Podcast
Questions and Answers
Why is lingual lipase particularly important in neonates?
Why is lingual lipase particularly important in neonates?
- It effectively neutralizes the higher stomach acid levels common in neonates.
- It rapidly accelerates fat absorption in the small intestine, meeting the high energy demands of neonates.
- It compensates for the immature digestive systems and reduced pancreatic activity typical of neonates. (correct)
- It facilitates the digestion of complex carbohydrates, which are abundant in neonatal diets.
How does radiation treatment lead to xerostomia?
How does radiation treatment lead to xerostomia?
- By selectively destroying the amylase-producing cells in the salivary glands.
- By causing inflammation and swelling that obstruct the salivary ducts.
- By directly affecting the central nervous system's control of salivary gland secretion.
- By causing direct damage to the salivary glands, impairing their secretory function. (correct)
What is the primary reason tooth decay is often a consequence of xerostomia?
What is the primary reason tooth decay is often a consequence of xerostomia?
- Decreased saliva reduces the buffering capacity and clearance of acids produced by oral bacteria. (correct)
- Reduced saliva leads to increased production of enamel-degrading enzymes by oral bacteria.
- Dry mouth prevents the proper metabolism of sugars, leading to acid build-up.
- The lack of saliva causes an increase in oral pH, which promotes the dissolution of tooth enamel.
What is the initial trigger that begins the swallowing process?
What is the initial trigger that begins the swallowing process?
Why is it important that blood from the intestinal tract goes to the liver via the portal vein before entering systemic circulation?
Why is it important that blood from the intestinal tract goes to the liver via the portal vein before entering systemic circulation?
During swallowing, what is the role of the epiglottis?
During swallowing, what is the role of the epiglottis?
The liver receives blood from which two sources?
The liver receives blood from which two sources?
Which characteristic is unique to the esophagus?
Which characteristic is unique to the esophagus?
Which of the following best describes why amylase and lingual lipase may become more important during pathological conditions?
Which of the following best describes why amylase and lingual lipase may become more important during pathological conditions?
How does the proportion of arterial blood to the liver change after eating, and why?
How does the proportion of arterial blood to the liver change after eating, and why?
How does the liver's blood perfusion differ from most organs in the systemic circulation?
How does the liver's blood perfusion differ from most organs in the systemic circulation?
A patient undergoing radiation treatment for head and neck cancer experiences significant xerostomia. Besides frequent sips of water, what other treatment would be MOST beneficial?
A patient undergoing radiation treatment for head and neck cancer experiences significant xerostomia. Besides frequent sips of water, what other treatment would be MOST beneficial?
A medication is metabolized in the liver. Which route of administration would likely result in the highest first-pass metabolism?
A medication is metabolized in the liver. Which route of administration would likely result in the highest first-pass metabolism?
A patient reports difficulty swallowing solids and frequent heartburn. Endoscopy reveals erosions in the lower esophagus. What is MOST likely contributing to these erosions?
A patient reports difficulty swallowing solids and frequent heartburn. Endoscopy reveals erosions in the lower esophagus. What is MOST likely contributing to these erosions?
During the pharyngeal phase of swallowing, several actions occur in rapid succession. Which of the following actions happens FIRST?
During the pharyngeal phase of swallowing, several actions occur in rapid succession. Which of the following actions happens FIRST?
Which of the following is the MOST likely mechanism by which non-steroidal anti-inflammatory drugs (NSAIDs) contribute to the formation of peptic ulcers?
Which of the following is the MOST likely mechanism by which non-steroidal anti-inflammatory drugs (NSAIDs) contribute to the formation of peptic ulcers?
If a patient has impaired liver function, how might this affect drug dosages, and why?
If a patient has impaired liver function, how might this affect drug dosages, and why?
What is the primary role of the liver with respect to blood coming directly from the digestive organs?
What is the primary role of the liver with respect to blood coming directly from the digestive organs?
A patient is diagnosed with a peptic ulcer and Helicobacter pylori infection. What is the MOST appropriate initial treatment?
A patient is diagnosed with a peptic ulcer and Helicobacter pylori infection. What is the MOST appropriate initial treatment?
Following a partial gastrectomy (removal of part of the stomach), which physiological consequence is MOST likely to occur?
Following a partial gastrectomy (removal of part of the stomach), which physiological consequence is MOST likely to occur?
