Podcast
Questions and Answers
Why is maintaining calcium homeostasis crucial for normal body functions?
Why is maintaining calcium homeostasis crucial for normal body functions?
- It ensures the structural integrity of hair and nails.
- It regulates the body's sleep-wake cycle.
- It is required for normal skeletal and smooth muscle function, blood coagulation, and enzyme activity. (correct)
- It directly influences the production of melanin in the skin.
Extracellular calcium exists in what three forms?
Extracellular calcium exists in what three forms?
- Crystalline, amorphous, and chelated
- Bound to phosphate, attached to hydroxyapatite, and dissolved in plasma
- Free, bound to osteoclasts, and within bone marrow
- Ionized, protein-bound, and complexed with anions (correct)
Which of the following is NOT a significant source of dietary calcium?
Which of the following is NOT a significant source of dietary calcium?
- Dairy Products
- Tofu
- Fortified Cereals
- Potatoes (correct)
How do parathyroid hormone (PTH) and calcitonin interact to maintain calcium homeostasis?
How do parathyroid hormone (PTH) and calcitonin interact to maintain calcium homeostasis?
What is the direct stimulus for parathyroid hormone (PTH) release?
What is the direct stimulus for parathyroid hormone (PTH) release?
What is a primary action of parathyroid hormone (PTH) in the kidneys?
What is a primary action of parathyroid hormone (PTH) in the kidneys?
How does parathyroid hormone (PTH) indirectly stimulate intestinal absorption of calcium?
How does parathyroid hormone (PTH) indirectly stimulate intestinal absorption of calcium?
Which cells secrete calcitonin?
Which cells secrete calcitonin?
What is the primary physiological effect of calcitonin?
What is the primary physiological effect of calcitonin?
Which of the following is a direct effect of calcitonin on bone?
Which of the following is a direct effect of calcitonin on bone?
What stimulates the release of calcitonin?
What stimulates the release of calcitonin?
Which form of vitamin D is the active metabolite that primarily affects calcium homeostasis?
Which form of vitamin D is the active metabolite that primarily affects calcium homeostasis?
What are the two primary organs involved in the conversion of vitamin D to its active form, calcitriol?
What are the two primary organs involved in the conversion of vitamin D to its active form, calcitriol?
How does calcitriol primarily increase calcium absorption in the intestines?
How does calcitriol primarily increase calcium absorption in the intestines?
How do phosphate levels affect vitamin D activation?
How do phosphate levels affect vitamin D activation?
What is the underlying cause of rickets in children?
What is the underlying cause of rickets in children?
Which of the following is NOT a known function of calcium in the human body?
Which of the following is NOT a known function of calcium in the human body?
How does calcitonin influence kidney function related to calcium homeostasis?
How does calcitonin influence kidney function related to calcium homeostasis?
In the context of calcium metabolism, what is the role of osteoclasts?
In the context of calcium metabolism, what is the role of osteoclasts?
Which of the following best describes how PTH affects phosphate levels?
Which of the following best describes how PTH affects phosphate levels?
What is the main role of vitamin D-binding protein (transcalciferin) in calcium homeostasis?
What is the main role of vitamin D-binding protein (transcalciferin) in calcium homeostasis?
How does calcitriol regulate its own synthesis?
How does calcitriol regulate its own synthesis?
According to the information, what are some causes of vitamin D deficiency?
According to the information, what are some causes of vitamin D deficiency?
What is the underlying mechanism of how thiazide diuretics can affect calcium homeostasis?
What is the underlying mechanism of how thiazide diuretics can affect calcium homeostasis?
How do oestrogens affect calcium homeostasis?
How do oestrogens affect calcium homeostasis?
In addition to PTH, calcitriol and calcitonin, what other hormones play a role in Calcium Homeostasis?
In addition to PTH, calcitriol and calcitonin, what other hormones play a role in Calcium Homeostasis?
When plasma calcium levels fall, how does the body respond to restore balance?
When plasma calcium levels fall, how does the body respond to restore balance?
How does hypercalcaemia after meals get prevented?
How does hypercalcaemia after meals get prevented?
As part of calcium homeostasis, PTH causes conversion of 25(OH)-D3 to calcitriol, what is the main effect of this conversion?
