Podcast
Questions and Answers
Which characteristic would LEAST likely be associated with E. coli?
Which characteristic would LEAST likely be associated with E. coli?
- Oxidase-positive (correct)
- Gram-negative
- Colon microbiome member
- Facultative anaerobe
In the context of E. coli, what is the significance of serotyping?
In the context of E. coli, what is the significance of serotyping?
- Determining the presence of specific virulence factors such as toxins.
- Classifying strains based on antibiotic resistance patterns.
- Differentiating strains based on their O-antigen. (correct)
- Identifying strains capable of fermenting specific sugars.
How does phase variation contribute to the virulence of E. coli?
How does phase variation contribute to the virulence of E. coli?
- Increasing the rate of horizontal gene transfer to acquire new antibiotic resistance genes.
- Modifying surface antigens to evade host immune responses. (correct)
- Enhancing the production of endotoxins to induce stronger inflammatory responses.
- Improving the efficiency of iron acquisition from the host environment.
What is the primary role of siderophores in E. coli infections?
What is the primary role of siderophores in E. coli infections?
What is the role of the K1 capsular antigen in Neonatal Meningitis-causing E. coli (NMEC)?
What is the role of the K1 capsular antigen in Neonatal Meningitis-causing E. coli (NMEC)?
Which of the following is the most accurate description of how E. coli acquires virulence factors?
Which of the following is the most accurate description of how E. coli acquires virulence factors?
Which characteristic makes antibiotic treatment of E. coli infections particularly challenging?
Which characteristic makes antibiotic treatment of E. coli infections particularly challenging?
What is the primary mechanism by which E. coli endotoxin exerts its effects on the host?
What is the primary mechanism by which E. coli endotoxin exerts its effects on the host?
Why are Eosin Methylene Blue (EMB) agar and MacConkey's agar used in microbiology?
Why are Eosin Methylene Blue (EMB) agar and MacConkey's agar used in microbiology?
What is the direct function of Type III secretion systems in E. coli?
What is the direct function of Type III secretion systems in E. coli?
How does the presence of E. coli in soil and water primarily occur?
How does the presence of E. coli in soil and water primarily occur?
In the context of E. coli infections, what does the term 'opportunistic pathogen' refer to?
In the context of E. coli infections, what does the term 'opportunistic pathogen' refer to?
What is the significance of flagellar motility for E. coli?
What is the significance of flagellar motility for E. coli?
How does E. coli's ability to ferment lactose affect its identification on MacConkey's agar?
How does E. coli's ability to ferment lactose affect its identification on MacConkey's agar?
In the context of urinary tract infections caused by Uropathogenic E. coli (UPEC), what is the role of hemolysin A?
In the context of urinary tract infections caused by Uropathogenic E. coli (UPEC), what is the role of hemolysin A?
Why are strains of Uropathogenic E. coli (UPEC) that lack certain virulence factors easily removed from the body in the urine?
Why are strains of Uropathogenic E. coli (UPEC) that lack certain virulence factors easily removed from the body in the urine?
Which of the following is a common source of intestinal pathogenic E. coli (IPEC) that leads to gastroenteritis?
Which of the following is a common source of intestinal pathogenic E. coli (IPEC) that leads to gastroenteritis?
In the context of ExPEC, what is the general meaning of "Extraintestinal"?
In the context of ExPEC, what is the general meaning of "Extraintestinal"?
What is the relevance of E. coli being a facultative anaerobe for its survival and pathogenicity?
What is the relevance of E. coli being a facultative anaerobe for its survival and pathogenicity?
Which of the following is a common characteristic of coliforms, including E. coli, that is used in water quality testing?
Which of the following is a common characteristic of coliforms, including E. coli, that is used in water quality testing?
How do alterations in surface antigens allow E. coli to adjust energy expenditure according to environmental factors, contributing to its survival?
How do alterations in surface antigens allow E. coli to adjust energy expenditure according to environmental factors, contributing to its survival?
How does E. coli's rapid growth and simple nutritional requirements contribute to its ability to cause infections?
How does E. coli's rapid growth and simple nutritional requirements contribute to its ability to cause infections?
Septicemia, in the context of E. coli infections, is most likely to occur under which of the following conditions?
Septicemia, in the context of E. coli infections, is most likely to occur under which of the following conditions?
What is the commonality among plasmids, bacteriophages, and pathogenicity islands in the context of E. coli virulence?
What is the commonality among plasmids, bacteriophages, and pathogenicity islands in the context of E. coli virulence?
Which of the following factors is LEAST likely to contribute to the ability of E. coli to cause disease?
Which of the following factors is LEAST likely to contribute to the ability of E. coli to cause disease?
Which media type is most effective in the identification of lactose-fermenting coliforms?
Which media type is most effective in the identification of lactose-fermenting coliforms?
How do virulence factors influence the pathogenesis in different pathotypes of E. coli?
How do virulence factors influence the pathogenesis in different pathotypes of E. coli?
What describes the pathogenic mechanism of E. coli strains causing gastroenteritis?
What describes the pathogenic mechanism of E. coli strains causing gastroenteritis?
In the context of ExPEC infections, which of the following environments is most susceptible?
In the context of ExPEC infections, which of the following environments is most susceptible?
