Podcast
Questions and Answers
What is the primary function of the heart within the cardiovascular system?
What is the primary function of the heart within the cardiovascular system?
- To produce red blood cells.
- To pump blood throughout the body. (correct)
- To filter waste products from the blood.
- To regulate body temperature.
Which of the following describes the location of the heart?
Which of the following describes the location of the heart?
- Located in the cranial cavity, above the brain.
- Located behind the kidneys, near the spine.
- Located in the mediastinum, between the lungs. (correct)
- Located in the abdomen, below the stomach.
Which layer of the heart wall is responsible for its contraction?
Which layer of the heart wall is responsible for its contraction?
- Epicardium
- Pericardium
- Myocardium (correct)
- Endocardium
What is the role of the atrioventricular valves?
What is the role of the atrioventricular valves?
Which event occurs during ventricular systole?
Which event occurs during ventricular systole?
Where does unoxygenated blood enter after flowing from the superior and inferior vena cavae?
Where does unoxygenated blood enter after flowing from the superior and inferior vena cavae?
Which valve does blood pass through when moving from the right atrium to the right ventricle?
Which valve does blood pass through when moving from the right atrium to the right ventricle?
What is the correct formula for calculating cardiac output?
What is the correct formula for calculating cardiac output?
What does Starling's Law of the heart describe?
What does Starling's Law of the heart describe?
Which structure is considered the primary pacemaker of the heart?
Which structure is considered the primary pacemaker of the heart?
What is the intrinsic firing rate of the SA node?
What is the intrinsic firing rate of the SA node?
What is the function of the AV node?
What is the function of the AV node?
What happens when the SA node malfunctions or slows significantly?
What happens when the SA node malfunctions or slows significantly?
What is the intrinsic firing rate of the Purkinje fibers?
What is the intrinsic firing rate of the Purkinje fibers?
What is the role of electrodes in an ECG?
What is the role of electrodes in an ECG?
What does an ECG record?
What does an ECG record?
On an ECG, what does the P wave represent?
On an ECG, what does the P wave represent?
What does the QRS complex represent on an ECG?
What does the QRS complex represent on an ECG?
What does the T wave represent on an ECG?
What does the T wave represent on an ECG?
What is the standard paper speed for an ECG recording?
What is the standard paper speed for an ECG recording?
What does the vertical axis on ECG graph paper measure?
What does the vertical axis on ECG graph paper measure?
What is the time interval represented by one small square on standard ECG paper?
What is the time interval represented by one small square on standard ECG paper?
What is the duration of the PR interval?
What is the duration of the PR interval?
What is Einthoven's Law?
What is Einthoven's Law?
What does it mean if Einthoven's Law is not met?
What does it mean if Einthoven's Law is not met?
In standard limb leads, which lead is most useful for visualizing the P wave?
In standard limb leads, which lead is most useful for visualizing the P wave?
What is the typical progression of the QRS complex in the precordial (V) leads?
What is the typical progression of the QRS complex in the precordial (V) leads?
What is a common cause of wandering baseline artifact on an ECG tracing?
What is a common cause of wandering baseline artifact on an ECG tracing?
What causes AC interference artifact (60 Hz) on an ECG?
What causes AC interference artifact (60 Hz) on an ECG?
What action should be taken if electrical contact interruption is observed on an ECG tracing?
What action should be taken if electrical contact interruption is observed on an ECG tracing?
How are filters used in ECG monitoring?
How are filters used in ECG monitoring?
When is shaving a patient's chest needed for ECG electrode placement, and what must be obtained first?
When is shaving a patient's chest needed for ECG electrode placement, and what must be obtained first?
What is the primary purpose of Holter monitoring?
What is the primary purpose of Holter monitoring?
What is the meaning of the term 'ambulatory' in the context of ambulatory ECG monitoring?
What is the meaning of the term 'ambulatory' in the context of ambulatory ECG monitoring?
What is a vital instruction that must be given to a patient undergoing Holter monitoring?