As part of calcium homeostasis, PTH causes conversion of 25(OH)-D3 to calcitriol, what is the main effect of this conversion?
Flashcards
Calcium homeostasis
Calcium homeostasis
Maintaining stable calcium levels for normal body functions.
Calcium homeostasis maintenance
Calcium homeostasis maintenance
Process by which the body maintains stable calcium levels.
Parathyroid hormone (PTH)
Parathyroid hormone (PTH)
Hormone that increases plasma Ca2+ levels.
Calcitonin (CT)
Calcitonin (CT)
Signup and view all the flashcards
Vitamin D
Vitamin D
Signup and view all the flashcards
Calcium's role
Calcium's role
Signup and view all the flashcards
Calcium location
Calcium location
Signup and view all the flashcards
Chemical forms of calcium
Chemical forms of calcium
Signup and view all the flashcards
Sources of calcium
Sources of calcium
Signup and view all the flashcards
Parathyroid glands
Parathyroid glands
Signup and view all the flashcards
Chief cells
Chief cells
Signup and view all the flashcards
Control of PTH release
Control of PTH release
Signup and view all the flashcards
Kidneys with PTH
Kidneys with PTH
Signup and view all the flashcards
Bones when under PTH
Bones when under PTH
Signup and view all the flashcards
Calcitonin
Calcitonin
Signup and view all the flashcards
Calcitonin action
Calcitonin action
Signup and view all the flashcards
Vitamin D
Vitamin D
Signup and view all the flashcards
Vitamin D activation
Vitamin D activation
Signup and view all the flashcards
Calcitriol action
Calcitriol action
Signup and view all the flashcards
Vitamin D deficiency
Vitamin D deficiency
Signup and view all the flashcards
Study Notes
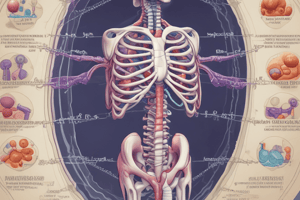
- The lecture covers the hormonal regulation of calcium metabolism
- The learning outcomes are to understand the importance of calcium homeostasis and how it is maintained, along with the physiological actions of the hormones involved
Hormones Involved
- Parathyroid hormone (PTH) raises plasma calcium levels
- Calcitonin (CT) decreases plasma calcium levels
- Vitamin D (Vit D) raises plasma calcium levels
- Other hormones in calcium homeostasis include oestrogens, growth hormone, and glucocorticoids
Calcium Homeostasis
- Dietary intake of 1000mg of calcium contributes to the plasma calcium level of 2.2 - 2.6mM
- Absorption of 350mg occurs in the gut, with 150mg secreted
- Faecal excretion accounts for 800mg
- Bone formation uses 500mg of calcium, balanced by bone resorption of 500mg
- Storage of calcium in bone is approximately 1kg
- PTH and Vitamin D increase reabsorption, while calcitonin decreases it
- Urinary excretion removes 200mg of calcium
- PTH and Vitamin D increase filtration, while calcitonin decreases it
Calcium Importance
- Calcium is essential for bone and teeth formation
- Calcium is essential for normal skeletal and smooth muscle function
- Calcium is essential for cellular division, adhesion, growth, blood coagulation and enzyme activity
- Calcium maintains activity of excitable tissues such as neuromuscular transmission, cellular hormone release, and heart function
Calcium Location and Concentration
- Over 95% of calcium is stored in bone
- About 1% of calcium is intracellular
- Extracellular plasma calcium concentration is 2.2-2.6mM
- Cytosolic intracellular calcium concentration is 10-100nM
Chemical Form
- 50% of calcium is free (active form)
- 45% is protein-bound (albumin & globulins)
- 5% is complexed with anions like bicarbonate, sulphate, citrate, and phosphate
- The ratio is influenced by plasma pH
Sources of Calcium
- Tofu
- Dairy products
- Bread
- Vegetables like curly kale, okra, horseradish, watercress, peas, broccoli, cabbage, celery, and parsnips
- Pulses like red kidney beans, soya bean, and soya products
- Cereals enriched with calcium
- Dried fruit like figs
- Nuts
Phosphate
- Phosphate metabolism is closely linked to calcium but less controlled
- Phosphate is essential for synthesizing DNA, RNA, ATP, membrane phospholipids, and bone
