Podcast
Questions and Answers
What is the optimal angle to maintain between the spreader and the slide during blood smear preparation?
What is the optimal angle to maintain between the spreader and the slide during blood smear preparation?
- The angle is not important
- 30 degrees
- 90 degrees
- 45 degrees (correct)
Which characteristic does NOT describe a well-stained peripheral blood film?
Which characteristic does NOT describe a well-stained peripheral blood film?
- The thin portion has a 'rainbow' appearance
- The film appears bullet-shaped (correct)
- The lateral edges of the film are visible
- The film is smooth without irregularities
What is a significant advantage of using coverslips over slides in blood smear preparation?
What is a significant advantage of using coverslips over slides in blood smear preparation?
- Coverslips are easier to handle
- Coverslips produce larger sample areas
- Coverslips allow for faster drying
- Leucocytes are more evenly distributed in coverslip smears (correct)
Which drying method is NOT recommended for blood smears?
Which drying method is NOT recommended for blood smears?
What size should the blood drop be for an ideal blood smear?
What size should the blood drop be for an ideal blood smear?
What does a differential count primarily assess?
What does a differential count primarily assess?
Which white blood cell type is NOT classified among the five basic types in a differential count?
Which white blood cell type is NOT classified among the five basic types in a differential count?
What information does the absolute value in a differential count provide?
What information does the absolute value in a differential count provide?
What is one of the uses of a differential count?
What is one of the uses of a differential count?
Which of the following best describes the process of a manual differential count?
Which of the following best describes the process of a manual differential count?
What does an increase in eosinophils indicate?
What does an increase in eosinophils indicate?
Which of the following cells serves as the primary defense against infections?
Which of the following cells serves as the primary defense against infections?
What does 'shift to the left' refer to in a white blood cell response?
What does 'shift to the left' refer to in a white blood cell response?
What might cause eosinopenia?
What might cause eosinopenia?
What is the correct order of steps in performing a differential count?
What is the correct order of steps in performing a differential count?
Which of these conditions is associated with lymphocytosis?
Which of these conditions is associated with lymphocytosis?
What is a common disorder causing monocytosis?
What is a common disorder causing monocytosis?
Which type of blood smear is prepared using the two-glass slide method?
Which type of blood smear is prepared using the two-glass slide method?
Flashcards
Differential Count
Differential Count
A blood test that determines the relative number of each type of white blood cell (WBC) present in a blood sample.
Neutrophils
Neutrophils
A specific type of WBC that fights bacterial infections by engulfing and destroying them.
White Blood Cell Count (WBC Count)
White Blood Cell Count (WBC Count)
A blood test that measures the total number of WBCs per microliter of blood.
Complete Blood Count (CBC)
Complete Blood Count (CBC)
Signup and view all the flashcards
Relative Differential Count
Relative Differential Count
Signup and view all the flashcards
Blood Smear Preparation
Blood Smear Preparation
Signup and view all the flashcards
Factors Influencing Blood Smear Thickness
Factors Influencing Blood Smear Thickness
Signup and view all the flashcards
Ideal Features of a Blood Smear
Ideal Features of a Blood Smear
Signup and view all the flashcards
Coverslip vs Slide Smear: Pros and Cons (Part 1)
Coverslip vs Slide Smear: Pros and Cons (Part 1)
Signup and view all the flashcards
Coverslip vs Slide Smear: Pros and Cons (Part 2)
Coverslip vs Slide Smear: Pros and Cons (Part 2)
Signup and view all the flashcards
Stab Cells (Band Cells)
Stab Cells (Band Cells)
Signup and view all the flashcards
Eosinophils
Eosinophils
Signup and view all the flashcards
Eosinophilia
Eosinophilia
Signup and view all the flashcards
Eosinopenia
Eosinopenia
Signup and view all the flashcards
Lymphocytes
Lymphocytes
Signup and view all the flashcards
Lymphocytosis
Lymphocytosis
Signup and view all the flashcards
Study Notes
Differential Count and Blood Smear Preparation
- A differential count, also known as a leukocyte differential count, peripheral differential, white blood cell morphology, or WBC differential, is formally known as a White Blood Cell Count Differential.
- It's typically part of a complete blood count (CBC).
- It determines the relative number of each type of white blood cell (WBC) in peripheral blood.
- Results are expressed as percentages (relative numbers of each WBC type in relation to the total WBC) and absolute values (percentage × total WBC).
Uses of Differential Count
- Assesses the body's ability to respond to and eliminate infections.
- Detects the severity of allergic and drug reactions.
