Podcast
Questions and Answers
What is the primary function of the pharyngeal phase of swallowing?
What is the primary function of the pharyngeal phase of swallowing?
- Lubricating the food bolus
- Elevating the soft palate to allow airflow
- Initiating peristalsis in the esophagus
- Preventing food entry into the airway (correct)
Which type of digestion primarily occurs in the stomach?
Which type of digestion primarily occurs in the stomach?
- Chemical digestion
- Both mechanical and chemical digestion (correct)
- Absorption of nutrients
- Mechanical digestion
What role does bile play in lipid digestion?
What role does bile play in lipid digestion?
- It protects the stomach lining during lipid digestion
- It directly breaks down lipids into fatty acids
- It serves as an enzyme to digest carbohydrates
- It emulsifies fats to facilitate their breakdown (correct)
At which point does carbohydrate digestion begin?
At which point does carbohydrate digestion begin?
What is the primary method by which food is propelled through the digestive tract?
What is the primary method by which food is propelled through the digestive tract?
Which layer of the alimentary canal is the innermost layer that contains mucous epithelium?
Which layer of the alimentary canal is the innermost layer that contains mucous epithelium?
What is the primary function of mesenteries in the digestive system?
What is the primary function of mesenteries in the digestive system?
Which of the following structures is not part of the digestive tract?
Which of the following structures is not part of the digestive tract?
What is the role of the myenteric plexus found in the muscularis layer?
What is the role of the myenteric plexus found in the muscularis layer?
Which accessory organ of the digestive system is the largest internal organ?
Which accessory organ of the digestive system is the largest internal organ?
What is the function of the visceral peritoneum in the digestive system?
What is the function of the visceral peritoneum in the digestive system?
Which structure connects the lesser curvature of the stomach to the liver?
Which structure connects the lesser curvature of the stomach to the liver?
The muscularis layer of the alimentary canal typically consists of how many layers?
The muscularis layer of the alimentary canal typically consists of how many layers?
What is the primary function of the hepatic portal vein?
What is the primary function of the hepatic portal vein?
Which component of the liver aids in detoxification by removing old blood cells and bacteria?
Which component of the liver aids in detoxification by removing old blood cells and bacteria?
Which of the following accurately describes the role of bile produced by the liver?
Which of the following accurately describes the role of bile produced by the liver?
What triggers the contraction of the gallbladder to release bile?
What triggers the contraction of the gallbladder to release bile?
What is the correct pathway of bile from the liver to the duodenum?
What is the correct pathway of bile from the liver to the duodenum?
Which of the following is NOT a function of the liver?
Which of the following is NOT a function of the liver?
What is the role of the Kupffer cells in the liver?
What is the role of the Kupffer cells in the liver?
Which type of teeth is primarily responsible for grinding food during mastication?
Which type of teeth is primarily responsible for grinding food during mastication?
Flashcards are hidden until you start studying
Study Notes
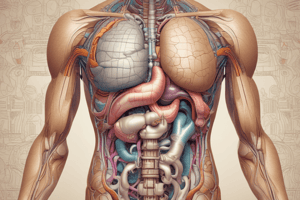
Digestive System Overview
- Digestive System comprises the digestive tract (alimentary canal) & accessory organs
- Digestive tract is a continuous tube from mouth to anus
- Accessory organs (liver, pancreas, gallbladder) aid in digestion & absorption but are located outside the GI tract
Digestive Tract Structure
- Main parts: oral cavity, pharynx, esophagus, stomach, small intestine, large intestine, anus
- Layers: mucosa (innermost), submucosa, muscularis, serosa (outermost)
- Mucosa contains: mucous epithelium, lamina propria, muscularis mucosa
- Submucosa contains: blood vessels, nerves, lymphatics & submucosal plexus (nerve cells stimulating gland secretion)
- Muscularis contains: two layers (inner circular & outer longitudinal except in stomach) & myenteric plexus (controls motility)
- Serosa is part of the peritoneum (visceral peritoneum)
Peritoneum
- Visceral Peritoneum covers organs
- Parietal Peritoneum lines body wall
- Retroperitoneal organs (e.g., kidneys, pancreas) are covered by peritoneum on one surface
Mesenteries
- Functions
- Hold abdominal organs in place
- Serve as pathways for vessels & nerves
