Podcast
Questions and Answers
Why is type O blood considered a universal donor?
Why is type O blood considered a universal donor?
- It contains both anti-A and anti-B antibodies.
- The allele is dominant to both A and B.
- It does not contain A or B agglutinogens on its red blood cells.
- It possesses both A and B agglutinogens on its red blood cells. (correct)
What immunological event occurs in agglutination?
What immunological event occurs in agglutination?
- Red blood cells explode due to osmotic pressure. (correct)
- The complement system lyses foreign blood cells directly.
- Phagocytic white blood cells directly engulf foreign red blood cells.
- Antibodies bind to antigens on red blood cells, causing them to clump together.
How are ABO blood types determined in a lab setting?
How are ABO blood types determined in a lab setting?
- By observing the color change of the plasma after adding specific enzymes.
- By mixing diluted red blood cells with anti-A and anti-B antibodies and observing for agglutination.
- By centrifuging the blood sample and analyzing the density of the separated layers. (correct)
- By directly measuring the concentration of antibodies in the blood sample.
In the context of Rh blood types, what determines if a person is Rh-positive?
In the context of Rh blood types, what determines if a person is Rh-positive?
Why does erythroblastosis fetalis occur?
Why does erythroblastosis fetalis occur?
How does Rh immunoglobulin (RhoGAM) prevent erythroblastosis fetalis?
How does Rh immunoglobulin (RhoGAM) prevent erythroblastosis fetalis?
What is the most immediate threat to kidney function following a severe transfusion reaction?
What is the most immediate threat to kidney function following a severe transfusion reaction?
Why are xenografts almost always rejected without immunosuppressive therapy?
Why are xenografts almost always rejected without immunosuppressive therapy?
What is the primary immunological component responsible for graft rejection?
What is the primary immunological component responsible for graft rejection?
What is a key risk associated with using immunosuppressant drugs to prevent graft rejection?
What is a key risk associated with using immunosuppressant drugs to prevent graft rejection?
Which of the following transfusion reactions is most likely to cause acute kidney failure?
Which of the following transfusion reactions is most likely to cause acute kidney failure?
What is the significance of HLA antigens in transplantation?
What is the significance of HLA antigens in transplantation?
What is the primary reason for administering anti-Rh immunoglobulin to an Rh-negative mother after delivering an Rh-positive baby?
What is the primary reason for administering anti-Rh immunoglobulin to an Rh-negative mother after delivering an Rh-positive baby?
Which of the following is NOT a cause of acute kidney failure following a transfusion reaction?
Which of the following is NOT a cause of acute kidney failure following a transfusion reaction?
Why is it important to minimize the amount of donor plasma transfused in a mismatched transfusion?
Why is it important to minimize the amount of donor plasma transfused in a mismatched transfusion?
Which combination of parental Rh factors poses a risk of erythroblastosis fetalis in subsequent pregnancies?
Which combination of parental Rh factors poses a risk of erythroblastosis fetalis in subsequent pregnancies?
Following a transfusion reaction involving hemolysis, what substance is produced that can lead to jaundice?
Following a transfusion reaction involving hemolysis, what substance is produced that can lead to jaundice?
Why are individuals with suppressed immune systems more susceptible to certain types of cancers?
Why are individuals with suppressed immune systems more susceptible to certain types of cancers?
After receiving Rh positive blood, if an Rh negative patient undergoes a second transfusion with Rh positive blood, what is the likely outcome?
After receiving Rh positive blood, if an Rh negative patient undergoes a second transfusion with Rh positive blood, what is the likely outcome?
What is the function of immunosuppressive drugs following organ transplantation?
What is the function of immunosuppressive drugs following organ transplantation?
Flashcards
Blood Types (O, A, B)
Blood Types (O, A, B)
Blood classification based on the presence or absence of A and B antigens (agglutinogens).
ABO Gene Alleles
ABO Gene Alleles
A genetic locus with three alleles (A, B, O), where O is recessive to both A and B. Determines blood type.
Anti-A and Anti-B Agglutinins
Anti-A and Anti-B Agglutinins
Antibodies that develop when the corresponding antigen is not present on a person's red blood cells.
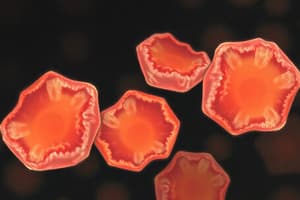
Agglutination
Agglutination
Signup and view all the flashcards
Blood Typing Process
Blood Typing Process
Signup and view all the flashcards
RH Blood Types
RH Blood Types
Signup and view all the flashcards
Anti-RH Agglutinin
Anti-RH Agglutinin
Signup and view all the flashcards
RH Immunoglobulin (RhoGAM)
RH Immunoglobulin (RhoGAM)
Signup and view all the flashcards
Mismatched Transfusion: Plasma Dilution
Mismatched Transfusion: Plasma Dilution
Signup and view all the flashcards
Mismatched Transfusion: Recipient Agglutinins
Mismatched Transfusion: Recipient Agglutinins
Signup and view all the flashcards
Hemoglobin Conversion
Hemoglobin Conversion
Signup and view all the flashcards
Acute Kidney Failure
Acute Kidney Failure
Signup and view all the flashcards
Autograft?