- Normal plasma phosphate range is 0.8-1.5mM
Parathyroid Hormone (PTH)
- Parathyroid glands consist of 4 oval, pea-sized bodies embedded in the back of the thyroid gland, found in all terrestrial vertebrates
- There are two types of epithelial cells in the parathyroid glands surrounded by connective tissue where chief cells are small, numerous, with clear cytoplasm and dense granules, and secrete PTH, and oxyphil cells are larger, fewer, with less granular cytoplasm and unknown function
PTH Production
- PTH is an 84 amino acid peptide derived from a larger precursor
- Rapid cleavage occurs after release in the liver and kidney, with a plasma half-life of 2-5 minutes
- The active portion consists of the 34 N-terminal amino acids
- Some cleavage occurs with in parathyroid glands
Control of Release of PTH
- Secretion is controlled by free ionised calcium concentration in plasma
- Low calcium concentration directly stimulates PTH release, involving a G protein-coupled cell surface calcium sensing receptor, with receptors found in all tissues
- Receptors have low affinity for Calcium²⁺ with an EC₅₀ of 3mM
- Magnesium has similar, but weaker, effects, with unclear physiological role
- Plasma phosphate levels have no direct effect
- Active Vitamin D metabolite, calcitriol, reduces PTH production
Physiological Actions of PTH
- PTH raises plasma free ionised Calcium²⁺ concentration
- There is interaction with active form of Vitamin D₃, calcitriol on the kidney, causing a rapid increase in distal tubule Calcium²⁺ reabsorption from glomerular filtrate and decreased phosphate reabsorption
- Plasma Calcium²⁺ and Magnesium²⁺ increases
- Plasma phosphate decreases
- PTH promotes formation of active vitamin D metabolite, calcitriol, in kidney tubular cells
Bone
- PTH stimulates rapid efflux of Calcium²⁺ across 'osteocyte-osteoblast bone membrane' into extracellular fluid
- PTH indirectly stimulates osteoclasts to release Calcium²⁺ and phosphate by bone resorption
- PTH increases number of osteoclasts involved
GI Tract
- PTH indirectly stimulates intestinal absorption of Calcium²⁺ and phosphate
- The effect is mediated by increased synthesis of calcitriol by kidney and takes at least 24 hours to occur
Calcitonin
- Calcitonin is a 32 amino acid peptide secreted by exocytosis from C cells of the thyroid gland
- This entire peptide is required for biological activity and has high species divergence
- Calcitonin stimulates specific plasma membrane receptors
- PTH is more vital when controlling Calcium²⁺ levels in Humans
Control of Release
- Secretion is controlled by free ionised Calcium²⁺ concentration in plasma
- High Calcium²⁺ concentration directly stimulates calcitonin release
- Gastrin releases calcitonin
- It prevents hypercalcaemia after meals and acts as a satiety hormone
- The plasma t₁ of calcitonin is 2-15 minutes and it is degraded in plasma and kidney
Physiological Actions
- Calcitonin decreases plasma free ionised Calcium²⁺ concentration
- It has a lowered effect of plasma Calcium²⁺, which increases PTH secretion and production of vitamin D metabolites
Bone
- Calcitonin decreases Calcium²⁺ efflux across osteocyte-osteoblast bone membrane
- It directly reduces osteoclast activity to resorb bone
- Calcitonin decreases formation of new osteoclasts from bone marrow
Kidney
- Calcitonin inhibits reabsorption of Calcium²⁺ and phosphate from loop of Henle and distal tubule
- It has an increased excretion of Calcium²⁺, Na⁺, K⁺, and decreased excretion of Mg²⁺
Vitamin D
- Vitamin D consists of essential fat-soluble sterols that can be classified as a hormone
- Vitamin D is obtained from diet or synthesised in the skin following sunlight (U.V.) exposure
- It is metabolised to produce active metabolite, calcitriol
- Vitamin D has the most important effects on bone, kidney and Gl tract
- Many additional target organs and it stimulates cell differentiation, and inhibits proliferation of skin and immune cells