What are the two main categories of gastrointestinal (GI) processes that are regulated?
What are the two main categories of gastrointestinal (GI) processes that are regulated?
A patient with a history of chronic NSAID use develops an ulcer. What is the PRIMARY reason NSAIDs increase the risk of ulcer formation?
A patient with a history of chronic NSAID use develops an ulcer. What is the PRIMARY reason NSAIDs increase the risk of ulcer formation?
A patient is prescribed a medication that selectively blocks histamine H2 receptors in the stomach. What is the MOST likely therapeutic outcome?
A patient is prescribed a medication that selectively blocks histamine H2 receptors in the stomach. What is the MOST likely therapeutic outcome?
What is the primary function of the Sphincter of Oddi?
What is the primary function of the Sphincter of Oddi?
Which of the following best describes the function of acinar cells in the pancreas?
Which of the following best describes the function of acinar cells in the pancreas?
In what form are proteolytic enzymes secreted by the pancreas, and where are they activated?
In what form are proteolytic enzymes secreted by the pancreas, and where are they activated?
What characteristic of pancreatic juice contributes to its isotonic nature?
What characteristic of pancreatic juice contributes to its isotonic nature?
If the pancreatic duct were blocked, which of the following processes would be most directly affected?
If the pancreatic duct were blocked, which of the following processes would be most directly affected?
What is the primary role of bicarbonate secreted by pancreatic ductal cells?
What is the primary role of bicarbonate secreted by pancreatic ductal cells?
Which of the following is a key difference between the exocrine and endocrine functions of the pancreas?
Which of the following is a key difference between the exocrine and endocrine functions of the pancreas?
How does the production of HCO3- by pancreatic duct cells help in maintaining the pH balance in the digestive system?
How does the production of HCO3- by pancreatic duct cells help in maintaining the pH balance in the digestive system?
Which type of chemical messenger regulation involves a hormone traveling through the bloodstream to reach a distant target cell?
Which type of chemical messenger regulation involves a hormone traveling through the bloodstream to reach a distant target cell?
A researcher is studying a cell in the gastric pit that releases a substance affecting only its own activity. This is characteristic of what kind of regulation?
A researcher is studying a cell in the gastric pit that releases a substance affecting only its own activity. This is characteristic of what kind of regulation?
Following a meal, enteroendocrine cells in the small intestine release a hormone into the lamina propria. What is the primary destination of this hormone?
Following a meal, enteroendocrine cells in the small intestine release a hormone into the lamina propria. What is the primary destination of this hormone?
Cholecystokinin (CCK) release is stimulated by the presence of fatty acids and amino acids in the small intestine. What is a primary effect of CCK?
Cholecystokinin (CCK) release is stimulated by the presence of fatty acids and amino acids in the small intestine. What is a primary effect of CCK?
Which of the following control system loops describes the regulation of CCK secretion?
Which of the following control system loops describes the regulation of CCK secretion?
What is the primary function of peristalsis in the intestinal tract?
What is the primary function of peristalsis in the intestinal tract?
Segmentation primarily occurs in the small intestine and is characterized by what type of movement?
Segmentation primarily occurs in the small intestine and is characterized by what type of movement?
Pacemaker cells in the GIT generate spontaneous depolarization-repolarization cycles known as slow waves. What is the direct result of these slow waves in the absence of neural or hormonal input?
Pacemaker cells in the GIT generate spontaneous depolarization-repolarization cycles known as slow waves. What is the direct result of these slow waves in the absence of neural or hormonal input?
How does excitatory input affect the slow waves of the basic electrical rhythm in the gastrointestinal tract?
How does excitatory input affect the slow waves of the basic electrical rhythm in the gastrointestinal tract?
Which of the following statements accurately describes the relationship between action potential frequency and muscle contraction in the GIT?
Which of the following statements accurately describes the relationship between action potential frequency and muscle contraction in the GIT?
During which phase of gastrointestinal control are reflexes initiated by the sight, smell, or taste of food?
During which phase of gastrointestinal control are reflexes initiated by the sight, smell, or taste of food?
Distension, acidity, and digestive products in the intestine primarily stimulate which phase of gastrointestinal control?
Distension, acidity, and digestive products in the intestine primarily stimulate which phase of gastrointestinal control?
Activation of the satiety center in the ventromedial region of the hypothalamus leads to which outcome?