What is a vital instruction that must be given to a patient undergoing Holter monitoring?
What is a key adaptation necessary when applying a Holter monitor to an older adult?
What is a key adaptation necessary when applying a Holter monitor to an older adult?
In a three-electrode ECG monitoring system, what is typically selected for arrhythmia monitoring and why?
In a three-electrode ECG monitoring system, what is typically selected for arrhythmia monitoring and why?
Flashcards
The Heart
The Heart
Main organ of cardiovascular system; a two-sided muscle pump.
Mediastinum
Mediastinum
Space in chest between lungs, where the heart is located.
Pericardium
Pericardium
Closed, two-layered sac around the heart.
Parietal Pericardium
Parietal Pericardium
Signup and view all the flashcards
Visceral Pericardium
Visceral Pericardium
Signup and view all the flashcards
Epicardium
Epicardium
Signup and view all the flashcards
Myocardium
Myocardium
Signup and view all the flashcards
Endocardium
Endocardium
Signup and view all the flashcards
Heart Valves
Heart Valves
Signup and view all the flashcards
Atrioventricular Valves
Atrioventricular Valves
Signup and view all the flashcards
Tricuspid Valve
Tricuspid Valve
Signup and view all the flashcards
Mitral (Bicuspid) Valve
Mitral (Bicuspid) Valve
Signup and view all the flashcards
Semilunar Valves
Semilunar Valves
Signup and view all the flashcards
Pulmonic Valve
Pulmonic Valve
Signup and view all the flashcards
Aortic Valve
Aortic Valve
Signup and view all the flashcards
Ventricular Systole
Ventricular Systole
Signup and view all the flashcards
Ventricular Diastole
Ventricular Diastole
Signup and view all the flashcards
Circulation
Circulation
Signup and view all the flashcards
Stroke Volume
Stroke Volume
Signup and view all the flashcards
Cardiac Output
Cardiac Output
Signup and view all the flashcards
Preload
Preload
Signup and view all the flashcards
Afterload
Afterload
Signup and view all the flashcards
Starling's Law
Starling's Law
Signup and view all the flashcards
Peripheral Vascular Resistance
Peripheral Vascular Resistance
Signup and view all the flashcards
Blood Pressure
Blood Pressure
Signup and view all the flashcards
Sinoatrial (SA) Node
Sinoatrial (SA) Node
Signup and view all the flashcards
Internodal Pathways
Internodal Pathways
Signup and view all the flashcards
Floor of right atrium above tricuspid valve.
Floor of right atrium above tricuspid valve.
Signup and view all the flashcards
AV Junction
AV Junction
Signup and view all the flashcards
Bundle of His
Bundle of His
Signup and view all the flashcards
Bundle Branches
Bundle Branches
Signup and view all the flashcards
Purkinje Network
Purkinje Network
Signup and view all the flashcards
Electrocardiogram (ECG/EKG)
Electrocardiogram (ECG/EKG)
Signup and view all the flashcards
Electrodes
Electrodes
Signup and view all the flashcards
Electrocardiograph
Electrocardiograph
Signup and view all the flashcards
Galvanometer
Galvanometer
Signup and view all the flashcards
ECG Graph Paper: 1 millimeter
ECG Graph Paper: 1 millimeter
Signup and view all the flashcards
ECG Leads
ECG Leads
Signup and view all the flashcards
Einthoven's Triangle
Einthoven's Triangle
Signup and view all the flashcards
P Wave
P Wave
Signup and view all the flashcards
Study Notes
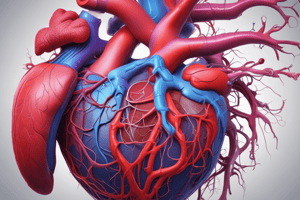
Anatomy of the Heart
- The heart is the main organ of the cardiovascular system
- It pumps blood throughout body while working with other systems to control heart rate and blood pressure
- Functions as a two-sided pump.
Location, Size, and Shape of the Heart
- Located in the mediastinum.
