Podcast
Questions and Answers
What could be a likely reason for a delayed allergic reaction after eating mammalian meats?
What could be a likely reason for a delayed allergic reaction after eating mammalian meats?
- Cross-reactivity with seafood
- Immediate hypersensitivity to poultry
- Prior exposure to shellfish
- Alpha-gal syndrome (correct)
Which factor is NOT considered a risk factor for anaphylaxis during anesthesia?
Which factor is NOT considered a risk factor for anaphylaxis during anesthesia?
- Vegetarian diet (correct)
- Female sex
- History of eczema
- Previous anaphylaxis
What are the three components of the triad indicating anaphylaxis under anesthesia?
What are the three components of the triad indicating anaphylaxis under anesthesia?
- HoTN, Tachycardia, Bronchospasm (correct)
- HoTN, Bronchospasm, Skin rash
- Cyanosis, Respiratory distress, Hypoglycemia
- Tachycardia, Hyperthermia, Bronchospasm
When should patients experiencing suspected anaphylaxis be evaluated?
When should patients experiencing suspected anaphylaxis be evaluated?
Which of the following is a common severe reaction that can occur with anaphylaxis under anesthesia?
Which of the following is a common severe reaction that can occur with anaphylaxis under anesthesia?
What should be included in the detailed description of an anaphylaxis event for evaluation?
What should be included in the detailed description of an anaphylaxis event for evaluation?
What is a common consequence of an allergic reaction to protamine administration?
What is a common consequence of an allergic reaction to protamine administration?
What should be monitored immediately after an anaphylaxis event?
What should be monitored immediately after an anaphylaxis event?
What is the primary mechanism through which Type I (IgE) mediated allergic reactions occur?
What is the primary mechanism through which Type I (IgE) mediated allergic reactions occur?
Which pathway of complement activation does not require the presence of antibodies?
Which pathway of complement activation does not require the presence of antibodies?
Which neuromuscular blocker is most commonly associated with anaphylaxis?
Which neuromuscular blocker is most commonly associated with anaphylaxis?
What is the reported incidence of anaphylaxis for Sugammadex?
What is the reported incidence of anaphylaxis for Sugammadex?
What percentage of perioperative allergic reactions are attributed to latex?
What percentage of perioperative allergic reactions are attributed to latex?
Which antibiotic is responsible for the majority of allergic reactions in the general population?
Which antibiotic is responsible for the majority of allergic reactions in the general population?
Which of the following is a common hypothesis regarding 'Latex fruit syndrome'?
Which of the following is a common hypothesis regarding 'Latex fruit syndrome'?
Which agent is known to cause histamine release but is not necessarily considered to cause anaphylaxis?
Which agent is known to cause histamine release but is not necessarily considered to cause anaphylaxis?
What is one potential reaction when vancomycin is infused too quickly?
What is one potential reaction when vancomycin is infused too quickly?
Anaphylaxis due to animal-derived products is often attributed to which carbohydrate?
Anaphylaxis due to animal-derived products is often attributed to which carbohydrate?
Which of the following may be used cautiously if a patient has a history of penicillin allergy?
Which of the following may be used cautiously if a patient has a history of penicillin allergy?
What should be done if there is a documented latex allergy in a patient prior to surgery?
What should be done if there is a documented latex allergy in a patient prior to surgery?
What is a rare but possible reaction from opioids administered intravenously?
What is a rare but possible reaction from opioids administered intravenously?
What are the potential reactions linked to alpha-gal syndrome after eating mammalian meats?
What are the potential reactions linked to alpha-gal syndrome after eating mammalian meats?
Which of the following is a risk factor for anaphylaxis during anesthesia?
Which of the following is a risk factor for anaphylaxis during anesthesia?
In a patient under anesthesia, which triad of symptoms is most indicative of anaphylaxis?
In a patient under anesthesia, which triad of symptoms is most indicative of anaphylaxis?
Which component should be recorded in detail when evaluating an anaphylactic event?
Which component should be recorded in detail when evaluating an anaphylactic event?
What is a significant indicator of anaphylaxis severity during anesthesia?
