
Signup and view all the flashcards
Elevated TSH
Elevated TSH
Signup and view all the flashcards
Hypothyroidism
Hypothyroidism
Signup and view all the flashcards
Synthroid Treatment
Synthroid Treatment
Signup and view all the flashcards
Untreated Hypothyroidism Risks
Untreated Hypothyroidism Risks
Signup and view all the flashcards
Exercise for Constipation
Exercise for Constipation
Signup and view all the flashcards
Endocrine dysfunction's impact on the musculoskeletal system
Endocrine dysfunction's impact on the musculoskeletal system
Signup and view all the flashcards
Neuroendocrine response to stress
Neuroendocrine response to stress
Signup and view all the flashcards
Catecholamines
Catecholamines
Signup and view all the flashcards
Cortisol
Cortisol
Signup and view all the flashcards
Anterior pituitary lobe functions
Anterior pituitary lobe functions
Signup and view all the flashcards
Posterior pituitary lobe functions
Posterior pituitary lobe functions
Signup and view all the flashcards
Pituitary tumors (Adenomas)
Pituitary tumors (Adenomas)
Signup and view all the flashcards
Acromegaly
Acromegaly
Signup and view all the flashcards
Cushing's disease
Cushing's disease
Signup and view all the flashcards
Excess prolactin
Excess prolactin
Signup and view all the flashcards
HGH deficiency
HGH deficiency
Signup and view all the flashcards
Acquired HGH deficiency
Acquired HGH deficiency
Signup and view all the flashcards
Papillary Thyroid Carcinoma
Papillary Thyroid Carcinoma
Signup and view all the flashcards
Follicular Thyroid Carcinoma
Follicular Thyroid Carcinoma
Signup and view all the flashcards
Parathyroid Gland
Parathyroid Gland
Signup and view all the flashcards
Parathyroid Hormone (PTH)
Parathyroid Hormone (PTH)
Signup and view all the flashcards
Hyperparathyroidism
Hyperparathyroidism
Signup and view all the flashcards
Primary Hyperparathyroidism
Primary Hyperparathyroidism
Signup and view all the flashcards
Secondary Hyperparathyroidism
Secondary Hyperparathyroidism
Signup and view all the flashcards
Parathyroidectomy
Parathyroidectomy
Signup and view all the flashcards
Hypocalcemia
Hypocalcemia
Signup and view all the flashcards
Hyperphosphatemia
Hyperphosphatemia
Signup and view all the flashcards
Tetany
Tetany
Signup and view all the flashcards
Bone Reabsorption
Bone Reabsorption
Signup and view all the flashcards
Iatrogenic Hypoparathyroidism
Iatrogenic Hypoparathyroidism
Signup and view all the flashcards
Addison Disease
Addison Disease
Signup and view all the flashcards
Aldosterone
Aldosterone
Signup and view all the flashcards
Adrenal Cortex
Adrenal Cortex
Signup and view all the flashcards
Study Notes
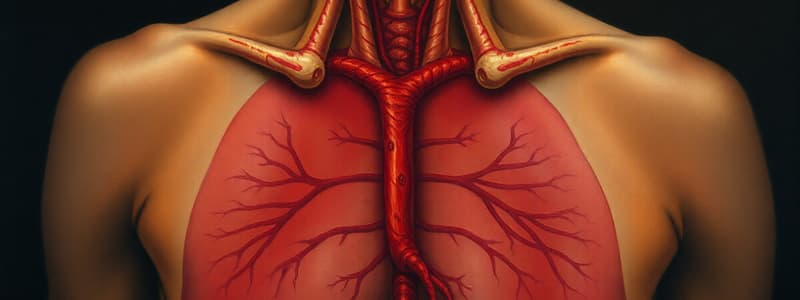
Endocrine System Overview
- Composed of numerous glands producing hormones
- Hormones travel through the bloodstream to target organs, affecting their function
- The endocrine system is responsible for:
- Fetal development of reproductive system and CNS
- Growth and development in childhood/adolescence
- Coordinating reproductive systems
- Maintaining internal environment
- Responding to emergency situations
Primary Function
- Secretion of hormones
Glands
- Pituitary
- Thyroid
- Parathyroid
- Adrenal
- Pancreas
- Pineal
- Thymus
- Ovaries/Testes
Endocrine Dysfunction
- Dysfunction causes alterations in the body's systems because the endocrine system regulates growth and development
Results from
- Hyperfunction or hypofunction
