Podcast
Questions and Answers
What is the outermost layer of the adrenal gland?
What is the outermost layer of the adrenal gland?
- Zona reticularis
- Adrenal medulla
- Capsule (correct)
- Zona fasciculata
Which region of the adrenal cortex is responsible for producing glucocorticoids?
Which region of the adrenal cortex is responsible for producing glucocorticoids?
- Adrenal medulla
- Zona glomerulosa
- Zona reticularis
- Zona fasciculata (correct)
What do the adrenal medulla cells secrete?
What do the adrenal medulla cells secrete?
- Aldosterone
- Cortisol
- Androgens
- Epinephrine and norepinephrine (correct)
Which layer of the adrenal gland is responsible for producing mineralocorticoids?
Which layer of the adrenal gland is responsible for producing mineralocorticoids?
Which part of the adrenal gland is located on top of the kidneys?
Which part of the adrenal gland is located on top of the kidneys?
What is the main function of androgens produced by the adrenal gland?
What is the main function of androgens produced by the adrenal gland?
What does the medulla of the adrenal gland primarily produce?
What does the medulla of the adrenal gland primarily produce?
Which structure surrounds the adrenal gland?
Which structure surrounds the adrenal gland?
Which zone of the adrenal cortex is responsible for the production of glucocorticoids?
Which zone of the adrenal cortex is responsible for the production of glucocorticoids?
Which of the following is NOT a component of the adrenal gland's structure?
Which of the following is NOT a component of the adrenal gland's structure?
What is the main function of the adrenal cortex?
What is the main function of the adrenal cortex?
What is the primary function of corticosteroids produced by the adrenal cortex?
What is the primary function of corticosteroids produced by the adrenal cortex?
Which hormone is responsible for regulating salt and water balance in the body?
Which hormone is responsible for regulating salt and water balance in the body?
Which hormones are categorized as catecholamines produced by the adrenal medulla?
Which hormones are categorized as catecholamines produced by the adrenal medulla?
What is the role of Angiotensin II in the body?
What is the role of Angiotensin II in the body?
What biological response is triggered by hormones released from the adrenal medulla?
What biological response is triggered by hormones released from the adrenal medulla?
What enzyme converts angiotensinogen into angiotensin I?
What enzyme converts angiotensinogen into angiotensin I?
What effect does aldosterone have on the kidneys?
What effect does aldosterone have on the kidneys?
Which hormone is primarily responsible for regulating blood sugar levels?
Which hormone is primarily responsible for regulating blood sugar levels?
What is the primary function of the cells in the Zona Glomerulosa?
What is the primary function of the cells in the Zona Glomerulosa?
Which zone of the adrenal cortex contains spongiocytes?
Which zone of the adrenal cortex contains spongiocytes?
What hormones are primarily secreted by the adrenal medulla?
What hormones are primarily secreted by the adrenal medulla?
Which hormones do the cells in the Zona Reticularis produce?
Which hormones do the cells in the Zona Reticularis produce?
What is the primary role of corticotropin in the adrenal gland?
What is the primary role of corticotropin in the adrenal gland?
What is a key characteristic of the adrenal medulla?
What is a key characteristic of the adrenal medulla?
What type of hormones are secreted by the adrenal medulla?
What type of hormones are secreted by the adrenal medulla?
What effect do the hormones secreted by the adrenal medulla primarily have?
What effect do the hormones secreted by the adrenal medulla primarily have?
Which statement regarding the blood circulation in the adrenal gland is true?
Which statement regarding the blood circulation in the adrenal gland is true?
What term describes the action of hormones from the adrenal medulla mimicking the sympathetic nervous system?
What term describes the action of hormones from the adrenal medulla mimicking the sympathetic nervous system?
What is the primary source of blood supply to the superior part of the adrenal gland?
What is the primary source of blood supply to the superior part of the adrenal gland?
Which artery provides blood to the middle part of the adrenal gland?
Which artery provides blood to the middle part of the adrenal gland?
