Podcast
Questions and Answers
Where can pain be referred in relation to myocardial infarction?
Where can pain be referred in relation to myocardial infarction?
- Arms, back, abdomen, neck, or teeth (correct)
- Legs and arms only
- Head and shoulders only
- Chest only
What is the result of a thrombus or embolus in a coronary artery?
What is the result of a thrombus or embolus in a coronary artery?
- The heart valve structure is damaged
- Some or all tissue distal to the blockage dies (correct)
- The blood flow increases to compensate
- The heart stops pumping efficiently
What is a long-term result of a myocardial infarction?
What is a long-term result of a myocardial infarction?
- The size of the infarct and position affect pumping efficiency and conduction efficiency (correct)
- The heart valve structure is damaged
- Increased pumping efficiency
- The blood flow increases to compensate
What is a potential drawback of reperfusion therapy?
What is a potential drawback of reperfusion therapy?
What is the function of the valves in the heart?
What is the function of the valves in the heart?
When do the valves open in the heart?
When do the valves open in the heart?
What is the function of chordae tendineae in the heart?
What is the function of chordae tendineae in the heart?
What is the purpose of the semilunar valves?
What is the purpose of the semilunar valves?
What is the characteristic of the SA node that makes it the origin of cardiac excitation?
What is the characteristic of the SA node that makes it the origin of cardiac excitation?
What is the function of the AV bundle (Bundle of His)?
What is the function of the AV bundle (Bundle of His)?
What is the characteristic of pacemaker potentials that makes them autorhythmic?
What is the characteristic of pacemaker potentials that makes them autorhythmic?
What is the purpose of the long absolute refractory period in cardiac muscle action potential?
What is the purpose of the long absolute refractory period in cardiac muscle action potential?
What is the term for an irregular rhythm that is too slow?
What is the term for an irregular rhythm that is too slow?
What is the term for an irregular rhythm that is too fast?
What is the term for an irregular rhythm that is too fast?
What is the function of the Purkinje fibers?
What is the function of the Purkinje fibers?
What is the effect of changes in K+ and Ca2+ ion concentrations on cardiac rhythm?
What is the effect of changes in K+ and Ca2+ ion concentrations on cardiac rhythm?
What is the location of the heart in the body?
What is the location of the heart in the body?
What is the function of the pericardium?
What is the function of the pericardium?
What is the visceral layer of the pericardium also known as?
What is the visceral layer of the pericardium also known as?
What is cardiac tamponade?
What is cardiac tamponade?
What is the middle layer of the heart wall?
What is the middle layer of the heart wall?
What is the purpose of the gap junctions in cardiac muscle?
What is the purpose of the gap junctions in cardiac muscle?
What is the path of blood flow through the heart?
What is the path of blood flow through the heart?
What is the purpose of the coronary circulation?
What is the purpose of the coronary circulation?
What is angina pectoris?
What is angina pectoris?
What is the percentage of normal arterial blood flow that the heart can survive on?
What is the percentage of normal arterial blood flow that the heart can survive on?
What is the result of rapid, fluttering, out of phase contractions in the heart?
What is the result of rapid, fluttering, out of phase contractions in the heart?
What is the function of the AV node in the heart?
What is the function of the AV node in the heart?
What is the role of the sympathetic nervous system in regulating heart rate?
What is the role of the sympathetic nervous system in regulating heart rate?
What is the formula for calculating cardiac output?
What is the formula for calculating cardiac output?
What is the term for the amount of blood pumped by each ventricle in 1 minute?
What is the term for the amount of blood pumped by each ventricle in 1 minute?
What is the factor that determines the degree of stretching of cardiac muscle cells before contraction?
What is the factor that determines the degree of stretching of cardiac muscle cells before contraction?
What is the effect of high blood pressure on the heart?
What is the effect of high blood pressure on the heart?
What is the term for the maximum amount of blood that can be pumped by the heart in 1 minute?
What is the term for the maximum amount of blood that can be pumped by the heart in 1 minute?
What is the effect of sympathetic nervous stimulation on contractility?
What is the effect of sympathetic nervous stimulation on contractility?
What is the term for the volume of blood in the heart after it fills?