- Detects the response to parasitic and other types of infections.
- Crucial for evaluating the reaction to viral infections.
- Evaluates response to chemotherapy.
- Identifies various stages of leukemia.
Manual Differential Count
- Approximates WBC count based on cell count/high-power field (hpf).
- WBC counts (per cubic millimeter) are estimated roughly as follows:
- 2-4 cells/hpf = 4,000 – 7,000 WBC/mm³
- 4-6 cells/hpf = 7,000 – 10,000 WBC/mm³
- 7-10 cells/hpf = 10,000 – 13,000 WBC/mm³
- 10-20 cells/hpf = 13,000 – 18,000 WBC/mm³
White Blood Cell Types
- Five basic WBC types: Neutrophils, Lymphocytes, Monocytes, Eosinophils, and Basophils.
Neutrophils
- Also known as Segmented Polymorphonuclear Leukocytes (PMNs), Neutrophils, or Segs.
- The most common WBC type, functioning as the primary defense against infection.
- Neutrophilia: Increased neutrophil count, typically a response to infection or severe injury (e.g., bacterial infection, appendicitis, chronic myelogenous leukemia).
- "Shift to the left": Increased band/stab cells in a blood smear, an early sign of a WBC response to an infection, even before the overall WBC count increases.
Eosinophils
- Play a role in allergic disorders and combating parasitic infections.
- Eosinophilia: Increased eosinophil count, often in response to allergic disorders, skin inflammation (e.g., scarlet fever), or parasitic infections; also seen in some bone marrow disorders such as eosinophilic leukemia.
- Eosinopenia: Decreased eosinophil count, often due to stress or steroid exposure.
Lymphocytes
- Play a role in both immediate and delayed responses to infections or inflammation.
- Lymphocytosis: Increased lymphocyte count, commonly seen in viral infections, infectious mononucleosis, lymphocytic leukemia, bone marrow cancers, or radiation therapy.
Monocytes
- Respond to inflammation, infection, and foreign bodies by ingesting and digesting foreign material.
- Monocytosis: Increased monocyte count, often seen in various kinds of infection and inflammatory disorders, including brucellosis and tuberculosis. Also associated with various cancers, including monocytic leukemia.
- Other conditions associated with monocytosis: subacute bacterial endocarditis, typhoid fever, rickettsial infections, collagen diseases, Hodgkin’s disease, Gaucher's disease.
Basophils
- Basophilia: Increased basophil count, often seen in chronic inflammation, hypersensitivity reactions (e.g., food allergies), or leukemia.
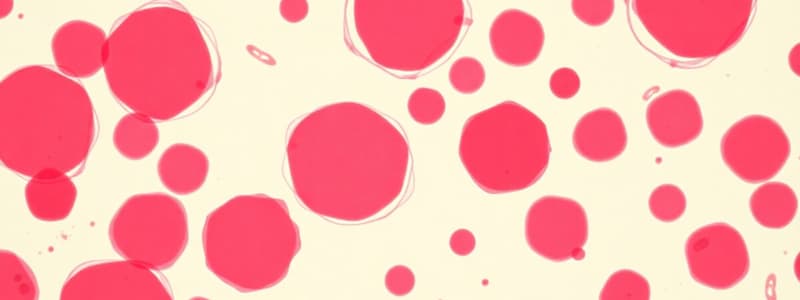
Blood Smear Preparation
- Steps: Prepare blood smear, stain the smear, count the cells, and report results.
- Smear Types: Cover glass smear, wedge smear, spun smear, buffy coat smear, thick blood smear.
- Smear Preparation Methods: 2-Coverslip method (Ehrlich's method), Two-glass slide method (Wedge method), Glass slide - Coverslip method (Beacom's method), Spinner's method.
- Prerequisites: Clean slides & coverslips, appropriate blood drop size, quick smearing to prevent clotting, proper spreader angle & pressure.
- Factors Affecting Smear Thickness: Drop size, angle between slide & spreader, spreader speed, spreader pressure.
- Well-Stained Smear Features: Film length (2/3 to 3¼ slide length), finger-shape (feather edge), smooth edges, & "rainbow" appearance at thin edge when held to light. Whole blood drop picked up & spread.
- Coverslip vs Slide: "Perfect" coverslip smears are better for even distribution of leukocytes; however "perfect" slide smears easier to learn & average quality slide smears are better than those of average coverslips.
- Methods in Drying Blood Smear: Air drying, low flame (e.g., bunsen burner), using oven, methyl alcohol or absolute alcohol immersion (1-2 minutes).
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.