How does the blood supply to the adrenal medulla primarily occur?
How does the blood supply to the adrenal medulla primarily occur?
What is the source of blood supply for the inferior part of the adrenal gland?
What is the source of blood supply for the inferior part of the adrenal gland?
What type of blood is supplied to the adrenal medulla from the adrenal cortex?
What type of blood is supplied to the adrenal medulla from the adrenal cortex?
What are the three groups of arteries supplying the adrenal gland?
What are the three groups of arteries supplying the adrenal gland?
What is the primary function of the intermediate cortical sinusoids in the adrenal gland?
What is the primary function of the intermediate cortical sinusoids in the adrenal gland?
Which structure forms a plexus just under the capsule of the adrenal gland?
Which structure forms a plexus just under the capsule of the adrenal gland?
What type of blood is supplied to the adrenal medulla from the adrenal cortex?
What type of blood is supplied to the adrenal medulla from the adrenal cortex?
Which arterioles primarily supply blood to the adrenal medulla?
Which arterioles primarily supply blood to the adrenal medulla?
What is the primary source of blood supply to the adrenal gland?
What is the primary source of blood supply to the adrenal gland?
Which structure supplies blood specifically to the adrenal medulla?
Which structure supplies blood specifically to the adrenal medulla?
Which of the following is NOT a pattern of blood distribution within the adrenal cortex?
Which of the following is NOT a pattern of blood distribution within the adrenal cortex?
What do short capsular capillaries primarily supply?
What do short capsular capillaries primarily supply?
What type of blood do intermediate cortical sinusoids drain into?
What type of blood do intermediate cortical sinusoids drain into?
How many groups of suprarenal arteries are involved in the blood supply to the adrenal gland?
How many groups of suprarenal arteries are involved in the blood supply to the adrenal gland?
What type of blood supply primarily supports the adrenal medulla?
What type of blood supply primarily supports the adrenal medulla?
Which of the following correctly describes the drainage process from the adrenal cortex to the medulla?
Which of the following correctly describes the drainage process from the adrenal cortex to the medulla?
Which vein collects blood before it exits the adrenal gland?
Which vein collects blood before it exits the adrenal gland?
What is the final drainage point for blood leaving the adrenal gland?
What is the final drainage point for blood leaving the adrenal gland?
What path does venous blood take after draining from the adrenal cortex?
What path does venous blood take after draining from the adrenal cortex?
Which condition is characterized by an excess of aldosterone?
Which condition is characterized by an excess of aldosterone?
What is a common symptom associated with Cushing's syndrome?
What is a common symptom associated with Cushing's syndrome?
Which syndrome is the result of adrenal insufficiency?
Which syndrome is the result of adrenal insufficiency?
What condition may present with symptoms of muscle weakness and amenorrhea?
What condition may present with symptoms of muscle weakness and amenorrhea?
Which hormonal imbalance can lead to osteoporosis?
Which hormonal imbalance can lead to osteoporosis?
What is the primary function of the acinar cells in the pancreas?
What is the primary function of the acinar cells in the pancreas?
Which hormone is primarily produced in the Islets of Langerhans of the pancreas?
Which hormone is primarily produced in the Islets of Langerhans of the pancreas?
What type of solution do duct cells in the pancreas secrete?
What type of solution do duct cells in the pancreas secrete?
Which of the following structures is NOT part of the anatomical layout associated with the pancreas?
Which of the following structures is NOT part of the anatomical layout associated with the pancreas?
Which hormones are primarily involved in regulating glucose metabolism?
Which hormones are primarily involved in regulating glucose metabolism?
What are the functional units of the exocrine pancreas called?
What are the functional units of the exocrine pancreas called?
Which part of the pancreas is identified by pale staining?
Which part of the pancreas is identified by pale staining?
How is the exocrine portion of the pancreas primarily stained in histological images?
How is the exocrine portion of the pancreas primarily stained in histological images?
What is the primary function of the pancreas's endocrine component?