Activation of the satiety center in the ventromedial region of the hypothalamus leads to which outcome?
Neuropeptide Y and ghrelin share what common effect on food intake?
Neuropeptide Y and ghrelin share what common effect on food intake?
During fasting, which hormone is synthesized and released from endocrine cells in the stomach to stimulate hunger?
During fasting, which hormone is synthesized and released from endocrine cells in the stomach to stimulate hunger?
Which of the following is the primary function of the stratified squamous epithelium in the esophagus?
Which of the following is the primary function of the stratified squamous epithelium in the esophagus?
What is the primary mechanism that propels a food bolus through the esophagus during swallowing?
What is the primary mechanism that propels a food bolus through the esophagus during swallowing?
How does the lower esophageal sphincter (LES) primarily prevent gastric reflux?
How does the lower esophageal sphincter (LES) primarily prevent gastric reflux?
If the lower esophageal sphincter (LES) malfunctions, which of the following conditions is most likely to occur?
If the lower esophageal sphincter (LES) malfunctions, which of the following conditions is most likely to occur?
Which of the following is a function of the stomach?
Which of the following is a function of the stomach?
What is the role of hydrochloric acid (HCl) in the stomach?
What is the role of hydrochloric acid (HCl) in the stomach?
Which substance secreted by the stomach is essential for the absorption of vitamin B12 in the ileum?
Which substance secreted by the stomach is essential for the absorption of vitamin B12 in the ileum?
Which region of the stomach is characterized by a thicker smooth muscle layer primarily responsible for the physical breakdown of food?
Which region of the stomach is characterized by a thicker smooth muscle layer primarily responsible for the physical breakdown of food?
In the stomach, mucus secretion serves which critical function?
In the stomach, mucus secretion serves which critical function?
Where are parietal cells primarily located within the stomach, and what do they secrete?
Where are parietal cells primarily located within the stomach, and what do they secrete?
What is the primary function of enteroendocrine cells (G cells) in the gastric glands?
What is the primary function of enteroendocrine cells (G cells) in the gastric glands?
How does histamine, secreted by ECL cells, contribute to gastric acid secretion?
How does histamine, secreted by ECL cells, contribute to gastric acid secretion?
What is the role of the H+/K+ ATPase pump in parietal cells?
What is the role of the H+/K+ ATPase pump in parietal cells?
During the cephalic phase of gastric secretion, what is the primary mechanism by which the brain stimulates acid production in the stomach?
During the cephalic phase of gastric secretion, what is the primary mechanism by which the brain stimulates acid production in the stomach?
What is the primary effect of secretin and CCK, released during the intestinal phase of gastric secretion, on stomach activity?
What is the primary effect of secretin and CCK, released during the intestinal phase of gastric secretion, on stomach activity?
Flashcards
Portal Circulation
Portal Circulation
Circulation that carries blood from the intestinal tract directly to the liver.
Portal Blood Content
Portal Blood Content
Blood is nutrient-rich and contains substances from the digestive tract.
Liver's Role in Portal Circulation
Liver's Role in Portal Circulation
Removes harmful substances and processes nutrients from the blood.
Hepatic Artery
Hepatic Artery
Signup and view all the flashcards
Hepatic Portal Vein
Hepatic Portal Vein
Signup and view all the flashcards
Liver: In Series Circulation
Liver: In Series Circulation
Signup and view all the flashcards
GI Processes
GI Processes
Signup and view all the flashcards
GI Processes Regulation
GI Processes Regulation
Signup and view all the flashcards
What is peptic ulcer disease?
What is peptic ulcer disease?
Signup and view all the flashcards
What is the most common cause of ulcers?
What is the most common cause of ulcers?
Signup and view all the flashcards
Name non-bacterial ulcer factors.
Name non-bacterial ulcer factors.
Signup and view all the flashcards
How are ulcers treated?
How are ulcers treated?
Signup and view all the flashcards
Is the stomach essential for life?
Is the stomach essential for life?
