Podcast
Questions and Answers
What are the functions of the ankle and foot? (Select all that apply)
What are the functions of the ankle and foot? (Select all that apply)
- Absorb stress and shock (correct)
- Play a role in absorbing heat
- Facilitate side-to-side movement only
- Provide a stable base of support in weight-bearing postures (correct)
How many bones are found in the foot?
How many bones are found in the foot?
26 bones & 2 sesamoid bones
The MCL (Deltoid ligament) controls lateral distraction forces on the ankle.
The MCL (Deltoid ligament) controls lateral distraction forces on the ankle.
False (B)
Ankle sprain involves stretching or tearing of ligaments in the __________.
Ankle sprain involves stretching or tearing of ligaments in the __________.
What is the purpose of the Anterior Drawer Test?
What is the purpose of the Anterior Drawer Test?
What is the purpose of the Talar Tilt Test?
What is the purpose of the Talar Tilt Test?
What is the purpose of the Squeeze Test?
What is the purpose of the Squeeze Test?
When performing the Anterior Drawer Test, the foot should be placed in which position?
When performing the Anterior Drawer Test, the foot should be placed in which position?
The Talar Tilt Test is used to diagnose syndesmotic injury.
The Talar Tilt Test is used to diagnose syndesmotic injury.
Define muscle spasm.
Define muscle spasm.
What are some factors that can contribute to muscle spasm?
What are some factors that can contribute to muscle spasm?
Muscle cramps are painful, intense, and sustained muscle contractions.
Muscle cramps are painful, intense, and sustained muscle contractions.
The primary cause of pain in muscle spasm is ____, which leads to the release of substances causing pain.
The primary cause of pain in muscle spasm is ____, which leads to the release of substances causing pain.
Match the following modalities with their rehabilitation use:
Match the following modalities with their rehabilitation use:
What is the neurotransmitter for skeletal muscles?
What is the neurotransmitter for skeletal muscles?
What is the receptor type found on skeletal muscle fibers?
What is the receptor type found on skeletal muscle fibers?
ATP is initially used for muscle contraction, and then ATP is generated by the muscle cell primarily from ________.
ATP is initially used for muscle contraction, and then ATP is generated by the muscle cell primarily from ________.
Low level laser therapy is known to disrupt the cycle at trigger points.
Low level laser therapy is known to disrupt the cycle at trigger points.
What are the characteristics of latent MTPS?
What are the characteristics of latent MTPS?
What are the characteristics of active MTPS?
What are the characteristics of active MTPS?
According to Simon and Travell, what are the three characteristics of MTPS?
According to Simon and Travell, what are the three characteristics of MTPS?
In MTPS, the abnormal release of acetylcholine can lead to taut band formation.
In MTPS, the abnormal release of acetylcholine can lead to taut band formation.
Diagnosis of MTPS is often confirmed through physical examination findings such as ___, ___, and ___
Diagnosis of MTPS is often confirmed through physical examination findings such as ___, ___, and ___
What are absolute contraindications for trigger point dry needling?
What are absolute contraindications for trigger point dry needling?
What are relative contraindications for trigger point dry needling?
What are relative contraindications for trigger point dry needling?
What is the recommended frequency range for ultrasound in trigger point injections?
What is the recommended frequency range for ultrasound in trigger point injections?
A latent trigger point causes spontaneous pain.
A latent trigger point causes spontaneous pain.