- Lies in front of the spinal column, behind the sternum, and between the lungs.
- Two-thirds of the heart lies to the left of the midline.
- The apex of the heart lies just above the diaphragm.
- The base of the heart is at the level of the third rib
- Roughly the size of owners closed fist
Layers of the Heart
- The pericardium is a closed, two-layered sac, includes parietal and visceral layers.
- The parietal pericardium is tough, nonelastic, and made of fibrous connective tissue.
- The visceral pericardium is a thin, serous inner layer of the pericardium.
- The epicardium is the smooth outer surface of the heart.
- The myocardium is the thick, middle layer of the heart composed of cardiac muscle cells, responsible for contractility.
- The endocardium is the innermost layer composed of connective tissue.
Valves of the Heart
- Four valves allow blood to flow in one direction.
- The two sets of valves are atrioventricular and semilunar.
Atrioventricular Valves
- Located between the atria and ventricles.
- Allow blood to flow from the atria into the ventricles.
- Prevent blood from flowing backward from the ventricles.
- The tricuspid valve has three cusps and is located between the right atrium and right ventricle.
- The mitral bicuspid valve has two cusps, located between the left atrium and left ventricle.
Semilunar Valves
- Prevent backflow of blood into the ventricles.
- Each semilunar valve contains three semilunar or moon-shaped cusps
- The pulmonic valve is located between the right ventricle and the pulmonary artery.
- The aortic valve is located between the left ventricle and the trunk of the aorta.
Heart Valve Function
- Chamber pressure governs the opening and closing of heart valves.
- Ventricular systole involves contraction of the ventricles, closing the atrioventricular valves and opening the semilunar valves.
- Ventricular diastole involves relaxation of the ventricles, opening the atrioventricular valves and closing the semilunar valves.
Coronary Arteries
- The two main coronary arteries are the left and right coronary arteries.
- The left coronary artery branches into the left anterior descending artery, the marginal branch, and the circumflex artery.
- The right coronary artery branches into the posterior descending artery.
Circulation
- Circulation is the movement of blood through a course (body) that leads back to the initial point (the heart).
- Blood exits the heart in arteries, exchanges waste for oxygen in capillaries, and returns to the heart in veins.
Cardiac Cycle
- The heart functions as a unit with both atria contracting.
- Ventricles fill with blood to their limits.
- Blood is ejected into both the pulmonary and systemic circulations when the ventricles contract.
- The cardiac cycle represents the actual time sequence between ventricular contraction and relaxation.
Ventricular Systole and Diastole
- Ventricular systole is the simultaneous contraction of the ventricles, closing the mitral and tricuspid valves.
- Ventricular diastole is the simultaneous relaxation of the ventricles, opening the mitral and tricuspid valves.
- Pulmonary and aortic valves open during systole and close during diastole.
Stroke Volume and Cardiac Output
- Stroke volume is the volume of blood pumped out of one ventricle of the heart in a single beat.
- Stroke volume is estimated to be 70 cubic centimeters per beat.
- Normal heart rate is 60 to 100 beats per minute (BPM)
- Tachycardia is an increased heart rate (over 100 bpm), while bradycardia is a decreased heart rate (under 60 bpm).
Calculating Cardiac Output
- Cardiac output measures the amount of blood pumped by the left ventricle in one minute.
- Cardiac Output = Stroke Volume x Heart Rate.
- For example, if heart rate is 80 BPM and stroke volume is 70 cc per beat, the resulting cardiac output would be 5,600 cc per minute or 5.6 L/min.
- Preload is the pressure in the ventricles at the end of diastole.
- Afterload is the resistance against which the heart must pump.
- Starling's Law states that the more the myocardial fibers are stretched, the more the subsequent contraction will be.
- Peripheral vascular resistance is the amount of opposition to blood flow offered by the arterioles.
- Vasoconstriction and vasodilation determine peripheral vascular resistance.
- Blood Pressure = Cardiac Output x Peripheral Vascular Resistance.