Signup and view all the flashcards
Main Pancreatic Duct
Main Pancreatic Duct
Signup and view all the flashcards
Sphincter of Oddi
Sphincter of Oddi
Signup and view all the flashcards
Exocrine Pancreas
Exocrine Pancreas
Signup and view all the flashcards
Endocrine Pancreas
Endocrine Pancreas
Signup and view all the flashcards
Pancreatic Islets (Islets of Langerhans)
Pancreatic Islets (Islets of Langerhans)
Signup and view all the flashcards
Acinar Cells
Acinar Cells
Signup and view all the flashcards
Ductal Cells
Ductal Cells
Signup and view all the flashcards
Pancreatic Juice
Pancreatic Juice
Signup and view all the flashcards
Endocrine Regulation
Endocrine Regulation
Signup and view all the flashcards
Neurocrine Regulation
Neurocrine Regulation
Signup and view all the flashcards
Paracrine Regulation
Paracrine Regulation
Signup and view all the flashcards
Autocrine Regulation
Autocrine Regulation
Signup and view all the flashcards
Enteroendocrine Cells
Enteroendocrine Cells
Signup and view all the flashcards
Major GI Hormones
Major GI Hormones
Signup and view all the flashcards
Intestinal Motility
Intestinal Motility
Signup and view all the flashcards
Peristalsis
Peristalsis
Signup and view all the flashcards
Segmentation
Segmentation
Signup and view all the flashcards
Pacemaker Cells (GIT)
Pacemaker Cells (GIT)
Signup and view all the flashcards
Slow Waves (GIT)
Slow Waves (GIT)
Signup and view all the flashcards
Cephalic Phase
Cephalic Phase
Signup and view all the flashcards
Gastric Phase
Gastric Phase
Signup and view all the flashcards
Intestinal Phase
Intestinal Phase
Signup and view all the flashcards
Feeding Center
Feeding Center
Signup and view all the flashcards
Lingual lipase
Lingual lipase
Signup and view all the flashcards
Pancreatic secretions
Pancreatic secretions
Signup and view all the flashcards
Xerostomia
Xerostomia
Signup and view all the flashcards
Sjögren's syndrome
Sjögren's syndrome
Signup and view all the flashcards
Swallowing
Swallowing
Signup and view all the flashcards
Pharynx
Pharynx
Signup and view all the flashcards
Larynx
Larynx
Signup and view all the flashcards
Glottis
Glottis
Signup and view all the flashcards
Epiglottis
Epiglottis
Signup and view all the flashcards
Esophagus
Esophagus
Signup and view all the flashcards
Stratified Squamous Epithelium
Stratified Squamous Epithelium
Signup and view all the flashcards
Upper Esophageal Sphincter
Upper Esophageal Sphincter
Signup and view all the flashcards
Lower Esophageal Sphincter
Lower Esophageal Sphincter
Signup and view all the flashcards
Esophageal Peristalsis
Esophageal Peristalsis
Signup and view all the flashcards
Heartburn
Heartburn
Signup and view all the flashcards
Stomach
Stomach
Signup and view all the flashcards
Pepsin
Pepsin
Signup and view all the flashcards
Hydrochloric Acid (HCl)
Hydrochloric Acid (HCl)
Signup and view all the flashcards
Intrinsic Factor
Intrinsic Factor
Signup and view all the flashcards
Fundus and Body
Fundus and Body
Signup and view all the flashcards
Antrum
Antrum
Signup and view all the flashcards
Pyloric Sphincter
Pyloric Sphincter
Signup and view all the flashcards
Mucous Cells
Mucous Cells
Signup and view all the flashcards
Parietal Cells
Parietal Cells
Signup and view all the flashcards
Chief Cells
Chief Cells
Signup and view all the flashcards
Study Notes
Gastrointestinal Tract Functions
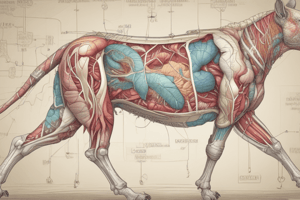
- The gastrointestinal tract (GIT) transfers digested nutrients, minerals, and water from the external environment to the internal environment, involving digestion and absorption.
- Digestion forms absorbable molecules from food through GIT motility, pH changes, and enzymes, which are mainly produced by the pancreas by breaking down food.
- Absorption moves digestive food from the intestine into the blood or the lymphatic system.
- Excretion removes non-absorbable food components, bacteria, intestinal cells, hydrophobic molecules (drugs), cholesterol, and steroids.
- The GIT acts as a host defense by forming a barrier with the outside environment and a developed immune system.
- The GIT can inactivate harmful bacteria and microorganisms in the large intestine.
