Podcast
Questions and Answers
What effect does the destruction of elastic fibers in the alveoli have on lung function?
What effect does the destruction of elastic fibers in the alveoli have on lung function?
- It enhances the ability to exhale air.
- It improves blood flow to the alveoli.
- It leads to a loss of recoil and air trapping during exhalation. (correct)
- It increases the elasticity of the lung tissue.
How does air trapping affect respiratory effort?
How does air trapping affect respiratory effort?
- It has no significant impact on respiratory effort.
- It decreases the work of breathing.
- It prevents any effort to exhale.
- It leads to hyperinflation and increased work of breathing. (correct)
What is the result of a ventilation/perfusion mismatch in COPD patients?
What is the result of a ventilation/perfusion mismatch in COPD patients?
- Enhanced efficiency of gas exchange.
- No impact on blood flow.
- Hypoxia and hypercapnia. (correct)
- Increased oxygenation of the blood.
Which is a major risk factor for the development of COPD?
Which is a major risk factor for the development of COPD?
What percentage of COPD exacerbations are triggered by respiratory infections?
What percentage of COPD exacerbations are triggered by respiratory infections?
Which of the following is NOT considered a non-modifiable risk factor for COPD?
Which of the following is NOT considered a non-modifiable risk factor for COPD?
What condition is indicated by prolonged hypoxia in COPD patients?
What condition is indicated by prolonged hypoxia in COPD patients?
What is the primary cause of COPD in high-income countries?
What is the primary cause of COPD in high-income countries?
What is the primary cause of Chronic Obstructive Pulmonary Disease (COPD) in high-income countries?
What is the primary cause of Chronic Obstructive Pulmonary Disease (COPD) in high-income countries?
Which of the following is not a characteristic of chronic bronchitis in COPD?
Which of the following is not a characteristic of chronic bronchitis in COPD?
What role do cytokines like IL-1β and TNF-α play in chronic bronchitis?
What role do cytokines like IL-1β and TNF-α play in chronic bronchitis?
Which subtype of COPD is characterized by impaired ciliary function and mucus accumulation?
Which subtype of COPD is characterized by impaired ciliary function and mucus accumulation?
What is the effect of smooth muscle hypertrophy in chronic bronchitis?
What is the effect of smooth muscle hypertrophy in chronic bronchitis?
Which factor is associated with the genetic susceptibility to COPD, particularly in non-smokers?
Which factor is associated with the genetic susceptibility to COPD, particularly in non-smokers?
Chronic exposure to what substance primarily triggers the proteolytic destruction of alveolar walls in emphysema?
Chronic exposure to what substance primarily triggers the proteolytic destruction of alveolar walls in emphysema?
What happens to the size and number of goblet cells as a result of chronic inflammation in COPD?
What happens to the size and number of goblet cells as a result of chronic inflammation in COPD?
Flashcards
Chronic Obstructive Pulmonary Disease (COPD)
Chronic Obstructive Pulmonary Disease (COPD)
A condition affecting the lungs, characterized by persistent airflow obstruction and inflammation, resulting in difficulty breathing.
Loss of Elastic Recoil
Loss of Elastic Recoil
The breakdown of elastic fibers in the alveoli, leading to reduced lung recoil and air trapping during exhalation.
Air Trapping
Air Trapping
Inability to exhale fully due to air trapping in the lungs, causing overinflation and increased breathing effort.
Ventilation/Perfusion Mismatch
Ventilation/Perfusion Mismatch
Signup and view all the flashcards
Pulmonary Hypertension
Pulmonary Hypertension
Signup and view all the flashcards
Smoking
Smoking
Signup and view all the flashcards
Occupational Exposure
Occupational Exposure
Signup and view all the flashcards
Repeated Respiratory Infections
Repeated Respiratory Infections
Signup and view all the flashcards
What is COPD?
What is COPD?
Signup and view all the flashcards
What is Chronic Bronchitis?
What is Chronic Bronchitis?
Signup and view all the flashcards
What is Emphysema?
