Podcast
Questions and Answers
Which of the following accurately describes the anatomical location of the heart?
Which of the following accurately describes the anatomical location of the heart?
- Situated in the middle mediastinum, with approximately two-thirds of its mass to the left of the midline. (correct)
- Positioned deep to the vertebrae, extending from the level of the 5th to the 7th intercostal space.
- Located primarily in the right mediastinum, with the apex directed superiorly.
- Lying within the pleural cavity, anchored by the fibrous pericardium to the diaphragm.
How does the fibrous pericardium contribute to the hearts function and protection?
How does the fibrous pericardium contribute to the hearts function and protection?
- By providing a flexible covering that allows the heart to expand freely during exercise.
- By preventing overstretching of the heart and anchoring it within the mediastinum. (correct)
- By directly anchoring the heart to the diaphragm, preventing movement during respiration.
- By secreting serous fluid that lubricates the heart, preventing friction during contraction.
If a blockage occurred in the coronary sinus, which area would be most directly affected?
If a blockage occurred in the coronary sinus, which area would be most directly affected?
- The pumping of deoxygenated blood from the right ventricle to the pulmonary trunk.
- The distribution of oxygenated blood from the aorta to the systemic circulation.
- The drainage of deoxygenated blood from the heart muscle itself into the right atrium. (correct)
- The flow of oxygenated blood from the lungs to the left atrium.
What is the functional significance of the left ventricle having a thicker myocardial wall compared to the right ventricle?
What is the functional significance of the left ventricle having a thicker myocardial wall compared to the right ventricle?
Which sequence accurately describes the flow of blood from the superior and inferior vena cavae to the lungs?
Which sequence accurately describes the flow of blood from the superior and inferior vena cavae to the lungs?
What is the primary function of the chordae tendinae?
What is the primary function of the chordae tendinae?
Which of the following accurately describes the flow of blood in the pulmonary circuit?
Which of the following accurately describes the flow of blood in the pulmonary circuit?
During ventricular contraction, why does minimal blood flow occur through the coronary arteries?
During ventricular contraction, why does minimal blood flow occur through the coronary arteries?
Which valve prevents backflow of blood from the aorta into the left ventricle?
Which valve prevents backflow of blood from the aorta into the left ventricle?
Which of the following structures prevents overdistention of the right ventricle?
Which of the following structures prevents overdistention of the right ventricle?
Following the systemic circuit, where does oxygenated blood go after leaving the left ventricle?
Following the systemic circuit, where does oxygenated blood go after leaving the left ventricle?
Why is coronary circulation essential to the heart?
Why is coronary circulation essential to the heart?
The PR interval on an ECG tracing represents the time between what two events?
The PR interval on an ECG tracing represents the time between what two events?
Which wave on an ECG tracing represents ventricular repolarization?
Which wave on an ECG tracing represents ventricular repolarization?
What does the QRS complex represent in an ECG tracing?
What does the QRS complex represent in an ECG tracing?
Which of the following best describes the purpose of an electrocardiograph?
Which of the following best describes the purpose of an electrocardiograph?
An abnormally long QT interval may indicate an increased risk for what?
An abnormally long QT interval may indicate an increased risk for what?
What physiological event does the P wave on an ECG tracing represent?
What physiological event does the P wave on an ECG tracing represent?
What is the significance of the U wave in an ECG tracing, when present?
What is the significance of the U wave in an ECG tracing, when present?
In clinical practice, how are electrodes positioned on the body to record an ECG?
In clinical practice, how are electrodes positioned on the body to record an ECG?
What is the cardiac cycle?
What is the cardiac cycle?
What is the primary role of the coronary arteries during heart relaxation?
What is the primary role of the coronary arteries during heart relaxation?
Which component of the cardiac conduction system is known as the primary pacemaker of the heart?
Which component of the cardiac conduction system is known as the primary pacemaker of the heart?
Why is the slow conduction rate of the AV node crucial for proper heart function?
Why is the slow conduction rate of the AV node crucial for proper heart function?
The Bundle of His serves as the sole electrical connection between which two areas of the heart?
The Bundle of His serves as the sole electrical connection between which two areas of the heart?
Which of the following describes the sequence of the spread of action potentials in the heart, starting from the pacemaker?
Which of the following describes the sequence of the spread of action potentials in the heart, starting from the pacemaker?
If the SA node fails, which part of the cardiac conduction system would likely take over as a secondary pacemaker, and what would be its expected impulse rate?
If the SA node fails, which part of the cardiac conduction system would likely take over as a secondary pacemaker, and what would be its expected impulse rate?
What is the role of Purkinje fibers in ventricular contraction?
What is the role of Purkinje fibers in ventricular contraction?
A cardiologist observes that a patient's ventricles are contracting before the atria have fully contracted. Which part of the cardiac conduction system is MOST LIKELY malfunctioning?