______ can bind to troponin, leading to the movement of tropomyosin and actin-myosin attachment.
______ can bind to troponin, leading to the movement of tropomyosin and actin-myosin attachment.
Study Notes
Ankle Sprain
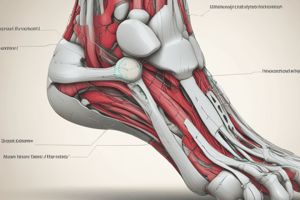
Functions of Ankle and Foot
- Stability: provide a stable base of support in various weight-bearing postures and act as a rigid lever for effective push-off during gait
- Mobility: absorb stress and shock, and propel the body during walking
- Protection: provide sensation to the sole of the foot
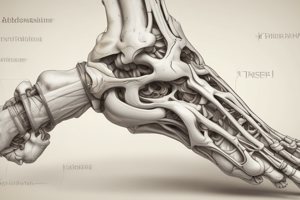
Bones
- 26 bones and 2 sesamoid bones divided into 3 functional segments:
- Forefoot (anterior): 5 metatarsals, 14 phalanges
- Midfoot (middle): navicular, cuboid, 3 cuneiform bones
- Hindfoot (posterior): talus, calcaneus
Joints
- 25 component joints, including:
- Proximal and distal tibiofibular joints
- Ankle (talo-crural) joint
- Talo-calcaneal (subtalar) joint
- Talo-navicular joint
- Calcaneo-cuboidal joint
- Transverse tarsal joint
- 5 tarso-metatarsal joints
- 5 metatarso-phalangeal joints
- 9 interphalangeal joints
Ligaments
- Medial collateral ligament (MCL):
- Also known as deltoid ligament
- Fan-shaped
- Superficial and deep fibers from the borders of the tibial malleolus to the navicular, talus, and calcaneus
- Extremely strong
- Controls medial distraction forces on the ankle
- Lateral collateral ligament (LCL):
- Composed of 3 separate bands: anterior talofibular ligament, posterior talofibular ligament, and calcaneofibular ligament
- Weaker and more susceptible to injury than MCL
- Controls varus (lateral distraction) forces
Definitions of Motion
- Axis: through the fibular malleolus, body of the talus, and just below or through the tibial malleolus
- Tibial torsion: more posterior position of the fibular malleolus due to normal torsion or twist in the distal tibia in relation to the proximal tibia
Ankle Sprain
- Involves stretching or tearing of ankle ligaments
- 85% of ankle sprains occur on the lateral aspect, involving the anterior talofibular ligament (ATFL) and calcaneofibular ligament (CFL)
- 5-10% of ankle sprains are syndesmotic or high ankle sprains, involving the tear of the anterior distal tibiofibular ligament
- 5% of ankle sprains occur on the medial aspect, involving the deltoid ligament
Epidemiology
- Ankle sprains are a common cause of morbidity in the general population and athletes
- Peak incidence occurs between 15-24 years of age
- Males are more commonly affected than females (incidence ratio 1.04)
- However, a recent meta-analysis showed that females have a higher incidence rate than males (13.6 vs 6.94 per 1000 exposures)
Mechanism of Injury
- Strains occur depending on the mechanism of injury
- Stress supination and inversion of the foot (most common) → tear of the lateral ankle structures (ATFL)
- Stress eversion of the foot → tear of the medial ankle structures (deltoid ligament)
- Stress dorsiflexion and external rotation of the foot → syndesmotic injury
Grading
- Grade I: partial tear of the ATFL, CFL, and posterior talofibular ligament (PTFL) intact
- Grade II: complete tear of the ATFL, partial tear of the CFL, and PTFL intact
- Grade III: complete tear of the ATFL, CFL, and PTFL
Functional Limitations
- Patients may experience difficulty walking due to pain and swelling
- Proprioception and balance on the injured ankle may be impaired
- Athletes may have difficulty returning to play until the swelling and pain have subsided, and rehabilitation is almost complete
Symptoms
- Patients report pain, swelling, and tenderness on the injured ligament
- Some patients may report a "pop" sensation at the time of injury
- Difficulty weight-bearing on the injured ankle during ambulation
- Ecchymosis may occur within 24-48 hours
Physical Examination
- Look: edema and ecchymosis around the ankle
- Feel: palpate the ATFL, CFL, and deltoid ligament
- Move: assess range of motion (ROM) of the ankle joint
Special Tests
- Anterior Drawer Test: assesses the integrity of the ATFL
- Talar Tilt Test: assesses the integrity of the CFL and deltoid ligament
- Squeeze Test: diagnoses syndesmotic injury
Imaging
- X-ray: assesses for fractures and osteochondral lesions
- MRI: assesses soft tissue injuries and osteochondral lesions
- Ultrasound: assesses soft tissue injuries and subluxation of tendons
Diagnosis
- Differential diagnosis: fracture, osteochondral lesion, syndesmotic injury, and tendon subluxation
Treatment
- Conservative management: rehabilitation, bracing, and protection
- Surgical management: may be necessary for grade III ankle sprains or those with osteochondral lesions
Rehabilitation Protocol
- Phase 1 (acute): 3-5 days, aims to protect the injured tissue, reduce pain and inflammation, and maintain functional range of motion
- Phase 2 (subacute): 5-10 days, aims to improve strength, proprioception, and functional range of motion
- Phase 3 (maturation): 10-14 days, aims to improve strength, power, and functional range of motion### Ankle Sprain Protocol
- The ankle sprain protocol consists of three phases: acute, subacute, and mature phases.
- During the acute phase, the goal is to reduce pain and inflammation, and to prevent further injury.
- In the subacute phase, the goal is to improve range of motion (ROM), strength, and proprioception.
- In the mature phase, the goal is to restore functional ability and prevent re-injury.
