Podcast
Questions and Answers
Which of the following best describes the primary storage location of calcium in the body?
Which of the following best describes the primary storage location of calcium in the body?
- Extracellular fluid
- Muscle tissue
- Blood plasma
- Bones and teeth (correct)
Which of the following is a critical function of calcium in the human body?
Which of the following is a critical function of calcium in the human body?
- Synthesis of red blood cells
- Regulation of body temperature
- Detoxification of harmful substances
- Bone structure and muscle contraction (correct)
What is the main function of osteoclasts in bone remodeling?
What is the main function of osteoclasts in bone remodeling?
- Dissolving bone tissue (correct)
- Stimulating bone growth
- Secreting the bone matrix
- Signaling bone density
Which of the following molecules directly inhibits osteoclastogenesis?
Which of the following molecules directly inhibits osteoclastogenesis?
What is the primary organic component synthesized by osteoblasts to form bone?
What is the primary organic component synthesized by osteoblasts to form bone?
Which process do osteoclasts utilize to dissolve bone minerals during resorption?
Which process do osteoclasts utilize to dissolve bone minerals during resorption?
Which of the following cell types is considered a mechanosensor in bone, responding to strain and regulating bone remodeling?
Which of the following cell types is considered a mechanosensor in bone, responding to strain and regulating bone remodeling?
Which component contributes most to the flexibility of bone?
Which component contributes most to the flexibility of bone?
Which of the following accurately describes the effect of removing the organic component of bone?
Which of the following accurately describes the effect of removing the organic component of bone?
Which of the following proteins, secreted by osteoblasts, binds to hydroxyapatite and calcium, initiating mineralization and strengthening bone?
Which of the following proteins, secreted by osteoblasts, binds to hydroxyapatite and calcium, initiating mineralization and strengthening bone?
How does calcitriol primarily contribute to calcium homeostasis?
How does calcitriol primarily contribute to calcium homeostasis?
What is the primary stimulus for parathyroid hormone (PTH) secretion?
What is the primary stimulus for parathyroid hormone (PTH) secretion?
What is the primary action of calcitonin in regulating serum calcium levels?
What is the primary action of calcitonin in regulating serum calcium levels?
Which of the following is the most likely consequence of hypercalcemia?
Which of the following is the most likely consequence of hypercalcemia?
Which condition is most likely associated with vitamin D deficiency?
Which condition is most likely associated with vitamin D deficiency?
What condition is characterized by excessively brittle bones due to a genetic defect in collagen production?
What condition is characterized by excessively brittle bones due to a genetic defect in collagen production?
In cases of hypoparathyroidism, what is a common treatment strategy?
In cases of hypoparathyroidism, what is a common treatment strategy?
Which of the following is a potential cause of secondary hyperparathyroidism?
Which of the following is a potential cause of secondary hyperparathyroidism?
Which of the following characteristics is associated with osteoarthritis?
Which of the following characteristics is associated with osteoarthritis?
Which factor primarily leads to brittle and fragile bones in osteoporosis?
Which factor primarily leads to brittle and fragile bones in osteoporosis?
What is the underlying mechanism of multiple myeloma that leads to increased bone fractures?
What is the underlying mechanism of multiple myeloma that leads to increased bone fractures?
What is the primary function of VDJ recombination?
What is the primary function of VDJ recombination?
What process is directly responsible for increasing the affinity of antibodies to a specific antigen?
What process is directly responsible for increasing the affinity of antibodies to a specific antigen?
Where does somatic hypermutation primarily occur?
Where does somatic hypermutation primarily occur?
In the context of B-cell development, what is the role of clonal selection?
In the context of B-cell development, what is the role of clonal selection?
What is the role of interleukin-6 (IL-6) in the development of multiple myeloma?
What is the role of interleukin-6 (IL-6) in the development of multiple myeloma?
Which of the following conditions is directly linked to an increased risk of infection in multiple myeloma?
Which of the following conditions is directly linked to an increased risk of infection in multiple myeloma?
Which of the following is an indicator of kidney problems in multiple myeloma?
Which of the following is an indicator of kidney problems in multiple myeloma?
What is the significance of Bence-Jones proteins in the diagnosis of multiple myeloma?
What is the significance of Bence-Jones proteins in the diagnosis of multiple myeloma?
What is a frequent symptom of hypercalcemia linked to osteoclast activation in multiple myeloma?
What is a frequent symptom of hypercalcemia linked to osteoclast activation in multiple myeloma?
What is the primary characteristic of chronic myeloid leukemia (CML)?
What is the primary characteristic of chronic myeloid leukemia (CML)?