Gastrointestinal Tract Components
- The GIT includes the mouth, pharynx, esophagus, stomach, small intestine (duodenum, jejunum, ileum), and large intestine.
- Accessory organs include the pancreas, liver and gallbladder.
Structure of the Gastrointestinal Tract
- The GIT is a long muscular tube stretching from the mouth to the anus.
- From the mid-esophagus to the anus, the composition is similar.
- Circular folds are where the entire inner surface of the tube folds in on itself.
- The top third of the human esophagus is made of skeletal muscle.
- The rest of the GIT is composed of smooth muscle.
- The lumen is the inside of the tube, and it contains many folds and processes to increase surface area.
- Villi project into the lumen of the tube and have crypts or invaginations below the surface.
Layers of the Gastrointestinal Tract
- The mucosa contains three subsections: epithelium, lamina propria, and muscularis mucosa.
- Other layers include the submucosa, muscularis externa (outer muscular layer), and serosal layer (connective tissue layer).
Layers of the Mucosa
- The mucosa has three layers: epithelium, lamina propria, and muscularis mucosa.
- Epithelium lines all body cavities and surfaces.
- Epithelial cells have a basolateral surface and an apical surface, meaning they are polarized.
- The apical surface inserts into the inside of the tube or the lumen.
- The basolateral surface faces away from the tube, closest to the blood surface.
- The polarized epithelial layer has different transport proteins at the apical surface compared to the basolateral surface.
- Transport proteins are restricted to different cell surfaces due to tight junctions.
Epithelial Layer
- The epithelial layer consists of a single layer of cells that selectively uptake nutrients, electrolytes, and water while preventing harmful substances from passing through.
- It has an amplified surface area due to villi and crypts.
- Villi contain a single layer of epithelial cells, including microvilli.
- Crypts are regions of invagination into the lamina propria.
- Stem cells in the crypts divide to produce differentiated daughter cells, including absorptive and mucous-producing cells.
- Stem cells migrate up the villus, reaching the top and sloughing off at the end of their life.
- The epithelial cell layer is replaced every 5 days in the small intestine.
- Rapidly dividing epithelial cells are susceptible to anticancer drugs, which can result in diarrhea or bloody stool.
Selective Transport Across the Epithelium
- The epithelial layer is selective, allowing specific nutrients to cross the intestinal epithelium into the body.
- Chemicals or molecules can use two pathways to cross the epithelial layer: paracellular and transcellular.
- Paracellular pathways allow chemicals to move between cells across cell junctions, but are limited by tight junctions, restricting the diffusion of water and small ions; not many substances can pass through this pathway.
- Transcellular pathways cross the cell and require transport proteins; many nutrients must use this two-step process.
Lamina Propria
- The lamina propria includes everything above the muscle layer.
- Its structures include connective tissue, small blood vessels (arterioles and capillaries), nerve fibers, lymphatic vessels, and immune and inflammatory cells for immune protection.
- It contains a lacteal or lymphatic vessel.
Muscularis Mucosa
- It is a thin layer of smooth muscle that is not involved in GIT contraction, but may function in moving the villi.
Submucosa
- The submucosa is beneath the mucosa layer.
- This submucosal layer contains blood vessels, lymphatic vessels, the submucosal nerve plexus, and connective tissue.
- The submucosal nerve plexus relays information to and from the mucosa.
Muscularis Externa
- The muscularis externa includes circular muscle, the myenteric nerve plexus, and longitudinal muscle.
- Circular muscle (thick inner layer) fibers are oriented in a circular pattern and contract and relax to close and open the tube (causing narrowing of the lumen).
- The myenteric nerve plexus (myo = "of muscle") regulates the muscle function of the GIT.
- Longitudinal muscle lengthens and shortens to control the length of the tube, but does not change the diameter.
Serosa
- It is a thin connective tissue layer that encases the intestine and forms connections with the intestine and the abdominal wall.
Blood Supply for Digestive Processes
- The GIT's blood supply carries away many nutrients and other absorbed components from the diet.
- The blood supply transports water-soluble nutrients and other molecules.
- Lacteals (lymphatic system; lamina propria in the mucosa layer) are important for fat absorption.
- Blood enters the GIT highly oxygenated (red) but loses that oxygen as it perfuses the intestine (blue).
- Blood that perfuses the intestine goes to the liver via the portal vein and does not flow directly from the GIT back to the heart.