What is a significant indicator of anaphylaxis severity during anesthesia?
Which of the following conditions may contribute to an increased risk of anaphylaxis?
Which of the following conditions may contribute to an increased risk of anaphylaxis?
What factor differentiates anaphylactic reactions from other allergic responses under anesthesia?
What factor differentiates anaphylactic reactions from other allergic responses under anesthesia?
When should serum tryptase levels be checked for effective evaluation of anaphylaxis?
When should serum tryptase levels be checked for effective evaluation of anaphylaxis?
Which of the following mechanisms is responsible for the degranulation of mast cells during a Type I allergic reaction?
Which of the following mechanisms is responsible for the degranulation of mast cells during a Type I allergic reaction?
What is the primary agent responsible for the majority of allergic reactions in the general population?
What is the primary agent responsible for the majority of allergic reactions in the general population?
Following the administration of Sugammadex, how quickly can anaphylaxis occur?
Following the administration of Sugammadex, how quickly can anaphylaxis occur?
What is the most common cause of perioperative allergic reactions attributed to latex?
What is the most common cause of perioperative allergic reactions attributed to latex?
In terms of allergic reactions in an anesthesia setting, what is a significant characteristic of NMBAs?
In terms of allergic reactions in an anesthesia setting, what is a significant characteristic of NMBAs?
Which of the following pathways can activate complement without antibodies?
Which of the following pathways can activate complement without antibodies?
What is a characteristic of the histamine release caused by Atracurium?
What is a characteristic of the histamine release caused by Atracurium?
If a patient has a known allergy to Penicillin, which medication should be avoided?
If a patient has a known allergy to Penicillin, which medication should be avoided?
What is a potential consequence of rapidly infused Vancomycin?
What is a potential consequence of rapidly infused Vancomycin?
Which best describes the incidence of anaphylaxis with Propofol?
Which best describes the incidence of anaphylaxis with Propofol?
In the context of Alpha-Gal syndrome, which of the following agents could be a trigger?
In the context of Alpha-Gal syndrome, which of the following agents could be a trigger?
What should be prioritized if a patient with a known latex allergy is scheduled for surgery?
What should be prioritized if a patient with a known latex allergy is scheduled for surgery?
Which of the following statements regarding NMBAs and anaphylaxis is true?
Which of the following statements regarding NMBAs and anaphylaxis is true?
What specific symptom triad is indicative of anaphylaxis under anesthesia?
What specific symptom triad is indicative of anaphylaxis under anesthesia?
Which group of patients has an increased risk of experiencing anaphylaxis during anesthesia?
Which group of patients has an increased risk of experiencing anaphylaxis during anesthesia?
When evaluating a patient for suspected anaphylaxis, which detail is least relevant?
When evaluating a patient for suspected anaphylaxis, which detail is least relevant?
After an anaphylactic event, when should serum tryptase levels be measured for effective analysis?
After an anaphylactic event, when should serum tryptase levels be measured for effective analysis?
Which of the following factors is NOT associated with increased risk for anaphylaxis?
Which of the following factors is NOT associated with increased risk for anaphylaxis?
What type of allergic reaction is most commonly linked to alpha-gal syndrome?
What type of allergic reaction is most commonly linked to alpha-gal syndrome?
Which of the following conditions can increase the likelihood of an allergic reaction to protamine administration?
Which of the following conditions can increase the likelihood of an allergic reaction to protamine administration?
What aspect of anaphylaxis presentation is specifically noted to differ when patients are under anesthesia?
What aspect of anaphylaxis presentation is specifically noted to differ when patients are under anesthesia?
What is the most common mechanism leading to vasodilation during a Type I (IgE) allergic reaction?
What is the most common mechanism leading to vasodilation during a Type I (IgE) allergic reaction?
What percentage of allergic reactions under anesthesia are attributed to neuromuscular blockers?
What percentage of allergic reactions under anesthesia are attributed to neuromuscular blockers?
Which type of hypersensitivity reaction accounts for 60% of allergic reactions associated with anesthesia?
Which type of hypersensitivity reaction accounts for 60% of allergic reactions associated with anesthesia?