Neuroendocrine Response to Stress
- Immune and endocrine systems are intimately related
- Stress increases sympathetic nervous system activity
- Adrenal glands release catecholamines
- Pituitary gland releases:
- ADH (antidiuretic hormone)
- Prolactin
- GH (growth hormone)
- ACTH (adrenocorticotropic hormone)
- Pituitary gland releases:
Neuroendocrine Response to Stress (Catecholamines)
- Epinephrine
- Increases heart rate and strength
- Causes peripheral vasoconstriction
- Elevates blood pressure
- Elevates blood glucose
- Stimulates fat breakdown
- Norepinephrine
- Dopamine
Neuroendocrine Response to Stress (Cortisol)
- Released from adrenal cortex
- Regulates proteins, carbohydrates, and lipids to increase blood glucose
- Inhibits fibroblast proliferation (poor wound healing, increased infection risk)
- Helps with fight-or-flight response
- Reduces inflammation
Pituitary Gland
- Master gland
- Anterior Lobe (Adenohypophysis)
- Secretes ACTH, TSH, LH, FSH, HGH, Prolactin
- Posterior Lobe (Neurohypophysis)
- Stores ADH (antidiuretic hormone), Oxytocin
Pituitary Tumors (Adenomas)
- Signs/symptoms:
- Headaches
- Increased intracranial pressure (ICP)
- Decreased drainage from 3rd ventricle
- Visual disturbances (optic chiasm, bilateral temporal hemianopsia)
- Endocrine abnormalities
Anterior Pituitary Gland Disorders
- Over secretion of at least one hormone (hyperpituitarism):
- HGH (Human Growth Hormone) → acromegaly in adults (usually benign tumor)
- Excessive growth (overgrowth of long bones, hypertrophy of soft tissues, widened joint spaces)
- Children can grow to >7ft (often up to 9 ft).
- Adults (30-50yrs)-Increased size of jaw bones, hands/feet
- ACTH → Cushing's disease (often due to an adenoma or exposure to glucocorticoids)
- Muscle wasting, osteopenia, moon face, easy bruising, abdominal striae, acne, obesity, glucose intolerance, 5:1 women to men ratio, typically seen in childbearing years.
- HGH (Human Growth Hormone) → acromegaly in adults (usually benign tumor)
- Prolactin diseases (over-secretion) - Amenorrhea, Gynecomastia, Lactation, Decreased libido, impotence.
HYPERpituitarism Medical/Surgical Treatment
- Benign tumors → surgery and/or radiation
- Medications to decrease or stunt hormone production
HYPERpituitarism Physical Therapy Implications
- Ambulation/exercise encouraged 24 hours post-op
- Watch for changes in consciousness, vision, pulse, and blood pressure (may signal increased ICP); report these changes
- Monitor for meningitis symptoms (headache, irritability, neck rigidity)
HYPOPituitarism
- Diminished secretion by anterior lobe (>70%)
- Congenital and acquired etiologies:
- Tumours
- Postpartum hemorrhage
- Anorexia
- Anemia
- GI dysfunction
- Gradual onset of symptoms and signs
- HGH → decreased growth, delayed puberty (affects cartilage, skeletal muscle, connective tissue, skin; enhances fatty acid production)
- LH/FSH → sexual/reproductive disorders
HYPOPituitarism - Signs and Symptoms
- Fatigue
- Muscle weakness
- Weight loss
- Poor appetite
- Joint stiffness
- Low blood pressure
- Headaches
- Erectile dysfunction
- Irregular menstruation
- Delayed growth/poor growth in children
Congenital HGH Deficiency
- Normal birth length
- Drop off height curve by 1-2 years of age
- Normal intelligence
- Obesity
- Delayed skeletal maturation
- Delayed puberty
- Short
- HGH replacement therapy (daily shot or during growth periods)
Acquired HGH Deficiency