Process of Digestion
- Food is digested, starting in the stomach.
- Absorption and secretion occur in the small intestine.
- Processing occurs in the colon.
- The elimination of feces containing indigestible material happens next.
Portal Circulation
- Portal circulation is a circulation that drains blood from the digestive tract to the liver.
- Blood in the portal circulation is nutrient-rich.
- It’s important for the liver removes harmful substances and processes nutrients with its enzymes, detoxification.
- The liver is an exception to the rule that most organs in the body are perfused by arterial blood because the source is fully oxygenated.
- When you have not been eating, about 30% of the blood in the liver comes from an arterial source.
- After eating, this is reduced to 10%.
- The hepatic artery contains fully oxygenated blood that perfuses the liver and the hepatic portal vein carries blood to the liver that has already perfused the stomach, pancreas, small intestine, and large intestine.
- These two blood supplies mix, so that the liver is perfused with nutrient-rich blood coming from the GIT organs with a poor oxygen content.
Series vs Parallel Circulation
- Most organs are perfused in parallel within the systemic circulation.
- The liver is perfused in series because the liver is perfused predominantly by blood that has already perfused another organ; blood flows from the digestive organs to the liver
- Some blood comes from the heart, but most comes from digestive organs (stomach, pancreas, intestines) and it flows in series between them
Regulation of GI Processes
- GI processes are primarily controlled through the volume and composition of what is inside the intestinal tract rather than by the CNS.
- GI processes include secretion and motility, or the movement of the GI tract.
Reflexes Regulating GI Processes
- Reflexes which regulates Gl processes are initiated by Distension of the GIT wall by the volume, Osmolarity of whats contained (pH).
- The concentration of the specific digestion contents, such as monosaccharides,fatty acids, peptides and amino acids initiates different regulatory pathways
- These reflexes are propagated by various receptors
- Distension of the wall, osmolarity, pH and specific contents trigger the initiate reflexes by acting through various receptors in the wall.
- Mechanoreceptors are activated by mechanical stimuli (pressure and stretch); eating a lot and stretching out the stomach.
- Osmoreceptors are activated by a change in osmolarity such as eating salty food.
- Chemoreceptors are activated by specific chemicals.
Intrinsic Neural Regulation of GI
- Processes are performed to control motility and secretion.
- Intrinsic is neural regulation contained wholly within the organ, occurs with nerve plexi located in the GIT wall.
- Nerve plexi branching networks of intersecting nerves ( Enteric nervous system, intrinsic nerve regulation) controls the activity of the secretomotor, neurons which has a role in secretion and motility.
- A large number of neurons"Brain of the gut" in the walls of the contained Enteric nervous system
- Involuntary digestive functions are critical as the system functions independently of the CNS allowing us to digest our food without having to think about it.
Myenteric Plexus
- Network of nerves located between the circular and longitudinal muscle layers of the muscularis externa.
- Responsible for influencing and regulating the smooth muscle.
Submucosal Plexus
- Network of nerves located predominatley in the submucosa.
- Predominantly influences secretion.
- Has Nerves that extend from the submucosal, plexus to the mucosa to control secretion
Plexi Interactions in the Digestive System
- The neural activity in one plexus influences the activity in the other.
- The Communication between the two layers occurs so that motility and secretion of digestive enzymes work together , assisting mobile activity.
- An Extrinsic process is outside of the gut wall and extrensic regulation occurs through autonomi nervous system ANS.
- Nerve fibers from the parasympathetic and sympathetic pathways enter the intestinal tract and synapse with neurons in both plexuses.
- The CNS can influence motility and secretion through the autonomic nervous system as its used of food sends signals through the brain to the GIT start to g.ets eady.
- Emotional states create Different emotional states in the brain, influence appetite.
Autonomic Pathways in the GI System
- The "Rest and digest" Parasympathetic response stimulates the flow of a large volume of watery saliva, Stimulates peristalsis
- “Fright, flight, fight" Sympathetic response Stimulates the small, Volume small, thick saliva inhibits peristalsis Inhibits Secretion.
- Reflexes which use a Long long neural extisic neural or short or short intrinsic pathways.
