Podcast
Questions and Answers
Explain the fundamental difference between the direct tube method and the indirect tube method in ABO blood grouping, highlighting their respective target molecules.
Explain the fundamental difference between the direct tube method and the indirect tube method in ABO blood grouping, highlighting their respective target molecules.
The direct tube method directly identifies the presence of A and B antigens on red blood cells (RBCs) by reacting them with anti-A and anti-B reagents. The indirect tube method, on the other hand, identifies antibodies in serum or plasma by mixing the patient's serum/plasma with known group O red blood cells and detecting the presence of agglutinins, which are antibodies targeting A or B antigens.
Describe the role of agglutination in both the direct and indirect tube methods, emphasizing its significance in interpreting results.
Describe the role of agglutination in both the direct and indirect tube methods, emphasizing its significance in interpreting results.
Agglutination, or clumping, is a crucial indicator in both methods. In the direct method, agglutination signifies the presence of A or B antigens on the RBCs when they react with the corresponding anti-A or anti-B reagents. In the indirect method, agglutination indicates the presence of antibodies (agglutinins) in the serum/plasma when it reacts with the known group O red blood cells, suggesting the possibility of transfusion incompatibility or HDFN.
What are the key considerations for ensuring accurate results in the direct tube method, emphasizing the importance of quality control?
What are the key considerations for ensuring accurate results in the direct tube method, emphasizing the importance of quality control?
Accurate results in the direct tube method require adherence to specific guidelines. These include using commercially prepared, highly specific monoclonal antisera, diluting the reagents correctly according to the manufacturer's instructions, maintaining proper temperature control during testing, and carefully interpreting the degree of agglutination. Weak reactions deserve specific attention, and proper control measures are crucial for minimizing false results.
Why is the indirect tube method essential for blood transfusion compatibility testing, and how is it used to achieve this goal?
Why is the indirect tube method essential for blood transfusion compatibility testing, and how is it used to achieve this goal?
Describe the importance of using a carefully selected panel of group O red blood cells in the indirect tube method, and explain why this is crucial for the test's accuracy.
Describe the importance of using a carefully selected panel of group O red blood cells in the indirect tube method, and explain why this is crucial for the test's accuracy.
What are the key differences in the reagents used in the direct and indirect tube methods and how do these differences relate to the specific goals of each method?
What are the key differences in the reagents used in the direct and indirect tube methods and how do these differences relate to the specific goals of each method?
Compare and contrast the results analysis in the direct and indirect tube methods, highlighting the indicators of positive and negative reactions in each method.
Compare and contrast the results analysis in the direct and indirect tube methods, highlighting the indicators of positive and negative reactions in each method.
Flashcards
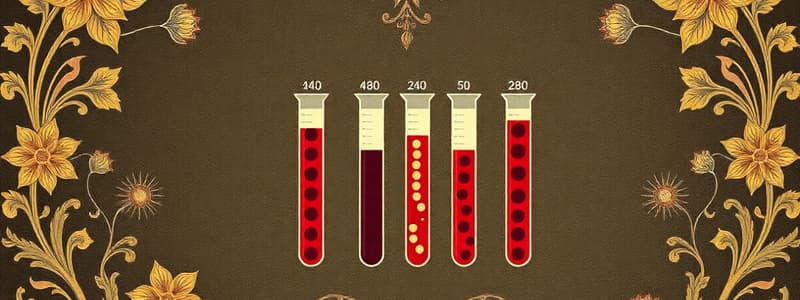
Direct Tube Method
Direct Tube Method
A procedure for ABO blood grouping by adding anti-A and anti-B reagents to RBC sample.
Agglutination
Agglutination
The clumping of red blood cells indicating the presence of antigens or antibodies.
Anti-A Reagent
Anti-A Reagent
A substance that reacts with A antigens on RBCs to indicate positive agglutination.
Anti-B Reagent
Anti-B Reagent
Signup and view all the flashcards
Indirect Tube Method
Indirect Tube Method
Signup and view all the flashcards
Hemolytic Disease of the Newborn (HDFN)
Hemolytic Disease of the Newborn (HDFN)
Signup and view all the flashcards
Reagents Dilution
Reagents Dilution
Signup and view all the flashcards
Temperature Control
Temperature Control
Signup and view all the flashcards
Study Notes
Direct Tube Method
- This method is a standard procedure for ABO blood grouping.
- It involves the direct addition of anti-A and anti-B reagents to a drop of the patient's red blood cell (RBC) sample.
- Agglutination (clumping) or lack thereof indicates the presence or absence of A or B antigens on the RBCs.
- Positive agglutination with anti-A indicates the presence of A antigen, while anti-B indicates the presence of B antigen.
- Lack of agglutination with either reagent means the corresponding antigen is not present.
- The direct method is suitable for routine testing and is relatively fast.
- It utilizes commercially prepared antisera (anti-A and anti-B). These are typically monoclonal antibodies which are highly specific for A and B antigens, resulting in reduced chances of false results.
- A positive reaction should be evaluated for the degree of agglutination. Weak reactions are often observed in certain patient populations, and require careful attention to detail.
- Reagents must be diluted appropriately according to the manufacturer’s instructions. Incorrect dilutions can lead to incorrect results.
- Proper control of temperature during testing is important.
Indirect Tube Method
- This method is used primarily for identification of antibody in plasma or serum.
- It is not used for determining the ABO antigens on the RBCs as that is done using the direct tube method.
- The patient's serum or plasma is mixed with a panel of known group O red blood cells.
- Presence of agglutinins (antibodies) against A or B will cause agglutination of the group O red blood cells in the test tube.
- This method is most suited for detecting antibodies.
- It is essential in cases of predicting potential transfusion incompatibility and managing patients with hemolytic disease of the newborn (HDFN).
- The reagents include O group red blood cells and patient's serum.
- The panel of group O red blood cells should be carefully selected to ensure detection of any possible antibody against A or B antigens.
- The principle is based on the reaction between red blood cell antigens and their corresponding antibodies. A positive reaction demonstrates the presence of antibodies in the patient's serum.
- Results analysis is crucial. Carefully examine for hemolysis or agglutination.
- Proper control of temperature is equally important as in the direct method.
- The indirect method is used for antibody screening and matching before blood transfusion.
- It is less commonly used in routine ABO grouping.
- Both methods should be accompanied by appropriate controls (e.g., positive and negative controls) to ensure the validity of test results.
- If any inconsistencies are found in the testing process or control, repeat the test or seek additional investigation.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.