What genetic abnormality is associated with chronic myeloid leukemia (CML)?
What genetic abnormality is associated with chronic myeloid leukemia (CML)?
What is the result of the BCR-ABL protein in CML?
What is the result of the BCR-ABL protein in CML?
In CML, what is the usual finding for granulocytes?
In CML, what is the usual finding for granulocytes?
What is the action of calcium blocking sodium channels?
What is the action of calcium blocking sodium channels?
Which of the following is the primary function of osteocytes within bone tissue?
Which of the following is the primary function of osteocytes within bone tissue?
What is the primary source of the organic component of bone matrix?
What is the primary source of the organic component of bone matrix?
How do osteoclasts contribute to maintaining calcium homeostasis in the body?
How do osteoclasts contribute to maintaining calcium homeostasis in the body?
What is the primary composition of the inorganic component of bone that provides its hardness?
What is the primary composition of the inorganic component of bone that provides its hardness?
Which of the following best describes the mechanism by which calcitriol influences bone?
Which of the following best describes the mechanism by which calcitriol influences bone?
Under what physiological condition would parathyroid hormone (PTH) secretion be expected to increase?
Under what physiological condition would parathyroid hormone (PTH) secretion be expected to increase?
How does calcitonin primarily reduce serum calcium levels?
How does calcitonin primarily reduce serum calcium levels?
Which of the following is a consequence of prolonged hypercalcemia?
Which of the following is a consequence of prolonged hypercalcemia?
Which of the following is a common cause of Vitamin D deficiency?
Which of the following is a common cause of Vitamin D deficiency?
What distinguishes osteogenesis imperfecta from other bone disorders like osteoporosis?
What distinguishes osteogenesis imperfecta from other bone disorders like osteoporosis?
What is a typical treatment approach for hypoparathyroidism, focusing on restoring calcium balance?
What is a typical treatment approach for hypoparathyroidism, focusing on restoring calcium balance?
In chronic kidney disease, why does secondary hyperparathyroidism often develop?
In chronic kidney disease, why does secondary hyperparathyroidism often develop?
Which of the following is a typical characteristic of osteoarthritis?
Which of the following is a typical characteristic of osteoarthritis?
Which of the following best describes the mechanism leading to osteoporosis?
Which of the following best describes the mechanism leading to osteoporosis?
Flashcards
Where is calcium stored?
Where is calcium stored?
99% is stored in bones and teeth, and 1% in blood.
What is calcium needed for?
What is calcium needed for?
Needed for bone structure, neuronal communication, muscle contraction, blood clotting and cellular functions.
What do osteoblasts do?
What do osteoblasts do?
They deposit minerals, building bone.
What do osteoclasts do?
What do osteoclasts do?
Signup and view all the flashcards
Osteoprogenitor cells
Osteoprogenitor cells
Signup and view all the flashcards
Osteoblasts
Osteoblasts
Signup and view all the flashcards
Osteocytes
Osteocytes
Signup and view all the flashcards
Osteoclasts
Osteoclasts
Signup and view all the flashcards
Bone matrix composition
Bone matrix composition
Signup and view all the flashcards
Organic matter (osteoid)
Organic matter (osteoid)
Signup and view all the flashcards
Inorganic matter of bone
Inorganic matter of bone
Signup and view all the flashcards
Role of certain proteins in bone
Role of certain proteins in bone
Signup and view all the flashcards
Rickets
Rickets
Signup and view all the flashcards
Osteogenesis imperfecta
Osteogenesis imperfecta
Signup and view all the flashcards
Calcium homeostasis regulators
Calcium homeostasis regulators
Signup and view all the flashcards
Parathyroid hormone (PTH)
Parathyroid hormone (PTH)
Signup and view all the flashcards
Calcitonin
Calcitonin
Signup and view all the flashcards
Hypercalcemia effects
Hypercalcemia effects
Signup and view all the flashcards
Hypocalcemia effects
Hypocalcemia effects
Signup and view all the flashcards
Hypocalcemia treatment
Hypocalcemia treatment
Signup and view all the flashcards
Hypoparathyroidism causes
Hypoparathyroidism causes
Signup and view all the flashcards
Hyperparathyroidism causes