What is the primary function of the pancreas's endocrine component?
Which of the following is a characteristic feature of acini in the pancreas?
Which of the following is a characteristic feature of acini in the pancreas?
What is the primary function of acinar cells in the pancreas?
What is the primary function of acinar cells in the pancreas?
Which hormones are produced by the pancreatic islets?
Which hormones are produced by the pancreatic islets?
How are the digestive enzymes produced by acinar cells transported to the duodenum?
How are the digestive enzymes produced by acinar cells transported to the duodenum?
What is unique about the secretion of hormones from the pancreatic islets?
What is unique about the secretion of hormones from the pancreatic islets?
Which of the following enzymes is NOT produced by acinar cells?
Which of the following enzymes is NOT produced by acinar cells?
What surrounds each islet in the pancreas?
What surrounds each islet in the pancreas?
What type of blood vessels supply each islet in the pancreas?
What type of blood vessels supply each islet in the pancreas?
Which component supports the cells in the islet of Langerhans?
Which component supports the cells in the islet of Langerhans?
How do the glandular cells in the islets of Langerhans typically appear?
How do the glandular cells in the islets of Langerhans typically appear?
What characterizes the cells of the surrounding exocrine pancreatic acini compared to islet cells?
What characterizes the cells of the surrounding exocrine pancreatic acini compared to islet cells?
What is the primary function of α cells in the Islets of Langerhans?
What is the primary function of α cells in the Islets of Langerhans?
Which hormone is secreted by β cells in the Islets of Langerhans?
Which hormone is secreted by β cells in the Islets of Langerhans?
What role does somatostatin, produced by delta cells, have in the islets?
What role does somatostatin, produced by delta cells, have in the islets?
What is known about the function of pancreatic polypeptide (PP) cells?
What is known about the function of pancreatic polypeptide (PP) cells?
What is the primary role of insulin in the body?
What is the primary role of insulin in the body?
Which condition is a result of insufficient insulin production?
Which condition is a result of insufficient insulin production?
What role does glucagon play when blood glucose levels are low?
What role does glucagon play when blood glucose levels are low?
Which hormone is secreted by beta cells in the pancreas?
Which hormone is secreted by beta cells in the pancreas?
What is one of the effects of insulin in the body?
What is one of the effects of insulin in the body?
What happens when blood glucose levels rise?
What happens when blood glucose levels rise?
Which statement about glucagon is false?
Which statement about glucagon is false?
Flashcards are hidden until you start studying
Study Notes
Anatomy
- Adrenal glands are positioned on top of each kidney.
- Two distinct adrenal glands are illustrated in the accompanying images.
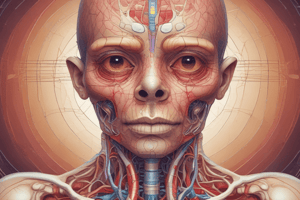
Histology
- The adrenal gland consists of multiple layers, observable in magnified images.
- The layers include:
- Capsule: Outermost protective layer.
- Zona glomerulosa: Produces mineralocorticoids, primarily aldosterone, which regulates sodium and potassium balance.
- Zona fasciculata: Responsible for producing glucocorticoids, especially cortisol, involved in stress response and metabolism regulation.
- Zona reticularis: Produces androgens, which contribute to the development of male characteristics and reproductive function.
- The adrenal medulla, the innermost region, secretes epinephrine (adrenaline) and norepinephrine (noradrenaline), key hormones in the fight-or-flight response.
- Caption indicates that the image represents the histology of the adrenal cortex and a portion of the adrenal medulla.
Structure of the Adrenal Gland
- Composed of an outer dense fibrous connective tissue capsule, providing protection and support.
- Divided into two main regions: the cortex (outer layer) and the medulla (inner layer).
Adrenal Cortex
- The cortex contains three distinct zones, each responsible for synthesizing specific hormones.
- Hormones produced by the cortex include corticosteroids which regulate metabolism, immune response, and stress responses.