What action should be taken if a patient has a documented allergy to latex?
What action should be taken if a patient has a documented allergy to latex?
What is the primary reason for the cross-reactivity seen with penicillin and some cephalosporins?
What is the primary reason for the cross-reactivity seen with penicillin and some cephalosporins?
Which of the following best describes the timing of anaphylaxis after administration of Sugammadex?
Which of the following best describes the timing of anaphylaxis after administration of Sugammadex?
Which of the following agents is known to cause histamine release but not necessarily anaphylaxis?
Which of the following agents is known to cause histamine release but not necessarily anaphylaxis?
What is a common consequence of anaphylaxis associated with propofol administration?
What is a common consequence of anaphylaxis associated with propofol administration?
Which condition is a significant trigger for anaphylaxis related to animal-derived products?
Which condition is a significant trigger for anaphylaxis related to animal-derived products?
What is the potential risk of rapidly infused vancomycin?
What is the potential risk of rapidly infused vancomycin?
Under what condition might a patient experience significant allergic reactions to iodine?
Under what condition might a patient experience significant allergic reactions to iodine?
What characteristic of alpha-gal syndrome contributes to anaphylactic reactions?
What characteristic of alpha-gal syndrome contributes to anaphylactic reactions?
Which of the following agents is least likely to cause severe allergic reactions during an anesthesia setting?
Which of the following agents is least likely to cause severe allergic reactions during an anesthesia setting?
Which response describes the activation pathways of the complement system?
Which response describes the activation pathways of the complement system?
What complication may arise from the administration of gelatin during anesthesia?
What complication may arise from the administration of gelatin during anesthesia?
Flashcards are hidden until you start studying
Study Notes
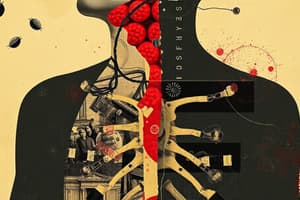
Anaphylaxis in Anesthesia Overview
- Anaphylaxis is a severe, potentially fatal allergic reaction that can occur during anesthesia.
- Common triggers include antibiotics, neuromuscular blockers (NMBs), latex, chlorhexidine (CHG), and blood products.
Most Common Culprits
- Antibiotics are the leading cause of anaphylaxis in the US.
- Neuromuscular blockers are the second most common in the US, but the primary cause in the UK.
- Other significant allergens include latex, CHG, and blood products.
Types of Allergic Reactions
- Type I (IgE Mediated) Reactions: Primary type of anaphylactic reaction, occurring in 60% of cases.
- Antigens stimulate mast cells and basophils, causing degranulation and release of mediators like histamine, leading to vasodilation and bronchoconstriction.
- Initial localized reactions can escalate quickly as allergens spread through the bloodstream.
Pathophysiology
- Anaphylaxis is marked by complement activation, a reaction cascade that can occur with or without antibodies.
- Three pathways exist: Classical, MB-Lectin, and Alternative, all leading to the release of potent mediators and immune response activation.
Neuromuscular Blockers (NMBAs)
- NMBAs account for 50-70% of allergic reactions during anesthesia.
- Succinylcholine and rocuronium are common culprits; sensitization from first exposure often leads to anaphylaxis upon re-exposure.
- Sugammadex can reverse anaphylaxis by binding rocuronium.
Antibiotics
- Penicillin and its derivatives are responsible for about 70% of allergic reactions in the general population.
- 8-10% cross-reactivity observed with cephalosporins in penicillin-allergic patients; avoid if anaphylaxis occurred from penicillin.
- Vancomycin should be administered slowly to prevent "Red Man Syndrome," characterized by flushing and hypotension.
Latex
- Approximately 20% of perioperative allergies result from latex exposure.
- "Latex fruit syndrome" relates to allergies involving fruits like bananas and avocados.
- Establish latex-free environments for patients with a known latex allergy.
Skin Prep and Contrast Dye
- Iodine and chlorhexidine may trigger allergy responses.
- Radiologic contrast dyes can also be anaphylactic triggers used during surgical procedures.
Opioids
- Commonly cause flushing and urticaria; life-threatening reactions are rare.