The Cardiac Conduction System
- The sinoatrial (SA) node is located in the upper posterior portion of the right atrial wall of the heart, acting as the primary pacemaker.
- The firing rate of the SA node is 60 to 100 beats per minute (BPM).
- Depolarization and myocardial contraction occur after the impulse leaves the SA node
Internodal Pathways
- Internodal pathways receive electrical impulses as they exit the SA node.
- Distribute the impulse throughout the atria.
- Transmit the impulse from the SA node to the AV node.
AV Node and Junction
- The atrioventricular (AV) node is located on the floor of the right atrium above the tricuspid valve.
- Electrical activity is delayed by 0.05 seconds to allow for more complete filling of the ventricles.
- It is the only pathway for atrial electrical impulses to reach the ventricles.
- The AV junction is where the AV node joins the bundle of His.
- If the SA node fails or slows significantly, AV junctional tissues initiate electrical activity as a secondary pacemaker.
Bundle of His and Bundle Branches
- The bundle of His is a conduction pathway that leads out of the AV node, located at the top of the interventricular septum.
- It is referred to as the common bundle, with the ability to self-initiate electrical activity at an intrinsic firing rate of 40 to 60 beats per minute.
- The bundle of His divides into two main bundle branches: the right and left bundle branches.
- Conduct electrical activity from the bundle of His to the Purkinje network
Purkinje Fibers
- Are a network of fibers that receive conductive signals from the AV nodes.
- Carry impulses directly to ventricular muscle cells.
- Simultaneously activate the left and right ventricles by directly stimulating the ventricular myocardium
- Firing rate of 20 to 40 beats per minute
Electrocardiogram (ECG/EKG)
- Used to determine or detect abnormal heart rhythms (arrhythmias), palpitations, blocked or narrowed arteries (coronary artery disease), or effectiveness of heart disease treatments.
Basis of the ECG
- Electrical activity is sensed by electrodes placed on the skin surface and recorded in the form of an electrocardiogram.
- A cardiac monitor depicts electrical impulses on a monitor screen or oscilloscope.
- Used to detect chest pain; dizziness, lightheadedness, or confusion; heart palpitations; rapid pulse; shortness of breath; weakness; fatigue; or a decline in exercise ability.
Electrocardiograph Components
- The electrocardiograph is the apparatus used to generate electrocardiograms.
- The ECG is the graphic tracing of electrical activity of the heart, NOT the mechanical activity.
- Electrical impulses from the heart are picked up by electrodes and conducted through lead wires into the machine.
- Electrodes are composed of a substance that is a good conductor of electricity.
- The electrical impulses given off by the heart are very small (around 0.002 volt).
- To produce a readable ECG, impulses are amplified by a device known as an amplifier, located within the electrocardiograph.
- Amplified voltages are changed into mechanical motion by a galvanometer and recorded on the electrocardiograph paper by a terminal print head.
ECG Graph Paper
- Electrical impulses present on the skin surface are very low voltage, so they are amplified by an ECG machine.
- The printed record of the electrical activity of the heart is called a rhythm strip, and the record is printed on graph paper at a set speed (25 mm/sec) to demonstrate the electrical conductivity of the heart.
- The recording is a plot of voltage on the vertical axis against time on the horizontal axis.
- Electrodes are connected to a galvanometer that records a potential difference.
- Electrocardiographic paper is divided into small squares, with each millimeter (mm) in width representing a time interval of 0.04 seconds.
- Darker lines divide the paper every fifth square, vertically and horizontally.
- Large squares measure 5 millimeters in height and width, representing a time interval of 0.20 seconds.
- Paper leaves the machine at a constant speed of 25 millimeters per second (mm/sec).
- Amplitude or voltage is measured on the vertical line on the graph paper (y-axis), and time is measured on the horizontal line (x-axis).
- Doubling the standard rate (25 mm/sec) can reveal subtle ECG findings hidden at slower rates.