- Tumor or treatment for tumor
- Increased cardiac disease
- Central adiposity
- Insulin resistance
- Poor lipid profile
HYPOPituitary Disease - Gonadotropin deficiency
- Amenorrhea
- Breast atrophy
- Testicular atrophy
- Diminished libido
- Minimal pubic and axillary hair
- Hypothermia
- Hypotension
- Hypoglycemia
HYPOPituitary Disorders: Tests & Measures
- Blood work: Cortisol, prolactin, thyroxine, TSH, testosterone, estrogen, LH, FSH, HGH
- MRI of hypothalamus/pituitary
- Radiographs of hands in children to determine growth
HYPOPituitary Disease Medical Treatment
- Removal of causative factor (e.g., surgical tumor removal)
- Hormone replacement therapy (lifelong):
- Steroids to replace adrenal hormones
- Synthroid to correct loss of TSH
- Sex hormones
- Growth hormones
HYPOPituitarism - Implications for Physical Therapy
- May observe weakness, fatigue, lethargy, apathy, orthostatic hypotension
- Prevent infections
- Impaired vision may occur (bilateral hemianopia)
Posterior Pituitary Lobe Disorders
- Diabetes Insipidus:
- Rare; caused by damage to hypothalamus or posterior pituitary
- ADH (antidiuretic hormone) deficiency
- Kidneys don't reabsorb enough water
- Copious, diluted urine
- Dehydration, dizziness,fatigue, polydipsia
- Treatment: ADH replacement with medication
- Syndrome of Inappropriate ADH Secretion (SIADH)
- Increased ADH secretion
- Caused by infections, trauma, tumors, medications
- Increased water retention, hyponatremia (low sodium in blood)
- Lethargy, weakness, coma
- Treatment: Correct sodium balance (surgery, chemotherapy, radiation if tumor, fluid restriction, diuretics)
Thyroid Gland
- Located inferior to larynx
- Secretes:
- Thyroxine (T4)
- Triiodothyronine (T3)
- Calcitonin
- Actions:
- Regulates basal metabolism
- Promotes growth and development
- Mobilizes fat
- Exchanges electrolytes and proteins
Thyroid Disorders
- More common in women (4:1) and those with family history
- Affects many body systems:
- Hair
- Nails
- Eyes
- GI tract
- Lungs
- Heart
- Nervous tissue
- Bones
- Muscles
Hyperthyroidism
- Graves Disease: An autoimmune disease causing thyroid enlargement and increased hormone secretion (sympathetic nervous system activity increase)
- Accounts for 85% of hyperthyroidism cases
- Typically occurs between 20-40 years of age; predominantly seen in women (4:1)
- Can occur during pregnancy
- Symptoms:
- Increased size of thyroid (goiter)
- Heat intolerance
- Weight loss
- Sweating
- Tremor
- Tachycardia
- Irritability
- Poor concentration
- Diarrhea
- Mood swings
- Exophthalmos (eye protrusion)
- Diagnosis: Decreased or normal TSH, elevated T3 & T4, increased radioactive iodine uptake
- Treatment: Medication to inhibit synthesis (30% remission without treatment), radioactive iodine (RAI), followed by thyroid medication (RAI causes hypothyroidism), surgery
- Physical Therapy Implications: Exercise intolerance and reduced exercise capacity, proximal muscle weakness and myopathy, thyrotoxicosis can aggravate pre-existing heart disease, lead to atrial fibrillation, congestive heart failure, and worsen angina pectoris, increased risk for myocardial infarction.
Hypothyroidism
- Decreased thyroid hormones, slowing metabolism
- Causes:
- Autoimmune (Hashimoto's Thyroiditis)
- Surgery affecting thyroid
- Overmedication for hyperthyroidism
- Diet
- Congenital
- More prevalent in women (30-60 years old)
- Type I: Hormone deficient (loss of thyroid tissue).
