Podcast
Questions and Answers
What is the most common blood tube used for collecting plasma?
What is the most common blood tube used for collecting plasma?
- Brownish-red-capped vial
- Black-capped tube
- Purple-capped vial (correct)
- Orange-capped vial
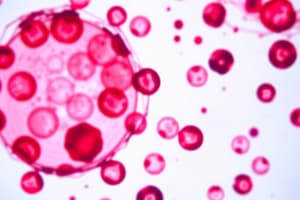
What is the primary function of red blood cells?
What is the primary function of red blood cells?
To transport oxygen and carbon dioxide
Platelets are large cells responsible for blood clotting.
Platelets are large cells responsible for blood clotting.
False (B)
What is the name of the precursor cells that differentiate into red blood cells, white blood cells, and platelets?
What is the name of the precursor cells that differentiate into red blood cells, white blood cells, and platelets?
Which of the following is NOT a component of a complete blood count (CBC)?
Which of the following is NOT a component of a complete blood count (CBC)?
What does the term 'anisocytosis' refer to in relation to red blood cells?
What does the term 'anisocytosis' refer to in relation to red blood cells?
What is the name of the process by which red blood cells are produced?
What is the name of the process by which red blood cells are produced?
Reticulocytes are mature red blood cells that lack a nucleus.
Reticulocytes are mature red blood cells that lack a nucleus.
Which of the following is a common cause of a low reticulocyte count?
Which of the following is a common cause of a low reticulocyte count?
What is the main component of red blood cells that gives them their red color?
What is the main component of red blood cells that gives them their red color?
Hematocrit (HCT) measures the percentage of whole blood occupied by red blood cells.
Hematocrit (HCT) measures the percentage of whole blood occupied by red blood cells.
What is the name given to the average volume of a red blood cell?
What is the name given to the average volume of a red blood cell?
Which of the following conditions is characterized by abnormally small red blood cells?
Which of the following conditions is characterized by abnormally small red blood cells?
What is the main purpose of a blood smear?
What is the main purpose of a blood smear?
What is the term used to describe an abnormally low white blood cell count?
What is the term used to describe an abnormally low white blood cell count?
What is the most abundant type of white blood cell in the blood?
What is the most abundant type of white blood cell in the blood?
The presence of band neutrophils in a blood smear indicates an active bone marrow response.
The presence of band neutrophils in a blood smear indicates an active bone marrow response.
What is the term used to describe the process by which neutrophils move from the marginal pool into the bloodstream?
What is the term used to describe the process by which neutrophils move from the marginal pool into the bloodstream?
Neutropenia is a condition characterized by an abnormally high neutrophil count.
Neutropenia is a condition characterized by an abnormally high neutrophil count.
What type of white blood cell is typically elevated during allergic reactions and parasitic infections?
What type of white blood cell is typically elevated during allergic reactions and parasitic infections?
Basophils release histamine and other inflammatory mediators during degranulation.
Basophils release histamine and other inflammatory mediators during degranulation.
What are the largest white blood cells?
What are the largest white blood cells?
Which of the following conditions is typically associated with an elevated monocyte count?
Which of the following conditions is typically associated with an elevated monocyte count?
What is the term for a decrease in lymphocyte count?
What is the term for a decrease in lymphocyte count?
Reactive lymphocytosis is a sign of a healthy immune response.
Reactive lymphocytosis is a sign of a healthy immune response.
In SARS-CoV-2 infection, what can cause a decrease in circulating lymphocyte numbers?
In SARS-CoV-2 infection, what can cause a decrease in circulating lymphocyte numbers?
Atypical lymphocytosis is a characteristic feature of infectious mononucleosis.
Atypical lymphocytosis is a characteristic feature of infectious mononucleosis.
What is the primary role of hemoglobin in red blood cells?
What is the primary role of hemoglobin in red blood cells?
Mature red blood cells in humans contain a nucleus.
Mature red blood cells in humans contain a nucleus.
What is the lifespan of a red blood cell in circulation?