Hyperparathyroidism causes
Signup and view all the flashcards
Osteoarthritis
Osteoarthritis
Signup and view all the flashcards
Osteoporosis
Osteoporosis
Signup and view all the flashcards
Rheumatoid arthritis
Rheumatoid arthritis
Signup and view all the flashcards
Multiple myeloma
Multiple myeloma
Signup and view all the flashcards
Kidney problems in myeloma
Kidney problems in myeloma
Signup and view all the flashcards
Dendritic cells role in myeloma
Dendritic cells role in myeloma
Signup and view all the flashcards
VDJ recombination
VDJ recombination
Signup and view all the flashcards
Hypercalcemia
Hypercalcemia
Signup and view all the flashcards
Hypocalcemia
Hypocalcemia
Signup and view all the flashcards
Hypermutation
Hypermutation
Signup and view all the flashcards
Clonal selection
Clonal selection
Signup and view all the flashcards
Symptoms of myeloma
Symptoms of myeloma
Signup and view all the flashcards
Study Notes
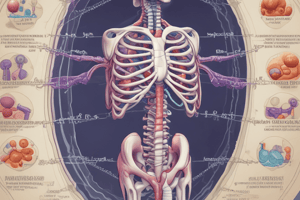
- Physiology and Biochemistry of Calcium Metabolism
- Year number: 2
- Week number: 5
- Week name: Back pain from a minor fall
Learning Objectives
- Describe the regulation of serum calcium concentrations including:
- Effects of regulatory hormones on the GI tract
- Effects of regulatory hormones on the kidney and bone
- Parathyroid gland's role in the distribution of calcium and phosphorus in the body
- Actions of PTH
- Role of vitamin D in calcium homeostasis
- Role of calcitonin in calcium homeostasis
- Discuss examples and the underlying mechanisms of pathologies like bone marrow disease, bony invasion, and parathyroid disease that can result in hyper and hypocalcaemia.
Calcium Storage
- 99% of calcium is stored in the bones and teeth (skeleton storage bank with hydroxyapatite) - Ca10(PO4)6(OH)2
- 1% is found in the blood
Calcium Needs
- Bone structure
- Neuronal communication
- Calcium is implicated to play roles in synaptic plasticity, memory, and neurotransmitter release
- Muscle contraction
- Blood clotting:
- Activates different factors (e.g., prothrombinase complex (Factors Xa and Va))
- Converts prothrombin to thrombin
- Cellular functions: exocytosis
Bone Remodelling
- Bones are continuously remodelled through mineral deposition (osteoblasts) and resorption (osteoclasts)
- Osteoblasts build bone using hydroxyapatite crystals (calcium & phosphate)
- Osteoclasts degrade (corrode) bone
Stem Call Lineage
- Stem cells differentiate into osteoblasts or macrophages
- Osteoblasts give rise to: lining cells and osteocytes
- Macrophages give rise to: osteoclasts
Osteoblast Development
- RUNX2 is a key transcription factor associated with osteoblast differentiation
Osteoclast Differentiation Regulation
- Osteoclasts are regulated by osteoblasts
- RANKL binds to the RANK receptor on osteoclast precursors, inducing osteoclast formation
- OPG inhibits osteoclastogenesis
- Both M-CSF and RANKL molecules are necessary for osteoclastogenesis and are widely involved in the differentiation of monocyte/macrophage derived cells
Osteoblasts
- Synthesize soft organic matter of bone matrix like collagen (osteoid)
- Lay down collagen fibres
- Fibres harden after being encrusted with calcium and phosphate minerals forming hydroxyapatite crystals
Osteoclasts
- Facilitate mineral resorption by dissolving the crystals and releasing the minerals into the blood
- Use pumping H+ out of the cell along with Cl- ions followed by electrical attraction (Cl-/HCO3- transporter)
- HCl dissolves bone minerals
- Release acid phosphatase and other proteases that digest collagen
Bone Cell Types
- Osteoprogenitor cells (progenitor, ancestor)
- Stem cells that differentiate into osteoblasts
- Osteoblasts
- Bone-forming cells (osteogenesis or ossification)
- Stress and fractures stimulate stem cells to rapidly multiply numbers of osteoblasts
- Secrete biochemical signals that may regulate bone remodelling, i.e. adjustments to bone shape and density to adapt to stress
- Osteocytes
- Multiple functions
- Some osteocytes reabsorb (dissolve) bone matrix while others deposit it (rebuild)
- Thought to be mechanosensor cells (strain sensors) that control the activity of osteoblasts and osteoclasts within a basic multicellular unit (BMU), a temporary anatomic structure where bone remodelling occurs
- Osteoclasts
- Giant cells
- Bone-dissolving cells found on the bone surface
- Formed by the fusion of stem cells and can contain 50+ nuclei
Bone Remodeling Phases
- Resting stage
- Bone resorption