Leads
- Electrodes are adhesive pads containing conductive gel which attach to patient's skin, enabling electrical impulses to be recorded from the heart.
- Leads are how electrodes are connected to the cardiac monitor which include positive, negative, and ground.
- Bipolar leads have one positive and one negative.
- Limb leads include leads I, II, and III, with lead II being the most common as it visualizes the P-wave.
- Lead I runs from the right arm (-) to the left arm (+).
- Lead II runs from the right arm (-) to the left leg (+).
- Lead III runs from the left arm (-) to the left leg (+).
Einthoven's Triangle
- Imaginary inverted triangle formed around the heart through proper placement of bipolar leads
- Top is formed by Lead I, the right side by Lead II, and the left side by Lead III.
- Einthoven stated that Lead I + Lead III = Lead II, which is called Einthoven's law.
- Each lead represents a different view of the heart.
ECG Planes
- The 12-lead ECG views the heart in two distinct planes: the frontal plane and horizontal plane.
- The frontal plane is what the limb leads look at, while the horizontal plane is what the vector (V) leads look at
Positioning and Placement of Electrodes
- Two-arm leads should be placed between the shoulder and wrist.
- Two-leg leads should be placed between the hips and ankles.
- Augmented limb leads include aVR, aVL, and aVF, utilizing the four limb leads.
- The heart is the focal point, and current flows from the heart outward to the extremities.
- The ECG machine must boost amplification due to positions of these leads.
- Chest leads, called precordial or vector (V) leads, look at the horizontal or transverse plane.
Quality of the ECG and Standardization
- The electrocardiograph must be standardized to ensure an accurate and reliable recording for QRS complex amplitude.
- An application of one 1 millivolt (mV) of electricity causes the stylus to move ten 10 millimeters high or ten (10) small squares.
- The standardization mark is automatically recorded by three-channel electrographs on the tracing.
- Most ECG machines automatically place a standardization mark at the beginning of the tracing.
- Ensure this is at the beginning of each patient's tracing.
- The paper consists of a black or blue base with a white plastic coating.
- A heated stylus moves over the heat-sensitive paper and melts away the plastic coating, resulting in the recording of the ECG.
ECG Wave Forms and Intervals
- Wave or waveform refers to movement away from the baseline or isoelectric line, positive deflection is above the isoelectric line and negative deflection is below.
- Electrical impulses that leave the SA node produce waveforms on the graph paper.
- One complete cardiac cycle is represented by the P, Q, R, S (QRS complex), and T waves.
- First wave is produced by an electrical impulse from the SA node with a smooth, rounded upward deflection.
- Representing depolarization of the left and right atria occurring in 0.10 seconds.
- Also the time for an impulse to travel from the SA node through internodal pathways in the atria toward the ventricles.
- Time interval from the start of the P wave to the start of the QRS complex is 0.12 to 0.20 seconds.
- Includes Q, R, and S waves which represents conduction of the impulse from the bundle of His through the ventricular muscle, causing ventricular depolarization.
- Time interval for QRS is less than 0.12 seconds measured from the start to end.
- Isoelectric Point
- Time interval during which the ventricles are depolarized and repolarization begins.
- Follows the ST segment, representing ventricular repolarization, is slightly rounded, and has a positive deflection.
T Wave and QT Interval
- Represents the resting phase of the cardiac cycle. From the beginning of the QRS complex to the end of the T wave, which represents all ventricular activity (depolarization and repolarization), the QT interval is normally 0.28-0.44 sec.
- A U wave is usually absent but if present, its height should be < 1/3 of the T wave.
- When a tall U wave presents, it indicates electrolytes imbalance mainly low K+ in blood (Hypokalemia).
- Leads I, II, III, QRS is a positive deflection while aVR QRS is a negative deflection.
- aVL QRS is biphasic and aVF QRS is a positive deflection.
- V1 QRS is a negative deflection.
- QRS progresses through until V6.
- V6 QRS is a positive deflection.
Artifacts
- Produced by something other than than the electrical activity of the patient's heart.