- Morphine and meperidine may cause histamine release leading to reactions, including hypotension.
Fluids and Other Agents
- Blood products and colloids can also cause anaphylaxis.
- Specific agents like radiocontrast dye, NSAIDs, insulin, and local anesthetics are potential allergens.
Alpha-Gal Syndrome
- An allergy to the carbohydrate galactose-alpha-1,3-galactose linked to mammalian-derived products.
- Symptoms can occur hours after exposure, ranging from urticaria to anaphylaxis.
Anaphylaxis Prevention
- Detailed patient histories regarding allergies are essential for risk assessment.
- Prior anaphylaxis, female sex, and pre-existing conditions like asthma or eczema increase risk.
- Close monitoring of patients with known allergies during anesthesia is critical.
Recognizing Anaphylaxis Under Anesthesia
- Presents primarily as circulatory collapse with a triad of hypotension, tachycardia, and bronchospasm.
- Serum tryptase measurement helps confirm anaphylaxis, with samples taken immediately and 24 hours post-event.
Treatment and Referral
- Patients suspected of anaphylaxis should undergo evaluation within 4-6 weeks after the event to gather comprehensive data.
- Detailed records should include surgical reports, symptoms, handling of medications, and any materials used during the procedure.
Anaphylaxis in Anesthesia Overview
- Anaphylaxis is a severe, potentially fatal allergic reaction that can occur during anesthesia.
- Common triggers include antibiotics, neuromuscular blockers (NMBs), latex, chlorhexidine (CHG), and blood products.
Most Common Culprits
- Antibiotics are the leading cause of anaphylaxis in the US.
- Neuromuscular blockers are the second most common in the US, but the primary cause in the UK.
- Other significant allergens include latex, CHG, and blood products.
Types of Allergic Reactions
- Type I (IgE Mediated) Reactions: Primary type of anaphylactic reaction, occurring in 60% of cases.
- Antigens stimulate mast cells and basophils, causing degranulation and release of mediators like histamine, leading to vasodilation and bronchoconstriction.
- Initial localized reactions can escalate quickly as allergens spread through the bloodstream.
Pathophysiology
- Anaphylaxis is marked by complement activation, a reaction cascade that can occur with or without antibodies.
- Three pathways exist: Classical, MB-Lectin, and Alternative, all leading to the release of potent mediators and immune response activation.
Neuromuscular Blockers (NMBAs)
- NMBAs account for 50-70% of allergic reactions during anesthesia.
- Succinylcholine and rocuronium are common culprits; sensitization from first exposure often leads to anaphylaxis upon re-exposure.
- Sugammadex can reverse anaphylaxis by binding rocuronium.
Antibiotics
- Penicillin and its derivatives are responsible for about 70% of allergic reactions in the general population.
- 8-10% cross-reactivity observed with cephalosporins in penicillin-allergic patients; avoid if anaphylaxis occurred from penicillin.
- Vancomycin should be administered slowly to prevent "Red Man Syndrome," characterized by flushing and hypotension.
Latex
- Approximately 20% of perioperative allergies result from latex exposure.
- "Latex fruit syndrome" relates to allergies involving fruits like bananas and avocados.
- Establish latex-free environments for patients with a known latex allergy.
Skin Prep and Contrast Dye
- Iodine and chlorhexidine may trigger allergy responses.
- Radiologic contrast dyes can also be anaphylactic triggers used during surgical procedures.
Opioids
- Commonly cause flushing and urticaria; life-threatening reactions are rare.
- Morphine and meperidine may cause histamine release leading to reactions, including hypotension.
Fluids and Other Agents
- Blood products and colloids can also cause anaphylaxis.
- Specific agents like radiocontrast dye, NSAIDs, insulin, and local anesthetics are potential allergens.
Alpha-Gal Syndrome
- An allergy to the carbohydrate galactose-alpha-1,3-galactose linked to mammalian-derived products.
- Symptoms can occur hours after exposure, ranging from urticaria to anaphylaxis.
Anaphylaxis Prevention
- Detailed patient histories regarding allergies are essential for risk assessment.