- Types
- Lesser omentum: Connects the lesser curvature of the stomach to the liver and diaphragm
- Greater omentum: Connects the greater curvature of the stomach to the transverse colon; stores fat
Oral Cavity Structures
- Lips (Labia): protect anterior mouth opening; orbicularis oris muscle
- Cheeks: form lateral walls; buccinator muscle
- Hard palate: anterior roof
- Soft palate: posterior roof
- Uvula: fleshy projection at the back of the soft palate
- Tongue: large muscular organ, attached at the back, free at the front
Liver
- General Characteristics
- Largest internal organ (~1.36 kg)
- Located in the right upper quadrant, inferior to the diaphragm
- Composed of four lobes (two major – right & left, separated by the falciform ligament; two minor – caudate & quadrate visible from the posterior side)
- Contains a portal (porta hepatis) for vessels, ducts, and nerves
- Blood Supply
- Hepatic Artery: Delivers oxygenated blood
- Hepatic Portal Vein: Carries nutrient-rich blood from the digestive tract
- Hepatic Veins: Drain deoxygenated blood from the liver to the inferior vena cava
- Liver Structure
- Hepatic Cords: Composed of hepatocytes; radiating from the central vein
- Hepatic Sinusoids: Found between cords; containing phagocytic Kupffer cells for detoxification
- Bile Canaliculi: Transport bile from hepatocytes to the hepatic duct
- Functions
- Bile Production: 600-1000 ml/day; neutralizes stomach acid; emulsifies fats
- Storage: Glycogen, lipids, vitamins, copper, and iron
- Synthesis: Blood proteins (albumins, fibrinogen, globulins, heparin, clotting factors)
- Nutrient Conversion: Converts amino acids to glucose; activates vitamin D
- Detoxification: Converts toxic ammonia to urea for excretion
- Phagocytosis: Kupffer cells remove old blood cells and bacteria
Gallbladder
- Location: Small sac on the liver's inferior surface
- Function: Stores and concentrates bile produced by the liver
- Bile Flow: Exits via the cystic duct; joins with the common hepatic duct to form the common bile duct, which leads to the duodenum
- Stimulation: Cholecystokinin triggers gallbladder contraction to release bile during digestion
- Concentration: Bile becomes more effective when concentrated but can form stones if overly dehydrated
Bile Pathway
- Production: In the liver
- Flow: Right/left hepatic ducts → common hepatic duct → cystic duct (for storage in the gallbladder)
- Release: From the gallbladder via the cystic duct to the common bile duct and then to the duodenum during digestion
Digestive System Functions and Activities
- Ingestion: The process of taking food into the mouth (oral cavity)
- Mastication (Chewing): Breakdown of large particles via mechanical digestion to aid chemical digestion.
- Teeth Roles:
- Incisors and canines: Cut food
- Molars: Grind food.
- Muscles Involved: Masseter, temporalis, medial pterygoid, lateral pterygoid (depresses mandible, opens jaw)
- Teeth Roles:
- Swallowing (Deglutition): Movement of bolus (food/liquid) from the mouth to the esophagus.
- Phases:
- Voluntary Phase: Tongue moves bolus to pharynx
- Pharyngeal Phase: Controlled by the medulla oblongata; soft palate elevates, upper esophageal sphincter relaxes, epiglottis tips to prevent food entry into the airway
- Esophageal Phase: Peristalsis moves bolus to the stomach
- Phases:
- Propulsion: Movement of food through the digestive tract (~24-36 hours).
- Peristalsis: Alternating contractions push food
- Mass Movements: Strong contractions in the large intestine moving contents to the anus
- Mixing: Segmental contractions mix food with secretions to form chyme in the small intestine
- Secretions:
- Mucus: Lubricates & protects the GI tract
- Water: Aids in food liquefaction for digestion/absorption
- Bile: Emulsifies fats for digestion
- Enzymes: Break down food chemically
- Digestion Types:
- Mechanical Digestion: Physical breakdown (e.g., chewing, stomach churning, segmentation)
- Chemical Digestion: Enzyme-driven breakdown (e.g., carbohydrates to glucose)
- Carbohydrate Digestion:
- Starts in the mouth with salivary amylase, continues in the duodenum with pancreatic amylase, and completes with disaccharidases breaking down into monosaccharides.
- Lipid Digestion:
- Limited activity in the mouth/stomach due to lack of emulsification.
- Bile in the duodenum facilitates breakdown by pancreatic lipase into fatty acids and monoglycerides.
- Protein Digestion:
- Starts in the stomach with pepsin.
- Pancreatic enzymes (trypsin, chymotrypsin, carboxypeptidase) act in the small intestine, breaking proteins into peptides and further into amino acids by peptidases.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.