Adrenal Medulla
- The medulla functions as part of the sympathetic nervous system and produces vital catecholamines.
- Main hormones produced are adrenaline (epinephrine) and noradrenaline (norepinephrine), essential for the body's fight-or-flight response.
Histological Features
- Cross-section of the adrenal gland reveals key structures:
- Capsule: protective outer layer.
- Cortex: hormone-secreting outer portion.
- Medulla: inner part responsible for adrenaline production.
- Presence of fenestrated capillaries, allowing efficient hormone release into the bloodstream.
- Group of glandular cells indicates areas of hormone synthesis.
- Reticular fibers contribute to the structural integrity of the gland.
Adrenal Gland Overview
- Located above the kidneys, adrenal glands are crucial for producing life-sustaining hormones.
- Comprised of two layers: the adrenal cortex (outer layer) and adrenal medulla (inner layer).
Adrenal Cortex
- Corticosteroids: Three main types produced
- Aldosterone: Essential for regulating salt and water balance in the body.
- Cortisol: Crucial for blood sugar regulation and stress response.
- Androgens: Serve as sex hormones involved in various bodily functions.
- Overall function includes regulation of water levels and metabolism of carbohydrates, proteins, and fats.
Adrenal Medulla
- Catecholamines: Two primary hormones
- Adrenaline (epinephrine): Involved in the acute stress response.
- Noradrenaline (norepinephrine): Works alongside adrenaline during stress responses.
- Function focuses on initiating and supporting the body's "fight-or-flight" response in the face of danger.
Renin-Angiotensin-Aldosterone System (RAAS)
- Renin: Enzyme released by kidneys that transforms angiotensinogen into angiotensin I.
- Angiotensin I: A precursor that requires conversion to exert effects.
- Angiotensin-Converting Enzyme (ACE): Converts angiotensin I to angiotensin II.
- Angiotensin II: Powerful vasoconstrictor that increases blood pressure and stimulates aldosterone release.
- Aldosterone: Promotes sodium and water reabsorption in kidneys, further increasing blood pressure.
- This system plays a vital role in maintaining blood pressure during drops in levels.
Adrenal Gland Overview
- Located on top of each kidney, crucial in producing hormones that regulate metabolism, immune response, and stress.
Capsule
- The adrenal gland is encased in a protective capsule that helps maintain its structure.
Zones of Cortex
-
Zona Glomerulosa:
- Features round or horse-shoe-shaped clusters of glandular cells.
- Responsible for the secretion of mineralocorticoids, primarily aldosterone.
- Regulates sodium (Na+) balance and fluid homeostasis.
-
Zona Fasiculata:
- Composed of long, parallel cords of cells known as spongiocytes, interspersed with sinusoidal capillaries.
- Secretes glucocorticoids such as cortisol and corticosterone, along with some androgens.
- Regulated by ACTH (adrenocorticotropic hormone); plays vital roles in stress response and inflammation reduction.
-
Zona Reticularis:
- Contains anastomosing cords of glandular cells that produce androgens and limited amounts of glucocorticoids.
Medulla
- Made up of chromaffin cells that are densely packed in irregular cords.
- Produces catecholamines, including norepinephrine and epinephrine.
- Known as "ballistic control hormones" which play a critical role in the body’s fight or flight response.
Medulla of the Adrenal Gland
- Lacks a protective capsule, unlike typical endocrine glands.
- Principal hormones secreted are adrenaline (epinephrine) and noradrenaline (norepinephrine).
- These hormones are classified as sympathomimetic, meaning they mimic the effects of the sympathetic nervous system.
Function of Medullary Hormones
- Often referred to as "ballistic control hormones" due to their role in the body's rapid response mechanisms.
- Key in triggering the "fight or flight" response, preparing the body for stressful situations.
Blood Drainage in the Medulla
- Venous channels collect blood from the sinusoids located in the adrenal cortex.
- Blood is directed through the medulla before draining into the central medullary vein, facilitating hormone distribution.
