Podcast
Questions and Answers
What are the primary conditions encompassed by Chronic Obstructive Pulmonary Disease (COPD)?
What are the primary conditions encompassed by Chronic Obstructive Pulmonary Disease (COPD)?
- Bronchial hyperreactivity and asthma
- Asthma and chronic bronchitis
- Pulmonary fibrosis and emphysema
- Emphysema and chronic bronchitis (correct)
What is the significance of a FEV1/FVC ratio of less than 70% in pulmonary function tests?
What is the significance of a FEV1/FVC ratio of less than 70% in pulmonary function tests?
- Indicates excellent respiratory capacity
- Indicates normal lung function
- Confirms airflow limitation (correct)
- Suggests restrictive lung disease
Which of the following factors is a common cause of Chronic Obstructive Pulmonary Disease (COPD)?
Which of the following factors is a common cause of Chronic Obstructive Pulmonary Disease (COPD)?
- Environmental exposure to irritants (correct)
- Regular physical exercise
- Excessive exposure to sunlight
- High-altitude living
How does chronic inflammation contribute to the pathophysiology of COPD?
How does chronic inflammation contribute to the pathophysiology of COPD?
What does the 6-Minute Walk Test primarily evaluate in COPD patients?
What does the 6-Minute Walk Test primarily evaluate in COPD patients?
Which of the following tests would be least useful for identifying structural lung changes due to emphysema?
Which of the following tests would be least useful for identifying structural lung changes due to emphysema?
What is a characteristic symptom of airflow limitation in COPD?
What is a characteristic symptom of airflow limitation in COPD?
What role do cytokines play in the pathophysiology of COPD?
What role do cytokines play in the pathophysiology of COPD?
Flashcards
COPD
COPD
A progressive, chronic lung disease with airflow obstruction that doesn't fully reverse. It includes emphysema and chronic bronchitis.
Emphysema
Emphysema
Damage to the tiny air sacs (alveoli) in the lungs, causing them to lose their elasticity and ability to exchange gases efficiently.
Chronic Bronchitis
Chronic Bronchitis
Inflammation of the airways leading to increased mucus production and narrowing of the airways.
Airflow Limitation in COPD
Airflow Limitation in COPD
Signup and view all the flashcards
Air Trapping in COPD
Air Trapping in COPD
Signup and view all the flashcards
FEV1/FVC Ratio
FEV1/FVC Ratio
Signup and view all the flashcards
Hypoxemia in COPD
Hypoxemia in COPD
Signup and view all the flashcards
Hypercapnia in COPD
Hypercapnia in COPD
Signup and view all the flashcards
Study Notes
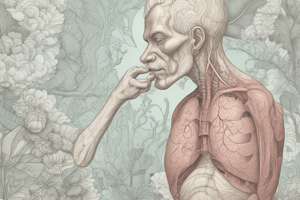
Chronic Obstructive Pulmonary Disease (COPD)
- COPD is a progressive, chronic inflammatory lung disease.
- Airflow obstruction is a key characteristic of COPD, and it's not fully reversible.
- COPD includes two main conditions: emphysema (damaging alveoli) and chronic bronchitis (inflammation/mucus in airways).
- Smoking is a primary cause of COPD.
- Environmental irritants and genetic factors, like alpha-1-antitrypsin deficiency, also contribute to COPD.
Pathophysiology of COPD
-
Chronic Inflammation: Exposure to noxious particles (e.g., cigarette smoke) causes inflammation in airways, lung parenchyma, and pulmonary vasculature.
-
Inflammatory cells (e.g., macrophages, neutrophils) release cytokines, perpetuating tissue damage.
-
Airflow Limitation: Small airway narrowing results from mucus hypersecretion and fibrosis.
-
Loss of elastic recoil in the lungs (due to alveolar destruction—emphysema) worsens airflow limitation.
-
Air Trapping and Hyperinflation: When small airways collapse during exhalation, air gets trapped, leading to hyperinflation and increased breathing effort.
-
Gas Exchange Abnormalities: Impaired alveoli reduce oxygen intake and carbon dioxide elimination. This leads to hypoxemia (low blood oxygen) and hypercapnia (high blood carbon dioxide).
Diagnostic Tests and Evaluations
- Pulmonary Function Tests (PFTs): Forced Expiratory Volume in 1 second (FEV1) measures the volume of air exhaled in one second. A FEV1/FVC ratio below 70% confirms airflow limitation (indicating COPD severity).
- Arterial Blood Gases (ABG): Measures oxygen (PaO2), carbon dioxide (PaCO2), and pH levels to evaluate gas exchange and identify abnormalities like hypoxemia and respiratory acidosis.
- Chest X-ray: Shows hyperinflation, a flattened diaphragm, or bullae (air-filled sacs). It identifies structural changes in the lungs caused by emphysema.
Additional Diagnostic Considerations
- Alpha-1 Antitrypsin Levels: Screening younger patients without a smoking history to assess for genetic deficiency. This helps determine genetic predisposition to COPD.
- 6-Minute Walk Test: Measures exercise tolerance and oxygen desaturation during physical activity. This evaluates functional capacity and the need for supplemental oxygen.
Medications for COPD
- Bronchodilators: These medications are used to relax smooth muscles in the airways and improve airflow.
- Drug Classifications:
- Beta-2 agonists (e.g., salbutamol, salmeterol)
- Anticholinergics (e.g., tiotropium, ipratropium)
- Methylxanthines (e.g., theophylline)
- Mechanism of Action:
- Beta-2 agonists: Relax smooth muscle in airways by stimulating beta-2 receptors.
- Anticholinergics: Block muscarinic receptors, reducing bronchoconstriction and mucus secretion.
- Methylxanthines: Relax airway muscles and improve diaphragmatic contractility.
- Drug Classifications:
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.