- Prior anaphylaxis, female sex, and pre-existing conditions like asthma or eczema increase risk.
- Close monitoring of patients with known allergies during anesthesia is critical.
Recognizing Anaphylaxis Under Anesthesia
- Presents primarily as circulatory collapse with a triad of hypotension, tachycardia, and bronchospasm.
- Serum tryptase measurement helps confirm anaphylaxis, with samples taken immediately and 24 hours post-event.
Treatment and Referral
- Patients suspected of anaphylaxis should undergo evaluation within 4-6 weeks after the event to gather comprehensive data.
- Detailed records should include surgical reports, symptoms, handling of medications, and any materials used during the procedure.
Anaphylaxis in Anesthesia Overview
- Anaphylaxis is a severe, potentially fatal allergic reaction that can occur during anesthesia.
- Common triggers include antibiotics, neuromuscular blockers (NMBs), latex, chlorhexidine (CHG), and blood products.
Most Common Culprits
- Antibiotics are the leading cause of anaphylaxis in the US.
- Neuromuscular blockers are the second most common in the US, but the primary cause in the UK.
- Other significant allergens include latex, CHG, and blood products.
Types of Allergic Reactions
- Type I (IgE Mediated) Reactions: Primary type of anaphylactic reaction, occurring in 60% of cases.
- Antigens stimulate mast cells and basophils, causing degranulation and release of mediators like histamine, leading to vasodilation and bronchoconstriction.
- Initial localized reactions can escalate quickly as allergens spread through the bloodstream.
Pathophysiology
- Anaphylaxis is marked by complement activation, a reaction cascade that can occur with or without antibodies.
- Three pathways exist: Classical, MB-Lectin, and Alternative, all leading to the release of potent mediators and immune response activation.
Neuromuscular Blockers (NMBAs)
- NMBAs account for 50-70% of allergic reactions during anesthesia.
- Succinylcholine and rocuronium are common culprits; sensitization from first exposure often leads to anaphylaxis upon re-exposure.
- Sugammadex can reverse anaphylaxis by binding rocuronium.
Antibiotics
- Penicillin and its derivatives are responsible for about 70% of allergic reactions in the general population.
- 8-10% cross-reactivity observed with cephalosporins in penicillin-allergic patients; avoid if anaphylaxis occurred from penicillin.
- Vancomycin should be administered slowly to prevent "Red Man Syndrome," characterized by flushing and hypotension.
Latex
- Approximately 20% of perioperative allergies result from latex exposure.
- "Latex fruit syndrome" relates to allergies involving fruits like bananas and avocados.
- Establish latex-free environments for patients with a known latex allergy.
Skin Prep and Contrast Dye
- Iodine and chlorhexidine may trigger allergy responses.
- Radiologic contrast dyes can also be anaphylactic triggers used during surgical procedures.
Opioids
- Commonly cause flushing and urticaria; life-threatening reactions are rare.
- Morphine and meperidine may cause histamine release leading to reactions, including hypotension.
Fluids and Other Agents
- Blood products and colloids can also cause anaphylaxis.
- Specific agents like radiocontrast dye, NSAIDs, insulin, and local anesthetics are potential allergens.
Alpha-Gal Syndrome
- An allergy to the carbohydrate galactose-alpha-1,3-galactose linked to mammalian-derived products.
- Symptoms can occur hours after exposure, ranging from urticaria to anaphylaxis.
Anaphylaxis Prevention
- Detailed patient histories regarding allergies are essential for risk assessment.
- Prior anaphylaxis, female sex, and pre-existing conditions like asthma or eczema increase risk.
- Close monitoring of patients with known allergies during anesthesia is critical.
Recognizing Anaphylaxis Under Anesthesia
- Presents primarily as circulatory collapse with a triad of hypotension, tachycardia, and bronchospasm.
- Serum tryptase measurement helps confirm anaphylaxis, with samples taken immediately and 24 hours post-event.
Treatment and Referral
- Patients suspected of anaphylaxis should undergo evaluation within 4-6 weeks after the event to gather comprehensive data.
- Detailed records should include surgical reports, symptoms, handling of medications, and any materials used during the procedure.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.