- Reversal
- Bone formation
- Transition
- Mineralization
Bone Matrix Composition
- Collagen fibres
- Account for ~1/3 bone weight (organic matter)
- Provide flexibility
- Calcium phosphate (Ca3(PO4)2)
- Accounts for ~2/3 bone weight (inorganic matter)
- Interacts with calcium hydroxide (Ca(OH)2) to form crystals of hydroxyapatite (Ca10 (PO4)6(OH)2) salts
- Incorporates other salts (calcium carbonate, CaCO3) and ions (Na+, Mg2+, F-)
- Provides strength
Bone Mineralization
- Organic matter (Osteoid)
- Synthesized by osteoblasts
- Collagen, carbohydrate-protein complexes (glycosaminoglycans, proteoglycans, and glycoproteins)
- Inorganic matter
- 85% hydroxyapatite (crystallized calcium phosphate salt) [Ca10(PO4)6(OH)2]
- 10% calcium carbonate
- Other minerals (fluoride, sodium, potassium, and magnesium)
- Role of certain proteins: help regulate ordered deposition of minerals by regulating the amount and size of hydroxyapatite crystals
- Osteocalcin protein
- Secreted by osteoblasts
- Attaches to hydroxyapatite and binds calcium to bone allowing bone to be built in the right pattern which gives bone its strength
- Oseteonectin protein
- Secreted by osteoblasts during bone formation
- Initiates mineralization and promotes mineral crystal formation
- High affinity for collagen and calcium
- Osteopontin (bone sialoprotein I BSP-1)
- Secreted by osteoblasts, pre-osteoblasts, osteocytes, cardiac fibroblasts, and myoblasts
- Synthesis is stimulated by calcitriol (Vitamin D)
- High affinity for calcium
- Forms an integral part of the mineralized matrix and regulates crystal growth
- Contributes to bone remodeling by promoting osteoclastogenesis and osteoclast activity through CD44- and av3-mediated cell signalling.
- OPN serves to initiate the process by which osteoclasts develop their riffled borders to begin bone resorption- OPN contains and RGD integrin-binding motif
- Osteopontin takes a role in bone tissue destruction by two basic mechanisms
- Providing identification and adherence of osteoclastic cells by integrin av3-mediated OPN
- Modulation of osteoclastic function via integrin av3
- Osteocalcin protein
Demineralization of the Clavicle
- Bone: 50-70% minerals, 20-40% organic matrix, 5-10% water
- Dry weight matrix: 25% organic, 75% inorganic
- Organic component resists tension
- Inorganic component resists compression
- Removal of inorganic component makes bone flexible
- Removal of organic component makes bone brittle
Rickets
- Soft bones due to deficiency of calcium salts (Vitamin D deficiency)
Osteogenesis Imperfecta
- Brittle bone disease
- Genetic
- Excessively brittle bones due to lack of protein, collagen
- Mutations in COL1A1 and COL1A2 genes provide instructions for making type I collagen
Regulation
- Calcium homeostasis is regulated by calcitriol, calcitonin, and parathyroid hormone (PTH)
- Plasma Calcium: 2.2 - 2.6 mmol/l
- Ionised Calcium: 1.1 - 1.4 mmol/l
Calcitriol (Activated Vitamin D)
- Results in bone resorption in Kidney
- Results in the reduced excretion of Ca2+
- Results in the absorption of Ca2+ and phosphate
Parathyroid Hormone
- Secreted by the parathyroid gland on the posterior aspect of the thyroid gland in the neck
- Humans have 4 parathyroid glands
- Released when calcium levels decrease
- 1% drop in blood calcium levels doubles the secretion of PTH
- Stimulates osteoclast activity & inhibits osteoblast activity
Correction for Hypocalcemia (Parathyroid Hormone Dependent)
- Increased osteoclast activity leads to more bone resorption
- Reduced osteoblast activity leads to less bone deposition
- More urinary phosphate excretion
- Prevention of hydroxyapatite formation
- Less urinary calcium excretion & conservation of calcium
What increases blood Calcium
- Low calcium levels in plasma with parathyroid glands secreting parathyroid hormone (PTH)
- PTH stimulates osteoclasts to accelerate their erosion of bone matrix & release stored calcium ions into the body
- PTH enhances the calcium absorbing effects of calcitriol in the intestines
- Kidneys increasing renal production of calcitriol stimulates reabsorption in the kidney & intestines
Calcitonin
- Secreted by C cells in the thyroid gland
- Released when calcium levels increase
- Inhibits osteoclast activity and stimulates osteoblast activity
Correction for Hypercalcemia (Calcitonin Dependent)
- Reduced osteoclast activity & less bone resorption
- Increased osteoblast activity & more bone deposition
What decreases blood calcium?