Acute Phase
- Lasts 0-3 days after injury
- Goals:
- Reduce pain and inflammation
- Prevent further injury
- Restore ROM and strength
- Techniques:
- Pulsed ultrasound to reduce pain and inflammation
- Electric stimulation to minimize pain and muscle spasm
- Cryotherapy to reduce pain and inflammation
- Latihan ROM and strengthening exercises to improve ROM and strength
- Technique of "flushing-type" massage to increase blood circulation
Subacute Phase
- Lasts 3-6 weeks after injury
- Goals:
- Improve ROM and strength
- Increase proprioception and balance
- Prevent re-injury
- Techniques:
- Continue latihan ROM and strengthening exercises
- Add dynamic proprioception exercises with perturbation
- Use taping or bracing for additional support
- Stretching exercises to improve ROM
Mature Phase
- Lasts 6 weeks or more after injury
- Goals:
- Restore functional ability
- Prevent re-injury
- Improve proprioception and balance
- Techniques:
- Plyometric exercises to improve power and explosiveness
- Dynamic proprioception exercises with perturbation
- Aggressive stretching exercises to improve ROM
- Combine soft tissue techniques, such as cross-fiber massage and myofascial release
Criteria for Return to Activity
- Pain-free during activity
- No swelling
- Full ROM
- Full strength and endurance
- Normal proprioception and balance
- Patient feels psychologically ready
Muscle Spasm
- Definition: Involuntary muscle contraction that is painful and can be tender to the touch
- Causes:
- Overuse or fatigue
- Muscle imbalance or poor posture
- Dehydration or electrolyte imbalance
- Medical conditions, such as multiple sclerosis
- Medications, such as diuretics, statins, or beta-agonists
- Symptoms:
- Pain or stiffness
- Muscle weakness or fatigue
- Cramping or twitching
- Numbness or tingling
- Treatment:
- Stretching and strengthening exercises
- Modalities, such as heat or cold therapy
- Medications, such as muscle relaxants or pain relievers
- Manual therapy, such as massage or trigger point therapy
Myofascial Trigger Point Syndrome
- Definition: A condition characterized by pain and stiffness in a specific area of the muscle
- Causes:
- Muscle injury or overuse
- Poor posture or biomechanics
- Stress or anxiety
- Hormonal changes
- Symptoms:
- Pain or stiffness
- Limited range of motion
- Weakness or fatigue
- Numbness or tingling
- Treatment:
- Trigger point therapy
- Stretching and strengthening exercises
- Modalities, such as heat or cold therapy
- Manual therapy, such as massage or joint mobilization### Myofascial Trigger Point Syndrome (MTPS)
- MTPS is a condition of muscle pain or fascia, which can be acute or chronic, involving sensory, motor, or autonomic functions related to trigger points.
- Diagnosis is based on anamnesis and physical examination.
- Anamnesis typically includes complaints of pain, tenderness, and limited range of motion.
- Physical examination includes inspection, palpation, and identification of trigger points and taut bands.
Pathophysiology
- Three key features of MTPS:
- Release of acetylcholine, which leads to muscle contraction and pain.
- Shortening of sarcomeres, which increases muscle tension.
- Release of sensitizing substances, which causes pain.
- These features interact in a positive feedback cycle, leading to increased pain and muscle tension.
Vicious Cycle
- Abnormal release of acetylcholine leads to increased muscle tension and pain.
- Increased muscle tension and pain lead to the release of sensitizing substances, which further increases pain.
- Pain leads to muscle contraction, which leads to the release of acetylcholine, and so on.
Diagnosis
- Diagnosis is based on five major criteria and at least one minor criterion.
- Major criteria include:
- Trigger point
- Taut band
- Pain on palpation
- Referred pain
- Limited range of motion
- Minor criteria include:
- Autonomic dysfunction
- Muscle weakness
Treatment
- Manual therapy:
- Stretching with intermittent cold
- Deep pressure massage
- Trigger point release
- Modalities:
- Ultrasound
- Transcutaneous electrical nerve stimulation (TENS)
- Low-level laser therapy (LLLT)
- Radial shockwave therapy
- Dry needling: a technique that uses a thin needle to stimulate trigger points, muscles, and connective tissue.
Dry Needling
- Indications: MTPS that is not responsive to conservative treatment.
- Contraindications:
- Absolute: patient has a bleeding disorder, is taking anticoagulant medication, or has a fear of needles.
- Relative: patient has a compromised immune system, is pregnant, or has a psychological disorder.
Injections
- Injections can be used to treat MTPS that is not responsive to conservative treatment.
- Types of injections:
- Local anesthetics (e.g., lidocaine, procaine)
- Corticosteroids
- Other substances (e.g., botulinum toxin)
Physical Examination
- Posture evaluation
- Measurement of range of motion
- Muscle strength testing
- Palpation:
- Identification of trigger points and taut bands
- Assessment of muscle tenderness and pain
Spray and Stretch
- A technique that uses a vapocoolant spray to anesthetize the skin and allow for deeper stretching.
- Steps:
- Identify the muscle with the trigger point
- Position the patient in a comfortable position
- Spray the vapocoolant at a 45-degree angle, moving the can 10 cm/sec
- Stretch the muscle while the patient is relaxed
Referred Pain
- Pain felt at a distance from the actual trigger point
- Examples:
- Pain in the shoulder blade that originates from a trigger point in the neck
- Pain in the leg that originates from a trigger point in the lower back
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Learn about the functions of ankle and foot, including stability, mobility, and protection, and explore the bones that make up this complex system.