Flashcards
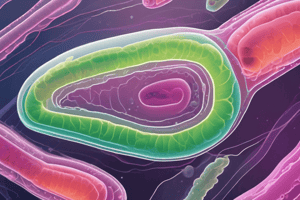
E. coli
E. coli
Common members of the colon microbiome, residing in the intestines of animals and humans, making them "enteric" bacteria.
Endogenous E. coli Infection
Endogenous E. coli Infection
Infections caused by strains transferred to new anatomical niches within the same organism.
Exogenous E. coli Infection
Exogenous E. coli Infection
Infections caused by pathogenic strains from external sources like contaminated soil or water.
E. coli Pilus
E. coli Pilus
Signup and view all the flashcards
E. coli Flagella motility
E. coli Flagella motility
Signup and view all the flashcards
Coliforms
Coliforms
Signup and view all the flashcards
EMB and MacConkey's agar
EMB and MacConkey's agar
Signup and view all the flashcards
E. coli Endotoxin
E. coli Endotoxin
Signup and view all the flashcards
E. coli Exotoxins/Adhesins
E. coli Exotoxins/Adhesins
Signup and view all the flashcards
Antibiotic resistance in E. coli
Antibiotic resistance in E. coli
Signup and view all the flashcards
Siderophores
Siderophores
Signup and view all the flashcards
Uropathogenic E. coli (UPEC)
Uropathogenic E. coli (UPEC)
Signup and view all the flashcards
Type 1 and P pili
Type 1 and P pili
Signup and view all the flashcards
Hemolysin A
Hemolysin A
Signup and view all the flashcards
Neonatal Meningitis-causing E. coli (NMEC)
Neonatal Meningitis-causing E. coli (NMEC)
Signup and view all the flashcards
E. coli Septicemia
E. coli Septicemia
Signup and view all the flashcards
Intestinal Pathogenic E. coli (IPEC)
Intestinal Pathogenic E. coli (IPEC)
Signup and view all the flashcards
Study Notes
- E. coli are common members of the colon microbiome and reside in the intestines of animals and humans, classifying them as "enteric" bacteria.
- E. coli can cause endogenous infections upon transfer to new anatomical niches and exogenous infections through ingestion of pathogenic strains found in soil and water due to fecal contamination.
- E. coli utilize pili for adhesion and biofilm formation, flagellar motility for movement, grow rapidly, and have simple nutritional needs.
- E. coli are facultative anaerobes, catalase-positive, oxidase-negative, reduce nitrate, and ferment glucose and lactose, classifying them as coliforms that are Gram-negative enteric lactose fermenters.
- Selective media like Eosin methylene blue agar and MacConkey's agar inhibit Gram-positive bacterial growth and indicate acid production from lactose fermentation, used to identify coliforms.
- EMB agar indicates lactose fermentation and strong acid production through a greenish hue, while MacConkey's agar indicates E. coli lactose fermentation via a pinkish-purple color.
- Virulence factors in E. coli are acquired via horizontal gene transfer of plasmids, bacteriophages, and pathogenicity islands.
- E. coli endotoxin, a heat-stable lipopolysaccharide, triggers inflammatory responses, disseminated intravascular coagulation, and hypovolemic shock via its A-antigen.
- The core polysaccharide of E. coli endotoxin is common to all Enterobacteriaceae, while the O-antigen classifies E. coli serotypes.
- Exotoxins in E. coli promote cell death or fluid loss, and adhesins are present on pili, fimbriae, or strain-specific surface antigens.
- Type III secretion systems in E. coli inject virulence effector proteins into host cells, promoting attachment, invasion, and cell destruction.
- Phase variation alters the expression of O, K, and flagellar H antigens and pili in E. coli, allowing immune evasion and energy expenditure adjustment.
- Antibiotic resistance in E. coli is rapidly spread via HGT, making treatments difficult, while siderophores acquire iron for bacterial growth, and polysaccharide capsules repel phagocytes to avoid serum killing.
- Extraintestinal pathogenic E. coli (ExPEC) are commensals that act as opportunistic pathogens in new anatomical sites.
Urinary Tract Infections
- Uropathic E. coli (UPEC) causes most urinary tract infections through Type 1 and P pili and Dr fimbriae attaching to urothelium
- Hemolysin A in UPEC causes cell damage, facilitating bacterial movement, while strains lacking these virulence factors are easily removed in urine.
Neonatal Meningitis
- E. coli is the second most common cause of bacterial neonatal meningitis
- Neonatal Meningitis-causing E. coli (NMEC) have special virulence factors enabling translocation across the blood-brain barrier, including Type I pili and Outer Membrane Protein A (OmpA) attaching to brain microvascular endothelial cells.
- Ibe proteins, CNF1, and other mediators facilitate NMEC invasion of the blood-brain barrier, while K1 capsular antigens are thought to prevent lysosome fusion, allowing live bacteria to move across the barrier.
Septicemia
- Septicemia occurs when urinary or gastrointestinal tract infections spread to the blood, potentially occurring due to abdominal trauma.
Gastroenteritis
- Intestinal Pathogenic E. coli (IPEC) infection follows ingestion of contaminated food or water potentially from human or animal feces.
- The pathotypes can affect the small and/or large intestine; Enteropathogenic and Enterotoxigenic E. coli for the small intestine, Enteroaggregative E. coli for both, and Enteroinvasive E. coli for the large intestine.
- Shiga toxin-producing E. coli virulence factors affect each pathotype determine the pathogenesis of infection.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.