A cardiologist observes that a patient's ventricles are contracting before the atria have fully contracted. Which part of the cardiac conduction system is MOST LIKELY malfunctioning?
Following ventricular contraction, what event must occur before the next action potential originates in the SA node?
Following ventricular contraction, what event must occur before the next action potential originates in the SA node?
Flashcards
Heart
Heart
A four-chambered, muscular organ located between the lungs, shaped like an inverted cone.
Apex of the Heart
Apex of the Heart
The pointed, inferior part of the heart, directed to the left.
Pericardium
Pericardium
A connective tissue sac that surrounds and protects the heart.
Right Atrium
Right Atrium
Signup and view all the flashcards
Ventricles
Ventricles
Signup and view all the flashcards
Interventricular Septum
Interventricular Septum
Signup and view all the flashcards
Atrioventricular (AV) Valves
Atrioventricular (AV) Valves
Signup and view all the flashcards
Tricuspid Valve
Tricuspid Valve
Signup and view all the flashcards
Bicuspid (Mitral) Valve
Bicuspid (Mitral) Valve
Signup and view all the flashcards
Semilunar Valves
Semilunar Valves
Signup and view all the flashcards
Pulmonary Circuit
Pulmonary Circuit
Signup and view all the flashcards
Systemic Circuit
Systemic Circuit
Signup and view all the flashcards
Coronary Artery Blood Flow
Coronary Artery Blood Flow
Signup and view all the flashcards
Cardiac Conduction System
Cardiac Conduction System
Signup and view all the flashcards
Sinoatrial (SA) Node
Sinoatrial (SA) Node
Signup and view all the flashcards
SA Node Location
SA Node Location
Signup and view all the flashcards
Atrioventricular (AV) Node
Atrioventricular (AV) Node
Signup and view all the flashcards
AV Node Delay Function
AV Node Delay Function
Signup and view all the flashcards
Atrioventricular (AV) Bundle
Atrioventricular (AV) Bundle
Signup and view all the flashcards
AV Bundle Function
AV Bundle Function
Signup and view all the flashcards
Purkinje Fibers
Purkinje Fibers
Signup and view all the flashcards
Electrocardiogram (ECG/EKG)
Electrocardiogram (ECG/EKG)
Signup and view all the flashcards
P Wave
P Wave
Signup and view all the flashcards
QRS Complex
QRS Complex
Signup and view all the flashcards
T Wave
T Wave
Signup and view all the flashcards
U Wave
U Wave
Signup and view all the flashcards
PR Interval
PR Interval
Signup and view all the flashcards
QT Interval
QT Interval
Signup and view all the flashcards
Cardiac Cycle
Cardiac Cycle
Signup and view all the flashcards
ECG Electrode Placement
ECG Electrode Placement
Signup and view all the flashcards
Study Notes
- Author: Julius John DP. Salamanes
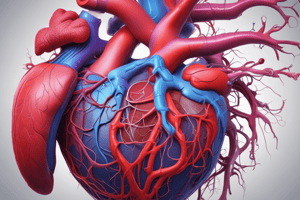
The Heart
- A four-chambered hollow muscular organ located between the lungs, shaped like a blunt inverted cone.
- The apex directed inferiorly and to the left, located at the 5th intercostal space, midclavicular line.
- The base directed posteriorly, superiorly, and to the right.
- The heart extends to the level of the 2nd intercostal space and is located deep to the sternum.
- It resides in the middle mediastinum.
- Approximately two-thirds of the heart's mass lies to the left of the midline.
- The heart's size approximates a fist.
- The weight for males is 250-390 gm.
- The weigh for females is 200-275 gm.
- The pericardial cavity contains the heart.
- Pericardial cavity is formed by the pericardium, or pericardial sac
- The pericardium is a connective tissue covering that protects the heart.
- The fibrous pericardium prevents overstretching and anchors the heart in the mediastinum.
- The serous pericardium consists of:
- Parietal pericardium
- Visceral pericardium
Heart Chambers
- Two superior chambers receive blood from veins.
- The right atrium receives deoxygenated blood from the superior vena cava, inferior vena cava, and coronary sinus.
- The left atrium receives oxygenated blood through pulmonary veins.
- Interatrial septum partitions the two atria.
- Two inferior chambers are the heart's major pumping chambers.
- The ventricles eject blood into the arteries to flow through the circulatory system.
- The right ventricle pumps blood into the pulmonary trunk.
- The left ventricle pumps blood into the aorta.
- The interventricular septum is the partition between ventricles.
Valves of the Heart
- The atrioventricular (AV) valves are between the atrium and ventricle.
- The tricuspid valve is between the right atrium and right ventricle.
- The bicuspid (mitral) valve is between the left atrium and left ventricle.