Blood Supply to the Adrenal Gland
- The adrenal gland features a complex blood supply system, with varying sources for its two regions: the cortex and the medulla.
Adrenal Cortex Blood Supply
- Primarily supplied by three arteries:
- Superior Suprarenal Artery:
- Originates from the inferior phrenic artery (a branch of the abdominal aorta).
- Supplies blood to the superior region of the adrenal gland.
- Middle Suprarenal Artery:
- Comes directly from the abdominal aorta.
- Supplies blood to the middle portion of the adrenal gland.
- Inferior Suprarenal Artery:
- Arises from the renal artery, another branch of the abdominal aorta.
- Supplies blood to the inferior section of the adrenal gland.
- Superior Suprarenal Artery:
Adrenal Medulla Blood Supply
- Unique blood supply characteristics, marked by the involvement of sympathetic nerve fibers.
- Receives:
- "Venous" Blood: Comes from cortical sinusoids located in the adrenal cortex.
- Arterial Blood: Supplied by specialized medullary arterioles, ensuring effective nutrient delivery.
Blood Supply of the Adrenal Gland
- Supplied by three groups of suprarenal arteries: superior, middle, and inferior.
- Short capsular capillaries specifically nourish the adrenal capsule.
- These capillaries branch into an arterial subcapsular plexus, providing additional support to the capsule.
Dual Blood Supply System
- Blood flows through intermediate cortical sinusoids, which drain into the zona reticularis plexus.
- The zona reticularis plexus delivers necessary blood to the adrenal cortex.
- Long medullary arterioles supply the adrenal medulla, ensuring adequate delivery of nutrients and oxygen.
- Medullary arterioles carry arterial blood, while "venous" blood is collected from the cortical sinusoids after its passage through the cortex.
- A subcapsular plexus forms just beneath the capsule, aiding in blood distribution.
- Another plexus is established in the zona reticularis, facilitating further blood flow within the adrenal gland.
Blood Supply to Adrenal Gland Cortex
- Suprarenal arteries consist of three groups: superior, middle, and inferior, branching from the renal arteries.
- Each group of suprarenal arteries forms multiple small arteries that penetrate the adrenal capsule.
- Blood distribution in the cortex occurs through three main patterns:
- Short capsular capillaries supply the adrenal capsule.
- These capillaries branch into an arterial subcapsular plexus, which supplies the cortex.
- Intermediate cortical sinusoids help in further distributing blood within the cortical region.
- Blood drains into the ** zona reticularis plexus**, ensuring efficient venous return.
- Cortical sinusoids carry "venous" blood, facilitating the flow through the cortex.
Blood Supply to Adrenal Gland Medulla
- Long medullary arterioles provide a direct blood supply to the adrenal medulla.
- These arterioles ensure a robust supply of arterial blood specifically for medullary function.
Diagram Overview
- The diagram illustrates the adrenal gland's blood supply with color-coded arteries: blue, red, and black lines indicate different arteries.
- Green lines in the diagram represent blood vessel plexuses, highlighting their locations within the gland.
- Numbers on the diagram correspond to the discussed points about blood supply and distribution.
Blood Supply of the Adrenal Gland Medulla
- The medulla receives a dual blood supply: arterial and venous.
- Venous blood comes from cortical sinusoids, draining through the cortex.
- Arterial blood is supplied directly by medullary arterioles.
Mechanism of Blood Drainage
- Venous blood from the cortex drains into venules located within the medulla.
- These venules converge into small adrenomedullary collecting veins.
- Collecting veins merge to form the Large Central Adrenomedullary Vein.
- This large vein ultimately drains into the suprarenal vein.
- Blood exits the adrenal gland at the hilus, the gland's entry and exit point.
Clinical Imbalances of Adrenal Gland Hormones
- Cushing's Syndrome: Excess cortisol leading to various symptoms.
- Nelson's Syndrome: Develops due to pituitary adenoma after adrenalectomy for Cushing's.