- Vitamin D modulates seasonal and daily biorhythms
Metabolism of Vitamin D
- Inactive liver precursor, 7-dehydrocholesterol, is converted to cholecalciferol by U.V. light or photo-isomerisation in skin
- Vitamin D is obtained from diet or fish liver oils, sardines, herring, salmon, tuna, liver, eggs, cereals, margarine and some dairy products as it is often fortified with vitamin D
- The recommended dietary allowances for Vitamin D in U.K. 200IU micrograms
- Vitamin D is hydroxylated first in the liver to 25-hydroxy-cholecalciferol (25-(OH)D₃)
- Vitamin D is hydroxylated secondly in the kidney to the active form: alpha,25-dihydroxycholecalciferol (calcitriol, 1,25-(OH)₂D₃), or in skin
- Ergocalciferol is derived from plant sterol ergosterol and is hydroxylated similarly to produce alpha, 25-dihydroxycalciferol (calciferol, 1,25-(OH)₂D₂)
Transport and Control of Release
- Calcitriol is transported in blood bound to vitamin D-binding alpha-globulin or transcalciferin in the unbound form, which makes it active
- The plasma t₁₂ transport time is 3-6 hours
- 10 micrograms a day is needed to maintain Calcium²⁺ homeostasis
- PTH promotes 1alpha-hydroxylation to active metabolite and inhibits 24-hydroxylation to weakly active metabolite
- Calcitriol regulates its own synthesis by stimulating 24-hydroxylation and by negative feedback to inhibit 1alpha-hydroxylase with 1alpha-hydroxylase that is also stimulated by decreased phosphate
Mechanism of Action of Calcitriol
- Free calcitriol and calciferol are lipophilic and cross the plasma membrane
- Calcitriol binds to vitamin D receptors (VDR) in the nucleus VDR heterodimerises with the Retinoid X receptor (RXR) which either undergoes stimulation or inhibition of target genes
- The effects take several days to appear following the synthesis of cytosolic calcium binding proteins, calbindins (CaBP(9K) and CaBP(28K)), transporter pump protein (Ca-Mg-ATPase), osteocalcin
- Several VDR exist, with different distributions, and may be involved in genetic susceptibility to osteoporosis and colon cancer
- Calcitriol binds to membrane-associated receptors to increase intestinal Calcium²⁺ absorption
Cellular events
- Calcitriol helps open chloride channels, activate protein kinase C (PKC) and mitogen-activated protein (MAP) kinases
Physiological Actions of Calcitriol
- Raises plasma free ionised Calcium²⁺ concentration
GI tract
- Calcitriol promotes active absorption of Calcium²⁺ in the upper small intestine
Kidney
- Calcitriol promotes active absorption of Calcium²⁺, which is less important, and increases phosphate excretion
Bone
- Calcitriol promotes active resorption of Calcium²⁺ and increases phosphate absorption
- It indirectly activates osteoclasts and increases activity and potentiates effects of PTH
Clinical Disorder Associated with Calcitriol
- Vitamin D deficiency can cause Rickets in young children and osteomalacia (soft bones) in adults
- Vitamin D deficiency is most common in the Middle and Far East
- Causes are genetic, intestinal fat malabsorption, chronic liver disease, lack of sunlight, or dietary deficiencies
- Children express swollen growing ends of bone, bone bent and deformed, and 'bowed legs' as a result
- Adults express bone pain, partial fractures and muscle weakness
- Treatment includes Vitamin D analogues and Calcium²⁺ supplements
Regulation Steps
- A fall in the plasma Calcium concentration causes secretion of PTH from parathyroids
- Secretion of PTH from parathyroids causes mobilisation of Calcium from bone and conversion of 25-(OH)-D₃ to calcitriol
- Mobilisation of Calcium from bone causes a rise in the plasma Calcium concentration
- Conversion of 25-(OH)-D₃ to calcitriol causes increased Calcium absorption in the GI tract and decreased excretion of Calcium by the kidney
- Increased Calcium absorption in the GI tract and decreases excretion of Calcium by the kidney causes a rise in the plasma Calcium concentration
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.