What is the lifespan of a red blood cell in circulation?
Erythropoiesis occurs in the _____ of the body.
Erythropoiesis occurs in the _____ of the body.
Match the following terms with their correct definitions:
Match the following terms with their correct definitions:
What happens to reticulocytes after they enter the bloodstream?
What happens to reticulocytes after they enter the bloodstream?
A reticulocyte count provides a direct measure of the number of mature red blood cells in circulation.
A reticulocyte count provides a direct measure of the number of mature red blood cells in circulation.
What increase in production stimulates erythropoiesis in response to hypoxia?
What increase in production stimulates erythropoiesis in response to hypoxia?
What indicates a reduction in neutrophil count and is associated with an increased risk of infections?
What indicates a reduction in neutrophil count and is associated with an increased risk of infections?
Eosinophils are primarily involved in the hypersensitivity response associated with allergic disorders.
Eosinophils are primarily involved in the hypersensitivity response associated with allergic disorders.
What physiological condition can lead to neutrophilia?
What physiological condition can lead to neutrophilia?
A condition characterized by the presence of
______ is commonly associated with allergic disorders.
A condition characterized by the presence of ______ is commonly associated with allergic disorders.
Match the following conditions with their associated white blood cell changes:
Match the following conditions with their associated white blood cell changes:
Which of the following is NOT a common cause of neutropenia?
Which of the following is NOT a common cause of neutropenia?
Basophils increase during parasitic infections.
Basophils increase during parasitic infections.
List one physiological or pathological stimulus that can cause the release of neutrophils from the marginal pool into circulation.
List one physiological or pathological stimulus that can cause the release of neutrophils from the marginal pool into circulation.
What is the function of platelets in the blood?
What is the function of platelets in the blood?
The purple-capped vial used for blood collection contains additives that prevent coagulation.
The purple-capped vial used for blood collection contains additives that prevent coagulation.
What is the typical range of white blood cells (WBCs) in the blood per microliter?
What is the typical range of white blood cells (WBCs) in the blood per microliter?
After centrifugation, the two components of blood are _____ and _____ elements.
After centrifugation, the two components of blood are _____ and _____ elements.
Which type of stem cells gives rise to erythrocytes, platelets, and granulocytes?
Which type of stem cells gives rise to erythrocytes, platelets, and granulocytes?
The black-capped tube is specifically used for _____ tests.
The black-capped tube is specifically used for _____ tests.
Match the blood cell type with its characteristic:
Match the blood cell type with its characteristic:
The highest number of cellular elements present in blood are leukocytes.
The highest number of cellular elements present in blood are leukocytes.
What is the normal range for hemoglobin (HGB) in females?
What is the normal range for hemoglobin (HGB) in females?
The presence of hypochromia in red blood cells indicates a higher than normal content of hemoglobin.
The presence of hypochromia in red blood cells indicates a higher than normal content of hemoglobin.
What condition might be assessed with a blood smear if a patient shows unexplained jaundice?
What condition might be assessed with a blood smear if a patient shows unexplained jaundice?
The normal range for white blood cells (WBC) is _____ X 10^3/µL.
The normal range for white blood cells (WBC) is _____ X 10^3/µL.
Match the following terms with their descriptions:
Match the following terms with their descriptions:
Which of the following conditions can be indicated by examining a blood smear?
Which of the following conditions can be indicated by examining a blood smear?
Megaloblastic anemia may result from vitamin B12 or folic acid deficiency.
Megaloblastic anemia may result from vitamin B12 or folic acid deficiency.
What does MCV stand for in a complete blood count?
What does MCV stand for in a complete blood count?
What condition is typically associated with elevated lymphocyte counts that suggest an immune response?
What condition is typically associated with elevated lymphocyte counts that suggest an immune response?
Monocytopenia can indicate impaired production of monocytes and is associated with leukemia.
Monocytopenia can indicate impaired production of monocytes and is associated with leukemia.
What role do monocytes play during the transition to the recovery phase of an infection?