Autograft?
Signup and view all the flashcards
Isograft?
Isograft?
Signup and view all the flashcards
Xenograft
Xenograft
Signup and view all the flashcards
HLA Antigens
HLA Antigens
Signup and view all the flashcards
Graft Rejection: T-Cells
Graft Rejection: T-Cells
Signup and view all the flashcards
Study Notes
- Blood is classified into four major types: O, A, and B, based on the presence or absence of A and B agglutinogens.
- Type O blood lacks both A and B agglutinogens.
- The blood group genetic locus has three alleles.
- The type O allele is nonfunctional and recessive to both A and B alleles.
- Presence of the O gene combined with A or B results in A or B phenotype.
- There are at least 30 common and hundreds of rare antigens on human blood cell membranes.
- When type A agglutinogens are absent, anti-A agglutinins develop and when type B agglutinogens are absent, anti-B agglutinins develop.
- Type B blood contains anti-A agglutinins.
- Type A blood contains anti-B agglutinins.
- Type O blood contains both anti-A and anti-B agglutinins.
- Agglutinins form between 2 and 8 months after birth.
- Anti-A or anti-B plasma agglutinins mix with red blood cells containing A or B antigens, the agglutinins attach to the red blood cells.
- Agglutinins attach to red blood cells because they have two binding sites (IgG) or ten binding sites (IgM).
- A single agglutinin can attach to multiple red blood cells simultaneously, which causes clumping or agglutination.
- Agglutination causes clumps that plug small blood vessels, and are then attacked by phagocytic white blood cells, causing the release of hemoglobin into the plasma.
- Activation of the complement system and formation of the membrane attack complex can cause immediate hemolysis of red blood cells.
- For blood typing, RBCs are separated from plasma, diluted with saline, mixed with intact agglutinins, and observed under a microscope for clumping, which indicates an antibody-antigen reaction.
RH Blood Types
- There are six common types of Rh antigens, each called an Rh factor: C, D, E, c, d, and e.
- A person with a capital letter antigen does not have the lowercase version, and vice versa.
- Type D is most prevalent and antigenic.
- Individuals with the D antigen are Rh positive; those without are Rh negative.
- Rh-negative individuals can still experience transfusion reactions from other Rh antigens, though milder.
- When an Rh-negative person receives Rh-positive blood, anti-Rh agglutinins develop slowly, reaching maximum concentration in about four months.
- Subsequent transfusions of Rh-positive blood can cause a sudden and severe reaction when sufficient antibodies have developed.
Erythroblastosis Fetalis
- Erythroblastosis fetalis typically occurs when the mother is Rh-negative and the father is Rh-positive, resulting in an Rh-positive fetus.
- The mother develops anti-Rh agglutinins upon exposure to the fetus's Rh antigens.
- Maternal agglutinins cross the placenta and cause red blood cell agglutination in the fetus, leading to jaundice and anemia at birth.
- Maternal anti-Rh agglutinins can persist in the infant's blood for 1-2 months, destroying more red blood cells.
- Rapid red blood cell production by the fetal liver and spleen leads to enlargement of these organs and release of early-stage erythrocytes into circulation.
- Rh immunoglobulin (RhoGAM) is administered to Rh-negative mothers around 28-30 weeks of gestation and after delivering an Rh-positive baby to prevent sensitization to the Rh antigen.
Transfusion Reactions
- In mismatched transfusions, donor blood plasma is diluted by the recipient's blood, reducing the likelihood of agglutination of donor cells due to low agglutinin levels.
- Donor plasma agglutinins are not diluted and can react with recipient red blood cells.
- Hemoglobin released from hemolyzed red blood cells is converted into bilirubin by phagocytes and excreted in bile by the liver.
- High bilirubin concentrations can cause jaundice, typically occurring if more than 400 mL of blood is hemolyzed in less than a day.
- Acute kidney failure after transfusion reactions can be caused by toxic substances that induce renal vasoconstriction, hypotension due to red blood cell loss, and unbound hemoglobin blocking renal tubules.
Grafts
- Autografts and isografts contain the same antigens and survive normally.
- Xenografts almost always cause immune reactions and graft death within one day to five weeks unless therapy is used.
- There are 150 different antigen choices for human leukocyte antigens (HLA), resulting in over 1 trillion possible combinations.
- Except for identical twins, it's extremely rare for two individuals to have the same HLA antigens.
- Individuals with depressed immune systems can receive grafts without significant therapy.
- Allografts in individuals with healthy immune systems rarely resist rejection for more than a few weeks.
- T-cells are the primary cause of graft rejection, therefore their suppression is crucial for graft survival.
- Immunosuppressive drugs suppress T-cells or T-helper cells making individuals more susceptible to bacterial and viral infections.
- The incidence of cancer is higher in immunosuppressed individuals, possibly because the immune system normally destroys early cancer cells.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Description
Learn about the classification of blood into types O, A, and B based on agglutinogens. Type O blood lacks A and B agglutinogens. Understand the genetic locus with three alleles and the development of anti-A and anti-B agglutinins in the absence of corresponding agglutinogens.