What is Emphysema?
Signup and view all the flashcards
What are the most common causes of COPD?
What are the most common causes of COPD?
Signup and view all the flashcards
Explain the pathophysiology of Chronic Bronchitis.
Explain the pathophysiology of Chronic Bronchitis.
Signup and view all the flashcards
Explain the pathophysiology of Emphysema.
Explain the pathophysiology of Emphysema.
Signup and view all the flashcards
How does COPD affect breathing?
How does COPD affect breathing?
Signup and view all the flashcards
What role does genetics play in COPD?
What role does genetics play in COPD?
Signup and view all the flashcards
Study Notes
Chronic Obstructive Pulmonary Disease (COPD)
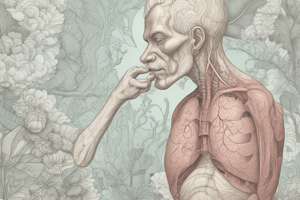
- COPD is a chronic, progressive respiratory disease characterized by persistent airflow limitation, not fully reversible
- Two overlapping phenotypes: Chronic bronchitis and Emphysema
- Chronic bronchitis: Chronic inflammation of the bronchi, excessive mucus production
- Emphysema: Destruction of alveolar walls, leading to loss of elastic recoil and air trapping
- Tobacco smoking is the primary cause of COPD, accounting for 70% of cases in high-income countries
- Exposure to environmental pollutants (indoor and outdoor air pollution) contributes to COPD development
- Occupational exposure (dust, vapors, irritants) can damage lungs and promote COPD
- Genetic mutations, such as a1-antitrypsin deficiency, increase COPD susceptibility, especially in non-smokers. The a1-antitrypsin protein normally protects lung tissue from damage.
- Pathophysiology generally involves chronic inflammation, airway remodeling, increased work of breathing, and abnormalities in mucus production.
- Airway hyperresponsiveness, inflammation, mucus hypersecretion, and airway narrowing contribute to the pathophysiology
- Chronic bronchitis: Inhaled irritants (e.g., cigarette smoke) promote chronic inflammation predominantly involving Th1 cells, macrophages, and neutrophils
- Increased mucus production due to cytokines like IL-1β and TNF-α, increasing goblet cell and mucous gland size and number.
- Impaired cilia function leads to mucus accumulation
- Chronic inflammation promotes smooth muscle hypertrophy, airway narrowing, and metaplasia of epithelial cells into squamous cells
- Alveolar destruction is caused by proteolytic enzymes, released by neutrophils and macrophages, destroying alveolar walls.
- Loss of elastic recoil, causing air trapping during exhalation, is a result of elastic fiber destruction in the alveoli
COPD Pathophysiology
- Chronic inflammation leads to airway remodeling, mucus hypersecretion, and airway narrowing.
- Chronic bronchitis, marked by mucus hypersecretion and airway abnormalities
- Emphysema, characterized by alveolar destruction and loss of elastic recoil.
- Air trapping: Inhaling air in the alveoli and not being able to exhale it completely results in hyperinflation and increased work of breathing, impacting the lungs' ability to fill completely with air in the lungs.
- Ventilation/Perfusion mismatch: Damaged alveoli cause imbalances in ventilation and blood flow.
- Pulmonary hypertension: Prolonged hypoxia, or low blood oxygen, can lead to vascular remodeling, promoting pulmonary hypertension and eventual right-sided heart failure (cor pulmonale).
COPD Risk Factors
- Modifiable risk factors: Smoking is the most significant cause (70% high-income countries), indoor/outdoor air pollution, occupational exposure (dust, chemicals, fumes), repeated respiratory infections
- Non-modifiable risk factors: Age (risk increases with age), gender (more common in men, but increasing in women), genetic predisposition (a1-antitrypsin deficiency), ethnicity
- There are genetic susceptibilities and socioeconomic factors that can also increase COPD risk.
COPD Transmission
- COPD is not transmissible (not an infectious disease); however, respiratory illnesses can trigger COPD exacerbations (acute events).
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.