- The semilunar valves are between the ventricle and an artery.
- The pulmonic valve is between the right ventricle and pulmonary trunk.
- The aortic valve is between the left ventricle and aorta.
Structures within the ventricles
- Chordae tendinae are tendon-like cords attached to the valves' cusps.
- Papillary muscles are cone-shaped muscular pillars attached to the chordae tendinae.
- Trabeculae carnae are coarse cardio muscle fiber ridges along the cardiac wall.
- Moderator band is a specialized muscle column at the septal wall which prevents overdistention of the right ventricle.
Blood Flow Through The Heart
- Blood flow to the lungs:
- Begins with the superior vena cava and the inferior vena cava.
- then blood flows through the right atrium and the tricuspid valve.
- Next blood flows through the right ventricle and the pulmonary valve.
- Blood flow in the lungs:
- Starts with the pulmonary artery and through the lungs.
- Returns via the pulmonary veins and flows through the left atrium.
- Flows through the mitral valve, then the left ventricle.
- Blood leaves the heart via the Aorta.
Types of Circulation
-
Pulmonary circuit (or circulation): -unoxygenated blood moves from the right ventricle to the respiratory (alveolar) surfaces of the lungs.
- oxygenated blood returns to the left atrium via the pulmonary veins.
- the right side of the heart pumps blood to the lungs and brings it back to the left side. Blood moves from the superior and inferior vena cavas to the lungs and then back to the left atrium.
-
Systemic circuit (or circulation):
- oxygenated blood is carried from the left ventricle to all parts of the body.
- All parts with the exception of the lungs, unoxygenated blood, returns to the right atrium.
- Left side of the heart pumps blood to tissues and back to the right.
- Blood moves from the left ventricle to the body and back to the superior and inferior vena cavas to the right atrium.
Coronary Circulation
- The myocardium has its own network of blood vessels, the coronary or cardiac circulation.
- The coronary arteries branch from the ascending aorta.
- Coronary arteries encircle the heart.
- Nutrients from blood within the heart chambers are not able to diffuse quickly enough.
- Little blood flows into the coronary arteries when the heart is contracting because they are squeezed shout.
- When the heart relaxes, the high pressure drives blood through the coronary arteries, into capillaries, and then into coronary veins.
The Cardiac Conduction System
- It is formed by specialized cardiac muscle cells in the heart wall
- It coordinates the atrial & ventricular contractions.
- Includes the follow key elements:
- Sinoatrial (SA) node
- Atrioventricular (AV) node
- Atrioventricular bundles (AV bundles) or Bundle of His
- Purkinje fibers
Sinoatrial (SA) node
- The primary pacemaker of the heart.
- Sets the rhythm of electrical excitation, causing the heart to contract.
- Found in the superior wall of the right atrium.
- It's located just inferior and lateral to the opening of the superior vena cava.
- Generates 60 to 100 impulses per minute.
- Action potentials originate at the SA node and spread over the right and left atria, causing them to contract.
Atrioventricular (AV) node
- It is strategically located in the lower part of the right atrium.
- Located just above the attachment of the septal cusp of the tricuspid valve.
- The slow rate of action potential enables the atria to complete contraction before potentials are delivered to ventricles.
- Coordinates incoming electrical impulses from the atria.
- After a light delay, relays impulse onward to ventricles.
- It generates 40-60 impulses per minute.
Atrioventricular (AV) bundle
- Also called the Bundle of His
- Bundles of conducting fibers in the interventricular system which runs a short distance and then divides.
- Right bundle branch
- Left bundle branch
- The only pathway that connects the myocardium of the atria to the myocardium of the ventricles electrically.
- Only route for transmission of impulse from atria into the ventricles.
Purkinje fibers
- Terminal point in the conduction system.
- Composed of Purkinje cells, which rapidly conduct impulses.
- Originates in the apex of the heart upward.
- Myocardial cells are stimulated which results in ventricular contraction
- 30-40 impulses per minute.
- After ventricular contraction, the ventricles relax.
- Once the Ventricles have completely relaxed, another action potential originates in the SA node, beginning the next cycle of contractions.
Electrocardiogram (ECG or EKG)
- It's a composite record of action potentials produced by all heart muscle fibers during each heartbeat.
- As action potentials propagate, they generates electrical currents.
- Electrical currents are detected at the surface of the body and recorded by a machine called electrocardiograph.
- During clinical practice, electrodes are placed on the arms and legs.
- Also, are placed at six positions on the chest to capture leads to record the ECG.
- The electrocardiograph amplifies the heart's electrical signals, producing 12 different tracings from different combinations of limb and chest leads.
Normal ECG tracing
P Wave
- Represents atrial depolarization (contraction) from the SA node through contractile fibers in both atria.