- Type II: Hormone resistant (pituitary failure to synthesize adequate TSH)
- Pathology: Thyroid tissue destruction → decreased thyroid hormone secretion → increased TSH secretion from the anterior pituitary
- Symptoms:
- Slowed metabolism (decreased GI tract mobility, weight gain)
- Bradycardia
- Slowed neurologic function (slow speech, decreased short-term memory, increased sleep, headache, cerebellar ataxia, mood changes)
- Increased cholesterol and triglycerides
- Anemia
- Musculoskeletal effects (proximal hip weakness, myalgia, stiffness in small joints, paresthesia, joint edema, increased bone density, carpal tunnel)
- Diagnosis: Elevated TSH, normal or decreased T3 & T4, elevated CPK-MB
- Treatment: Synthetic thyroid hormones (Synthroid)
- Prognosis: Untreated can cause severe CAD (increased triglycerides and cholesterol)
- Physical Therapy Implications: Correlation between hypothyroidism and fibromyalgia syndrome (FMS) continues to be investigated. Increased activity and exercise help clients with constipation from slowed metabolism and decreased peristalsis.
Thyroid Cancer
- Rare, usually slow-growing
- More prevalent in women (20-60 years old)
- Risk factors: Low iodine, radiation exposure
- Types:
- Papillary carcinoma: Develops in one lobe and spreads to lymph nodes
- Follicular carcinoma: Spreads to lungs and bones
- Treatment: Surgery, radioactive iodine, chemotherapy, radiation
Parathyroid Gland
- Two glands on each lobe of the thyroid.
- Secretes parathyroid hormone (PTH).
- Manages calcium levels: If calcium levels are low, PTH releases calcium from bones and absorbs it from the GI tract.
- Hyperparathyroidism: too much PTH production.
- Primary: Tumor in one or both glands. Symptoms may include thirst, frequent urination, high blood pressure, heartburn, confusion, kidney stones, and joint pain.
- Secondary: Low calcium levels in the blood. Common causes are low vitamin D and kidney diseases which affect phosphate
- HYPOparathyroidism: decreased PTH secretion, leads to hypocalcemia (low calcium levels), increased phosphate, and tetany (muscle spasms)
- Causes: Iatrogenic (accidental removal during thyroidectomy), hypovolemia and infarction of parathyroid, scar tissue, tumors, Low vitamin D Deficiency.
- Symptoms: Irritable, anxiety, agitation, increased osteoclast activity, spasms of respiratory muscles.
- Diagnosis: PTH levels, electrolytes, X-rays,
- Treatment: IV calcium if tetanic, vitamin D supplements, medications.
Adrenal Gland
- Located in each kidney, outer cortex and inner medulla
- Adrenal Cortex: Secretes mineralocorticoids (aldosterone- regulates blood pressure, sodium and potassium balance), glucocorticoids (cortisol-affects metabolism, response to stress, inflammation), androgens (testosterone, estrogen, progesterone)
- Adrenal Medulla: Secretes epinephrine, increasing heart rate, contractility, blood pressure, blood glucose
Adrenal Insufficiency (Addison's Disease)
- Cause is a drop in the secretion of cortisol (glucocorticoid) and aldosterone (mineralocorticoid)
- Possible etiologies: TB complications, autoimmune diseases, radiation, neoplasm, infections.
- Risk factors: Surgery, pregnancy, trauma, infection
- Pathogenesis: Hypoglycemia, weakness, hypotension, nausea, emotional lability, paranoia, increased skin pigmentation
- Diagnosis: Cortisol levels
- Treatment: Corticosteroids
- Prognosis: Untreated cases are usually fatal
- Physical Therapy Implications: Aquatic therapy may be contraindicated, because heat/humidity of the pool environment requires more cortisol, adrenal gland cannot regulate body temperature sufficiently
Secondary Adrenal Insufficiency
- Causes: Tumors in hypothalamus or pituitary, rapid taper of corticosteroids
- Symptoms: Arthralgia, myalgia, tendon calcification
- Treatment: ACTH replacement, managing fluid/electrolyte balances
Cushing Syndrome
- Increased cortisol levels, resulting from adrenal gland tumors or high-dose steroid treatments
- Symptoms: Muscle loss (amino acids), stretch marks, decreased wound healing, thin skin, muscle weakness, osteoporosis, fractures, Cushingoid face, increased weight, hair growth, buffalo hump
- Physical Therapy Implications: Adverse effects of corticosteroid treatment such as changes in sleep/mood, GI irritation, hyperglycemia, and fluid retention.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.