- Indicates a technical problem with either the patient set-up, or with the ECG instrument itself.
- Erratic spikes of varying sizes that can interrupt wave forms or the baseline.
- Patient is the source usually found only in affected leads.
Troubleshooting Artifacts
- Ensure that the patient is relaxed and comfortable and that body parts are well supported on the bed
- Ask patients to place hands under their buttocks to reduce involuntary shaking and check limp sensor position to ensure that there are no tremors
- Move limp sensor to torso if tremors cannot be controlled
- Has dry electrodes, dangling lead wires, loose electrodes or broken lead wires, use new electrodes and change the wires.
AC Artifacts
- Looks as a series of uniform small spikes, making the baseline like a thick line, alternative name is 60 Hz interference.
- Electrical currents in nearby equipment or a bad wiring can leak small amounts of the electrical energy that the ECG picks up.
- Has a poorly grounded ECG machine or it is not equipped to filter out the electrical interference, loose or broken ground connector or power cord.
Electrical Equipment
- Right leg electrode may be improperly connected or not connected at all.
- Patients' bed may not grounded; patient touching metal frame.
- Electrodes and/or cable tips may be corroded or dirty.
- Use three-pronged grounded outlet, do not cross lead wires, unplug other electrical appliances in the room, move table away from wall, and turn off fluorescent lights.
- The filters on the ECG are used to remove high frequency muscle artifact and external interference.
- However, it will cause slight adjustments to the ST segments and most ECGs are done with the filter "on".
Holter Monitor
- Used to rule out intermittent arrhythmias or ischemia that could be missed on a routine EKG.
- It records the electrical activity of the heart for 24 -72 hours and detects cardiac abnormalities that occur while the patient is engaged in daily activities.
- Explain each step of the procedure to the patient and allow them to ask questions.
Application of the Holter Monitor
- Apply the monitor has been prepared and after the patient (clothing and position has been prepped).
- Prepare skin by abrading a thin layer of skin where electrodes will go.
- Place and tape the five electrodes to trunk of body (instead of arms and legs).
- The EKG signals are recoded on a magnetic tape or digital flash media; Give patient care; instructions/guidelines for Holter monitor and diary.
- Patient returns after prescribed hours/days (typically 1-3) to the facility and the data is entered into a Computer.
- Computer scans for abnormalities.
Quality of a Holter Monitor Recording
- Correct patient information.
- Baseline of tracing smooth Standardization mark present.
- Einthoven's Law is met (II= I + III), aVR lead is a negative or downward deflection.
- R wave progression in chest leads and Lead II is a positive deflection.
Adapted Use of Holter Monitors
- Performed inside medical facility; Uses 3 or 5 electrodes on chest.
- Transmits to a central location where multiple patients may be monitored.
- Patient diary not required.
- Twelve-lead is the standard form and 5-lead monitoring take electrodes that are electrodes that are used for the limbs in 12-lead monitoring and place them on the chest wall.
- 5-lead monitoring is the same as 3-lead monitoring, with two additional electrodes to enable the monitoring of extra leads and help improve ST elevation readings.
- monitors leads I, II, III aVR, aVL, aVF, and V.
- Uses 5 electrodes (RA, RL, LA, LL and Chest).
- Monitor displays the bipolar leads (I, II and III) and a single unipolar lead (depending on position of the brown chest lead (positions V1–6).
Electrode Systems
- In this system you are recording Right arm (RA – white) - below the right, Left arm (LA – black) – below the left clavicle and Left leg (LL - red) - on the lower part of the ribcage, on the left-hand side.
- These systems are simple, cheap and easy to use.
- The available leads with this setup are I, II and III
Transtelephonic Monitoring
- Monitoring is primarily used to evaluate pacemaker function or monitor patients for 30 days or more.
- Information stored in the monitor; methods of transmission Telephone land line, Cell phone tower and Wi-Fi.
- It has two types
- Post-symptom event monitor
- Loop memory monitor
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.