- Appears as a small upward deflection.
QRS complex:
- Represents rapid ventricular depolarization.
- Spread of action potential through ventricular contractile fibers.
- Includes a: --Q wave which presents a downward deflection --R wave, which constitutes a large upright, and triangular trace --S wave presents a downward wave
T wave:
- Represents ventricular repolarization or ventricular relaxation.
- Occurs as the ventricles are starting to relax
- Dome-shaped upward deflection.
- Smaller and wider than the QRS complex.
- Repolarization occurs slowly.
U Wave:
- Not part of the three clearly recognizable waves in ECG
- Represents late ventricular repolarization.
Intervals or segments in ECG analysis
PR interval
- The time between the beginning of the P wave and the beginning of the QRS complex.
- represents the time from atrial depolarization to the beginning of ventricular depolarization.
QT interval
- The period extending from the beginning of the QRS complex to the end of the T wave.
- Represents the time from the beginning of ventricular depolarization to the end of ventricular repolarization.
- Can be lengthened by myocardial damage, myocardial ischemia, or conduction abnormalities.
Cardiac cycle
- A repetitive pumping process that starts at one contraction.
- Concludes at the start of the next contraction.
- It includes all events associated with one heartbeat.
- Alternating contraction and relaxation of atria and ventricles
- Blood is forced from areas of higher pressure to lower pressure.
Systole (contraction)
- Refers to the phase of contraction either atrial or ventricular
- Follows depolarization --Atrial systole which consists of contraction in the two atria. --Ventricular systole which consists of contraction in the two ventricles.
Diastole (relaxation)
- Phase of dilatation following repolarization --Atrial diastole is relaxation of the two atria. --Ventricular diastole is relaxation of the two ventricles.
Pressure and Volume changes during the Cardiac cycle.
- In each cardiac cycle, atria and ventricles contract and relax alternately.
- Forces blood from areas of higher pressure to areas of lower pressure.
- As chamber of the heart contracts, blood pressure within it increases.
- Each ventricle ejects the same blood volume per each beat.
- The same pattern exists for each pumping chamber.
- When the heart rate is 75 beats/min, a cardiac cycle lasts 0.8 seconds.
- During ventricular contraction and relaxation, the semilunar valves open, and the atrioventricular valves close.
- During ventricle relaxation and atrial contraction, the atrioventricular valves open and the semilunar valves close.
Cardiac output (CO)
- It is the volume of blood pumped by either ventricle into the aorta (or pulmonary trunk) each minute.
- Calculated by multiplying stroke volume and heart rate.
- Stoke volume (SV)- the volume of blood pumped by the ventricle during each contraction
- Heart rate (HR)- the number of heartbeats per minute
- Formula: Cardiac output (CO) = Stroke volume (SV) x Heart rate (HR)
- Under resting conditions, the heart rate is approximately 72 beats/min,.
- Stroke volume is approximately 70 ml/beat.
- Consequently, the cardiac output slightly more than 5L/min.
- CO= SV x HR
- = 70 ml/beat x 72 beats/min = 5040 ml/min (approx 5L/min)
Control mechanisms that modify the stroke volume and heart rate
- Intrinsic Regulation of the Heart
- Extrinsic Regulation of the Heart
- Nervous regulation
- Chemical regulation
- Intrinsic Regulation of the Heart: the mechanisms contained within the heart itself
- The amount of blood in the ventricles determines the degree the cardiac muscle fibers are stretched. At the end of ventricular diastole.
- Venous return is the amount of that returns to the heart.
- Preload- the degree to which the ventricular walls are stretched at the end of diastole;
- The amount of blood that fills the ventricles during ventricular relaxation.
- Afterload represents the pressure that is withstood by the ventricles as they're used to pump blood from.
- "Starling's Law of the Heart": the venous return should decrease and affect the preload stroke, and the cardiac output as well
Extrinsic Regulation of the Heart
- Refers to the mechanisms external to the heart.
- Either with nervous or chemical regulation.
- Nervous Regulation consists of the Baroreceptor Reflex.
- Autonomic nervous system carries nervous influences.
- Sympathetic and parasympathetic nerve fibers innervate the heart.
- Stimulation by sympathetic nerve fibers causes heart rate and stroke volume to increase.
- Stimulation by parasympathetic nerve fibers causes a decrease in heart rate.
Baroreceptors
- Stretch sensors that monitor blood pressure
- located in the aorta and in the wall of the internal carotid arteries.
- A chemical regulation of cardiac reflexes is referred to as "chemoreceptor reflex"
- Hormones, Like Epinephrine small amounts of norepinephrine released from the adrenal medulla are are released in response during an excercise emotional excitment.
- Epinephrine and norepinephrine bind to receptor proteins on cardiac muscle causing an increase in heart rate and stroke volume.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.