What is the term for the volume of blood in the heart after it fills?
Flashcards are hidden until you start studying
Study Notes
Location and Structure of the Heart
- The heart is located in the thoracic cavity, in the mediastinum, and is approximately the same size as a closed fist.
- The base of the heart is the wider, superior portion, and the apex is the point.
- The heart is protected by the pericardium, a tough, inelastic sac of fibrous connective tissue.
Pericardium
- The pericardium consists of two layers: the fibrous pericardium and the serous pericardium.
- The fibrous pericardium is attached to the diaphragm and anchors the heart, preventing it from overfilling.
- The serous pericardium has two layers: the parietal layer and the visceral layer.
- The parietal layer produces a serous fluid that reduces friction as the heart contracts and twists.
- The visceral layer forms the epicardium, the outer layer of the heart wall.
Heart Wall
- The heart wall has three layers: the epicardium, the myocardium, and the endocardium.
- The epicardium is the outer layer, a thin, transparent layer.
- The myocardium is the middle layer, a mass of cardiac muscle.
- The endocardium is the inner layer, a smooth lining for the chambers and valves.
Cardiac Muscle
- Cardiac muscle fibers are connected by intercalated discs, which allow action potentials to pass from fiber to fiber.
- Gap junctions and desmosomes ("spot welds") help to coordinate contractions and prevent cardiac fibers from separating.
Surface of the Heart
- The heart has external landmarks, including the atrioventricular grooves and the anterior/posterior interventricular sulcus.
- The coronary vessels run in these grooves, supplying blood to the heart.
Chambers of the Heart
- The heart has four compartments: the right and left atria, and the right and left ventricles.
- The interatrial septum separates the atria, and the interventricular septum separates the ventricles.
- The left ventricular wall is thicker than the right ventricular wall, as it must pump blood throughout the body and against gravity.
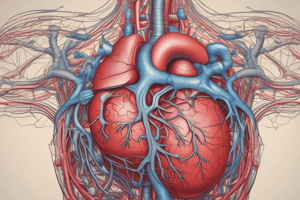
Blood Flow through the Heart
- The right atrium receives deoxygenated blood from the superior vena cava, inferior vena cava, and coronary sinus.
- The blood flows from the right atrium to the right ventricle, and then to the pulmonary trunk, which carries it to the lungs for gas exchange.
- The oxygenated blood from the lungs returns to the left atrium, and then flows to the left ventricle, which pumps it to the body via the aorta.
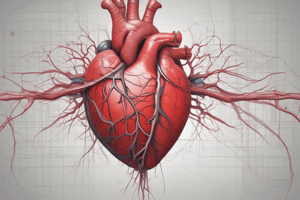
Myocardial Blood Supply
- The myocardium has its own blood supply, which branches off the aorta.
- The coronary vessels supply blood to the cardiac muscle, and the coronary veins return deoxygenated blood to the coronary sinus.
- The coronary circulation is crucial for the heart's function, and problems with it can lead to ischemia and infarction.
Pathologies
- Pericarditis is an inflammation of the pericardium, which can cause pain and damage to the lining tissues.
- Cardiac tamponade is a buildup of fluid in the pericardial cavity, which can lead to cardiac failure.
- Coronary circulation pathologies, such as emboli, atherosclerosis, and smooth muscle spasms, can cause ischemia and infarction.
- Angina pectoris is a classic chest pain caused by temporary myocardial ischemia.
- Myocardial infarction (heart attack) occurs when a thrombus or embolus blocks a coronary artery, leading to tissue death and scarring.
Valve Structure and Function
- The heart has four valves: the tricuspid and bicuspid valves, which separate the atria and ventricles, and the aortic and pulmonary semilunar valves, which prevent backflow of blood from the arteries.
- The valves are made of dense connective tissue covered by endocardium, and they open and close passively in response to pressure changes.
- Chordae tendineae and papillary muscles help to prevent the valves from opening too widely.
Conduction System and Pacemakers
- The heart has a conduction system, which generates and propagates electrical signals that control the heartbeat.
- The sinoatrial (SA) node is the primary pacemaker, firing 60-100 times per minute.