What role do monocytes play during the transition to the recovery phase of an infection?
An increase in basophils is known as __________.
An increase in basophils is known as __________.
Match the following immune conditions with their respective causes of lympocytopenia:
Match the following immune conditions with their respective causes of lympocytopenia:
What type of lymphocytosis is usually linked to neoplastic transformations like tumors and leukemias?
What type of lymphocytosis is usually linked to neoplastic transformations like tumors and leukemias?
A decrease in circulating lymphocyte numbers during SARS-CoV-2 infection indicates a healthy immune response.
A decrease in circulating lymphocyte numbers during SARS-CoV-2 infection indicates a healthy immune response.
Name two chronic infections that are typically associated with monocytosis.
Name two chronic infections that are typically associated with monocytosis.
What is the term used to describe the response of HSCs to pro-inflammatory signals during infection?
What is the term used to describe the response of HSCs to pro-inflammatory signals during infection?
Band neutrophils are a mature form of neutrophils that indicate a robust proliferation rate in the bone marrow.
Band neutrophils are a mature form of neutrophils that indicate a robust proliferation rate in the bone marrow.
What specific effect do inflammatory signals have on the fate of hematopoietic stem cells (HSCs)?
What specific effect do inflammatory signals have on the fate of hematopoietic stem cells (HSCs)?
A shift to the left in neutrophil nuclear segmentation indicates an increase in ______ neutrophils.
A shift to the left in neutrophil nuclear segmentation indicates an increase in ______ neutrophils.
Match the type of neutrophil with its corresponding description:
Match the type of neutrophil with its corresponding description:
What defines the homeostatic conditions for HSCs?
What defines the homeostatic conditions for HSCs?
Lymphoid output is increased in response to pro-inflammatory signals.
Lymphoid output is increased in response to pro-inflammatory signals.
What does a high presence of band neutrophils in the blood suggest?
What does a high presence of band neutrophils in the blood suggest?
Flashcards
Complete Blood Count (CBC)
Complete Blood Count (CBC)
A blood test panel that evaluates the three types of cells circulating in the blood: red blood cells (RBCs), white blood cells (WBCs), and platelets.
Plasma
Plasma
The liquid portion of blood, obtained after centrifuging a blood sample, containing clotting factors.
Purple-capped Vial (EDTA tube)
Purple-capped Vial (EDTA tube)
A small, purple-capped vial used for blood collection. It contains EDTA, an anticoagulant, preventing blood from clotting.
Hematocrit (HCT)
Hematocrit (HCT)
Signup and view all the flashcards
Hematopoietic Stem Cell (HSC)
Hematopoietic Stem Cell (HSC)
Signup and view all the flashcards
Mean Corpuscular Volume (MCV)
Mean Corpuscular Volume (MCV)
Signup and view all the flashcards
Mean Corpuscular Hemoglobin (MCH)
Mean Corpuscular Hemoglobin (MCH)
Signup and view all the flashcards
Mean Corpuscular Hemoglobin Concentration (MCHC)
Mean Corpuscular Hemoglobin Concentration (MCHC)
Signup and view all the flashcards
Red Cell Distribution Width (RDW)
Red Cell Distribution Width (RDW)
Signup and view all the flashcards
Blood Smear or Blood Film
Blood Smear or Blood Film
Signup and view all the flashcards
Megaloblastic Anemia
Megaloblastic Anemia
Signup and view all the flashcards
Eosinophils
Eosinophils
Signup and view all the flashcards
Basophils
Basophils
Signup and view all the flashcards
Monocytes
Monocytes
Signup and view all the flashcards
Lymphocytes
Lymphocytes
Signup and view all the flashcards
Leukopenia
Leukopenia
Signup and view all the flashcards
Leukocytosis