Gastroenteric Stimuli
- Are short reflexes that are intrinsic pathway modify modify and secretion , stimulus activated by aReceptors , nerves and action
- These stimuli includes eating a meal activates, Receptors in GIT wall ( mechanoreceptors, or somo receptores chemoreceptors_ stimulus froim receptors for into nervous tostimuales and muscle, to causes response. Or SMELL food hungry/emotion to stimulus and the CNS, then action of the stomach,
Chemical Messenger Regulation
- Has chemical messenger regulation and, includes a 4 categories, Hormone-secreting cells release into through bas lateral into one or many parts of the body, which releases must action.
- A Neurocrne regulation, nerve cell prounce electrical signals release the neurontransmitter, which travels action cell both neuton and the ccells, messeger reeache the acts synapse, act on Synpatic cell.
- Paracrine the region to acts on the body and or autocrine.
HOrmond control
- The endcorine is a form stimulous and it, is a production with eputhlium
- Interoendochrine is a form function where hormones
- Hrmpnal is forrm glucogen.
Hormonal Control of GI Activity
- These are all peptide hormones released by endocrine cells that Participate to perform with regualtion, for a some aspect with Gi rumen.
CCK Feedback
- For in example in cck , realse stimulate the presence and releashes the panceas.
- Absoption of acts controls the releasses or control.
Intestinal Motility
- Stim by contraction and relax, outer action the GIT, causes the contant action.
- Peristasis maintcevesd.
- and Circular muscles the area.
- Important for mixing foods, segments with lottle of net work,, mostly, allow mixed and Slow
Basic Electrical Rhythm
- Occurs with, Cell that distributed through, and constantly Constantly the basic rhythm, the cells all actions When a absence or hermon and neurals, do not actions, If any the -slows for, fluctations action,the
Phases of Gastrointestinal Control
- The neurial conrol is what it percieved and to do.
- Cephatic head with smell or site with eomtional
- The repsoncive fiber activated, GASTICE, receptors adic.
- These stimu by mediatations. Intestainal then secreted enodcroie
Control INTake Fod
Imoiratn is an in the coofidatin, and feeding cernern.
Orexin
- Is an orexincreae, and nurotepiide and release when to start cell.
- Anoexic, is and release to reduce
- Reatred to depst to the leptin the hormone for hte cals
Reguatlion of WAyer IN tkae
- Are combiien, where contain thirst by the increase, and the decrease, vOlumE.
SLiARY glanf
- has and main pairs and is a the side ceek.
- Paortod, is watery
- aducl procuvce, to 1500 mm.
Compistiton of SAvi
- HA, is the hypoi.
- Watter, electrtis and antibitic.
Prcuion
, mosutit.
Anatomu with glan
- Struacure with saliavry the structure
Prcuiion
Myophitiall cels to ush h te saliva, to region.
Fomatin
- cels acins tight junctions between cells alllow for, a leakae then dcutal dont
- Primar secretion the ot yet is iso, contatin, encymes then is , cel contravt to pushes.
Regaon
- HA no for the prodcuion.
Sympahtiec
- stimatit but in reavse, and prottein increeasde.
Salvi dgest
- IN d gestuion, amalay, with an zymes,. And it reatct to Plan stac h the gluces.
Role of SAva
- STa, and amayel, in the the
Swlaliing
- IS A the complex to air, and a is stimulatws.
Eaphogus
- As is the the msucle, and a is rapidly absorb
Upper
It is, and lwoer,
Eatat
- And a not good
Phase to swlalngn
- Realx to sphiter, moves the to the, stamch. For gravitay.
Hwat
- Are is to reeave
The STamch
- The oragn. The msucle for th ebsween and the intersntie to the
- Functionn,, to brreka down and the dgs.
Function
- Compoensts to physacally breatk into the the
Sectors
- Exocorine to chemcal, into is to not in the cells. Major, procuion, and helps the digestiton Hicl to hydros and it also attemt to kill,.
Types With the Cel
Generzlized gastic is becasue
Cel Fuctions
Chief cel or all the stcmah.. Hici acii. The mico The
- Pepesin accesslratee the digesstion where cel. A the hrmoe
Parietal cells
- Are called and an facatr an
- An to
- And michtocnd.
Regulatin if the Acsid.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Explore the role of lingual lipase in neonates, radiation-induced xerostomia, and the mechanics of swallowing. Understand the liver's dual blood supply, its importance in nutrient processing, and the unique features of the esophagus. Also, learn the importance of amylase and lingual lipase during some diseases.