- The atrioventricular (AV) node and the bundle of His are also part of the conduction system.
- The Purkinje fibers are specialized fibers that transmit the electrical signals to the ventricular muscle.
- Arrhythmias are irregular rhythms, which can be caused by problems with the conduction system or pacemakers.### Cardiac Electrophysiology
- Fibrillation: rapid, fluttering, out of phase contractions, no pumping, heart resembles a squirming bag of worms
- Ectopic pacemakers: abnormal pacemakers controlling the heart due to SA node damage, caffeine, nicotine, electrolyte imbalances, hypoxia, or toxic reactions to drugs
- Heart block: AV node damage, severity determines outcome, may slow conduction or block it
Conduction System and Pacemakers
- SA node damage: AV node can take over, firing at 40-50 beats/min
- If AV node is out, AV bundle, bundle branch, and conduction fibers fire at 20-40 beats/min
- Artificial pacemakers: can stimulate single or dual chambers, can be activity-dependent
Atrial, Ventricular Excitation Timing
- 0.05 sec from SA to AV node
- 0.1 sec to get through AV node, conduction slows
- Allows atria time to finish contraction and better fill ventricles
- Once action potentials reach AV bundle, conduction is rapid to rest of ventricles
Extrinsic Control of Heart Rate
- Basic rhythm of the heart is set by internal pacemaker system
- Central control from medulla is routed via ANS to pacemakers and myocardium
- Sympathetic input: norepinephrine, increases heart rate
- Parasympathetic input: acetylcholine, decreases heart rate
Electrocardiogram
- Measures the sum of all electro-chemical activity in myocardium at any moment
- P wave, QRS complex, T wave
Cardiac Cycle: Electrical & Mechanical Events
- Systole: heart muscle contracts, pushes blood out of body
- Diastole: heart relaxes, fills with blood
- Isovolumetric contraction: heart contracts but no blood is ejected
- Isovolumetric relaxation: heart relaxes, blood flows in
Cardiac Output
- Amount of blood pumped by each ventricle in 1 minute
- Cardiac Output (CO) = Heart Rate x Stroke Volume
- Example: HR = 70 beats/min, SV = 70 ml/beat, CO = 4.9 L/min
Cardiac Reserve
- Cardiac Output is variable
- Cardiac Reserve = maximal output (CO) – resting output (CO)
- Average individuals have a cardiac reserve of 4X or 5X CO
- Trained athletes may have a cardiac reserve of 7X CO
Regulation of Stroke Volume
- SV = EDV – ESV
- EDV: End Diastolic Volume, volume of blood in heart after it fills
- ESV: End Systolic Volume, volume of blood in heart after contraction
- Each beat ejects about 60% of blood in ventricle
- Preload, contractility, and afterload are the 3 most important factors in regulating SV
Regulation of Stroke Volume (continued)
- Preload: degree of stretching of cardiac muscle cells before contraction
- Contractility: increase in contractile strength separate from stretch and EDV
- Afterload: pressure that must be overcome for ventricles to eject blood from heart
Preload: Frank-Starling Law of the Heart
- Length-tension relationship of heart, where Length = EDV and Tension = SV
- Normally, muscle fibers are shorter than optimal length, increasing/decreasing fiber length increases/decreases force generation
Contractility
- The contractile strength at a given muscle length
- Sympathetic nervous stimulation opens Ca channels, increases contractility
- Positive inotropic effects: increase contractility, e.g., glucagon, thyroxin, epinephrine, digitalis
- Negative inotropic effects: reduce contractility, e.g., acidosis, high extracellular K, calcium channel blockers
Afterload
- If blood pressure is high, it is difficult for the heart to eject blood
- More blood remains in the chambers after each beat
- Heart has to work harder to eject blood, due to increased length/tension of cardiac muscle cells
Regulation of Heart Rate
- Normally, SV is constant
- Control of CO is exerted through changes in heart rate
- Intrinsic controls: Bainbridge effect, increase in EDV increases HR
- Extrinsic controls: autonomic nervous system, hormones, ions, body temperature, age/gender, body mass/blood volume, exercise, stress/illness
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.