Leukocytosis
Signup and view all the flashcards
Neutropenia
Neutropenia
Signup and view all the flashcards
Neutrophilia
Neutrophilia
Signup and view all the flashcards
Absolute Neutrophil Count (ANC)
Absolute Neutrophil Count (ANC)
Signup and view all the flashcards
Cytokine Storm
Cytokine Storm
Signup and view all the flashcards
Atypical Lymphocytosis
Atypical Lymphocytosis
Signup and view all the flashcards
Microcytic Anemia
Microcytic Anemia
Signup and view all the flashcards
Polycythemia
Polycythemia
Signup and view all the flashcards
Hemoglobin (Hb)
Hemoglobin (Hb)
Signup and view all the flashcards
Erythropoiesis
Erythropoiesis
Signup and view all the flashcards
Reticulocytes
Reticulocytes
Signup and view all the flashcards
Hypochromic Anemia
Hypochromic Anemia
Signup and view all the flashcards
Iron Deficiency Anemia
Iron Deficiency Anemia
Signup and view all the flashcards
Anemia of Chronic Disease
Anemia of Chronic Disease
Signup and view all the flashcards
Thalassemias
Thalassemias
Signup and view all the flashcards
Pancytopenia
Pancytopenia
Signup and view all the flashcards
Thrombocytosis
Thrombocytosis
Signup and view all the flashcards
Neutrophils
Neutrophils
Signup and view all the flashcards
Margination
Margination
Signup and view all the flashcards
Coomb's Test
Coomb's Test
Signup and view all the flashcards
Hemoglobin
Hemoglobin
Signup and view all the flashcards
Hematocrit
Hematocrit
Signup and view all the flashcards
Anisocytosis
Anisocytosis
Signup and view all the flashcards
Poikilocytosis
Poikilocytosis
Signup and view all the flashcards
Hypochromia
Hypochromia
Signup and view all the flashcards
Macrocytosis
Macrocytosis
Signup and view all the flashcards
Marginal Pool
Marginal Pool
Signup and view all the flashcards
Margination to Circulation
Margination to Circulation
Signup and view all the flashcards
Eosinopenia
Eosinopenia
Signup and view all the flashcards
Basopenia
Basopenia
Signup and view all the flashcards
HSC dormancy
HSC dormancy
Signup and view all the flashcards
Lineage priming
Lineage priming
Signup and view all the flashcards
Inflammatory signal 'push' on HSCs
Inflammatory signal 'push' on HSCs
Signup and view all the flashcards
Inflammatory signal 'pull' on HSCs
Inflammatory signal 'pull' on HSCs
Signup and view all the flashcards
Band neutrophil
Band neutrophil
Signup and view all the flashcards
Segmented neutrophil
Segmented neutrophil
Signup and view all the flashcards
Arneth formula
Arneth formula
Signup and view all the flashcards
Shift to the left
Shift to the left
Signup and view all the flashcards
Lymphocytopenia
Lymphocytopenia
Signup and view all the flashcards
Reactive Lymphocytosis
Reactive Lymphocytosis
Signup and view all the flashcards
Primary Lymphocytosis
Primary Lymphocytosis
Signup and view all the flashcards
Lymphocyte Count in SARS-CoV-2 Infection
Lymphocyte Count in SARS-CoV-2 Infection
Signup and view all the flashcards
Study Notes
Blood Cell Analysis
- Blood analysis assesses platelets, white blood cells (WBCs), and red blood cells (RBCs).
- Blood samples are centrifuged to separate plasma from cellular elements.
- Platelets comprise 0.1% of whole blood.
- White blood cells (WBCs) make up 0.1% of the whole blood sample.
- Red blood cells (RBCs) compose 99.9% of the whole blood.
- Plasma constitutes 46-63% of the whole blood.
- Formed elements (formed by platelets and blood cells) constitute 37-54% of the whole blood.
Blood Collection
- Blood tube types vary depending on the test.
- EDTA tubes prevent clotting, allowing all blood cells to be analyzed.
- Orange-capped vials contain thrombin, an accelerator to speed up coagulation, for serum collection.
- Brownish-red-capped vials allow normal coagulation, for serum collection.
- Black-topped tubes are used for erythrocyte sedimentation rate (ESR) tests.