- High calcium ion levels in plasma with C cells secreting calcitonin
- Calcitonin inhibits osteoclasts, deposit calcium ions within matrix of bones
- Decreasing PTH or calcitriol, there will be a decrease in Calcium ions in the intestines.
- Calcitonin inhibits excretory effect on the kidneys & suppressed Calcium ions reabsorption.
Hypercalcemia
- Excessive amounts of Ca2+ bind to the cell surface, increasing the charge difference across the cell membrane, which makes the Na+ channels less responsive
- Calcium blocks sodium channels and inhibits depolarization of nerve and muscle fibres,
- Nerve and muscle cells less responsive and excitable
- depression of the nervous system, emotional disturbances, muscle weakness, sluggish reflexes, sometimes cardiac arrest, at levels greater than 12 mg/dL
Hypercalcemia Causes
- Overactive parathyroid gland- small noncancerous tumors on one or more of the four parathyroid glands
- Bone cancer- metastases can increase osteoclast activity
- Multiple Myeloma increase osteoclast activity
- Other diseases such as tuberculosis and sarcoidosis that may raise levels of Vitamins D
- Digestive tract absorbing too much calcium
Hypocalcemia
- Leads to increased excitability in the nervous system
- Decreasing the charge differences across the cell membrane makes Na+ channels more responsive
- Results in muscle tremors, spasms, or cramps (tetany)
- Muscle of the larynx contracts tightly (laryngospasm), shutting airflow and cause suffocation, when Calcium plasma concentrations fall to 4 mg/dL or 1 mmol/l
Hypocalcemia Causes
- Vitamin D deficiency
- Diarrhea
- Thyroid Tumors
- May accidentally remove parathyroid gland
- Pregnancy & lactation
- Calcium is demanded by ossification of Fetal Skeleton & synthesis of Milk.
- Underactive Parathyroid Glands
- Treatment: IV/oral calcium supplements, & increase intake of Vitamins D Supplements.
Hypoparathyroidism
- Commonly caused by accidental damage during thyroid surgery
- Autoimmune disease of PTH
- Extensive Cancers radiations that affect radiation functions
- Low level of Magnesium prevents PTH releases
- Rapid decline leads to rapid calcium blood level decline, requiring therapies
- A fatal tetany occurs in 3-4 days
Hyperparathyroidism
- Typically caused by PTH primary secretions
- Gut failing and calcium deficiency leads to secondary hyperparathyroidism
- Secondary Vitamin D deficiency
- As the Kidney doesn't convert vitamins, this makes Bones deformed or Fragile, leading to more blood levels of calcium-phosphate; promotes more calcium phosphate
Defined Bone-Related Conditions
- Osteoarthritis is the degeneration of joint cartilage and the underlying bone
- Osteoporosis is decreased bone density
- Rheumatoid arthritis is an autoimmune inflammatory disorder of the hands and feet
Osteoporosis
- Common bone disease: loss of bone density
- Typical fracture is the head of the radius
- Focal & sub-trochanteric stress fracture
Multiple Myeloma
- Plasma Cells are the fully differentiated B-lymphocytes, that create specific antibodies
- Immature B cells mature into plasma, return to fight future infections
- When DNA plasma cells are damaged in lymphs, it creates tumours
- These tumours mainly accumulate in bone marrows, osteoclast activity surfaces
- 1500 new Australians are diagnosed each year, usually at 60+-year-old- or rarely under 40 years old
- M-proteins, myelomas, para-proteins & immunoglobulin chains are causes as renal failure factors.
- VDJ recombination is a process in the bone marrow where B cells assemble gene segments in B cells
- B cells receive high-affinity responses w Plasma from lymph & circulate to receptors
- There is somatic mutations for germinal centres for high affinity B cells
- Hypermutation in the lymph node diversifies antibody generation
- Clonal Selection produces more anti-bodies using immune systems
Symptoms of Multiple Myeloma
- Bone Pains
- Shortness of Breath
- Kidney Problems
- Confused Drowsiness
- Lower count or infections
Chronic Myeloid Leukaemia
- Increased myeloid in bone marrows (WBC)
- Characteristic chromosomal translocation called Philadelphia (22)
- Uncontrolled Kinase w Gleevec treatment
- Philadelphia chromosome & protein are genomic instability & abnormalities
- BCR-ABL protein drives to cell cycle to speedup & outgrow to control leading to death in the nucleus
- Increase in WBC, decrease in RBW with tear drop cells
- Immature Neutrophils increases with segmenting
- Stem Cells disorder, where is inability to function properly to fight & mature of the Granulocytes
- Granulocytes & eosinophils increases
- Anemia & Breathlessness
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.