Cellular Elements
- Erythrocytes (RBCs) are the most abundant blood cells (4-6 million/µL), responsible for oxygen and carbon dioxide transport.
- Leukocytes (WBCs) range from 4,800-10,800/μL, and form from the lymphatic system.
- Platelets (thrombocytes) originate from megakaryocytes (bone marrow cells), and function in blood clotting.
- Hematopoietic stem cells (HSCs) reside in the bone marrow, and differentiate into myeloid and lymphoid stem cells.
- Myeloid stem cells produce erythrocytes, platelets, and granulocytes.
- Lymphoid stem cells produce lymphocytes.
Complete Blood Count (CBC)
- CBC is a panel of tests assessing red blood cells (RBCs), white blood cells (WBCs), and platelets.
- Cells are separated by size via apertures: platelets are smallest, RBCs are medium, and WBCs are largest.
- CBC is used for general health screening and to diagnose various health conditions.
- CBC can be used when there are signs and symptoms related to blood cell disorders, or to monitor the severity of an existing condition.
- CBC is also used to monitor the effectiveness of a treatment.
- Abnormal results necessitate further tests to determine if the patient has a severe condition.
Red Blood Cells (RBCs) or Erythrocytes
- RBCs are flexible biconcave disks without a nucleus.
- They are the most abundant cells in the blood.
- Their cytoplasm is rich in haemoglobin, responsible for the red color of the blood.
- RBCs circulate for 100-120 days before removal by macrophages.
- Normal RBCs exhibit a central pallor.
- RBC analysis might reveal anisocytosis (variation in size) or poikilocytosis (variation in shape).
Reticulocyte Count
- Reticulocytes are immature RBCs, retaining RNA and increasing hemoglobin
- A reticulocyte count helps assess red blood cell generation rates.
- Normal reticulocyte index is less than 3%.
- Increased index suggests a response to blood loss or anemia.
Hemoglobin (Hb)
- Hb is a red blood cell pigment essential for oxygen transport.
- Measuring Hb helps diagnose anemia.
- Normal Hb levels differ based on gender and age.
Hematocrit (HCT)
- HCT measures the percentage of blood volume occupied by RBCs.
- It's a critical parameter in assessing anemia and polycythemia (abnormal increase in RBCs).
- Normal HCT values differ based on gender.
RBC Indices
- These calculations provide physical characteristics of RBCs, including MCV (mean corpuscular volume), MCH (mean corpuscular hemoglobin), MCHC (mean corpuscular hemoglobin concentration), and RDW (red cell distribution width).
CBC Components and Normal Ranges
- Includes values for WBCs, RBCs, hemoglobin, hematocrit, MCV, MCH, MCHC, and RDW. Numerical values are generally provided for various populations (males, females, etc).
Blood Smear / Film Analysis
- Visual examination of blood to assess cell morphology, to diagnose conditions affecting blood cell populations.
- Used in conjunction with CBC results to get a clearer analysis
White Blood Cell (WBC) Analysis
- Monocytes: largest white blood cells differentiating into macrophages, playing a role in tissue repair and immune response.
- Lymphocytes: originate in bone marrow and secondary lymph tissues, crucial in immune responses.
- Variations in WBC count (e.g., leukopenia, leukocytosis) indicate various conditions.
- Lymphocytes are subdivided into T lymphocytes and plasma cells.
- Infections, inflammation, or malignancies can affect respective cell counts.
Eosinophils
- Eosinophils are primary role in combating parasitic infections; also implicated in allergic reactions (e.g. asthma) and certain inflammatory conditions.
Basophils
- Basophils are granular cells associated with allergic reactions, releasing histamine and other inflammatory mediators.
Additional Information
- Direct/Indirect Coombs test are performed for suspected autoimmune hemolytic anemia.
- Bone marrow suppression factors are linked to chemotherapy.
- Various blood disorders (e.g., anemia, infections, inflammation) might affect blood cell counts.
- Cytokine release can impact blood cell levels in severe conditions (e.g., COVID-19).
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.