- Pseudo-Cushing's Syndrome: Symptoms mimic Cushing's due to factors like depression or alcoholism.
- Hyperaldosteronism: Overproduction of aldosterone, resulting in electrolyte imbalances and hypertension.
- Conn Syndrome: A specific type of hyperaldosteronism usually caused by an adrenal tumor.
- Bartter Syndrome: Genetic condition causing renal salt wasting, often leads to secondary hyperaldosteronism.
Adrenal Insufficiency
- Addison's Disease: Underproduction of adrenal hormones, particularly cortisol and aldosterone.
- Hypoaldosteronism: Low levels of aldosterone contribute to fluid and electrolyte imbalances.
Effects of Hyperaldosteronism
- Elevated aldosterone can lead to calcium insufficiency and various cardiovascular complications.
Symptoms Associated with Adrenal Gland Disorders
- Emotional Disturbance: Mood swings and psychological effects due to hormonal imbalances.
- Enlarged Sella Turcica: Associated with pituitary gland enlargement, often linked with tumors.
- Moon Facies: Rounded facial features commonly seen in Cushing's syndrome.
- Osteoporosis: Weakening of bones, increased risk of fractures due to hormonal effects.
- Cardiac Hypertrophy: Enlargement of the heart due to chronic hypertension from aldosterone excess.
- Buffalo Hump: Accumulation of fat at the nape of the neck, indicative of Cushing's syndrome.
- Obesity: Central obesity linked to excess cortisol production.
- Adrenal Tumor or Hyperplasia: Abnormal growth of adrenal tissue affects hormone levels.
- Thin, Wrinkled Skin: Loss of collagen and skin integrity due to hormonal imbalances.
- Abdominal Striae: Stretch marks resulting from skin stretching due to rapid weight gain.
- Amenorrhea: Absence of menstruation linked to hormonal disruptions.
- Muscle Weakness: Loss of muscle mass and strength due to cortisol's effects on muscle tissue.
- Purpura: Easy bruising due to skin fragility and blood vessel weakening.
- Skin Ulcers: Poor wound healing linked to glucocorticoid excess.
Anatomy of the Pancreas
- The pancreas is located near the duodenum, connecting to the bile duct from the liver.
- It plays a critical role in digestion and blood sugar regulation.
- Insulin and glucagon are the primary hormones produced by the pancreas, regulating glucose levels in the bloodstream.
- Blood supply is essential for the delivery of hormones and nutrients to the pancreas and overall metabolism.
- Duct cells are responsible for secreting an aqueous solution of sodium bicarbonate (NaHCO3), which helps neutralize stomach acid in the duodenum.
- Acinar cells produce digestive enzymes such as amylase, lipase, and proteases, essential for breaking down carbohydrates, fats, and proteins in the digestive process.
- The endocrine portion of the pancreas, known as the Islets of Langerhans, contains clusters of cells that secrete hormones directly into the bloodstream, playing a vital role in metabolic regulation.
Pancreas Overview
- Pancreas functions as both an endocrine and exocrine gland.
Endocrine Function
- Contains pancreatic islets (Islets of Langerhans) dispersed within the exocrine tissue.
- Islets are involved in hormone production and regulation.
Exocrine Function
- Functional units are known as acini, responsible for digestive enzyme secretion.
- Acini are arranged in groups, appearing as a darker pink on microscopic images.
Microscopic Imaging
- Right image: Shows low magnification of the entire pancreas, highlighting the pale staining of the endocrine portion.
- Left image: Features high magnification of the exocrine pancreas with a darker pink appearance, revealing distinct cell shapes and blood vessels.
Pancreas Functions
Exocrine Function (Digestive)
- Acinar cells are specialized cells in the pancreas that generate digestive enzymes.
- Key enzymes produced include:
- Amylase: breaks down carbohydrates
- Trypsin: digests proteins
- Peptidase: further aids in protein digestion
- Lipase: helps in the breakdown of fats
- Digestive enzymes are collectively known as pancreatic juice.
- Pancreatic juice is transported through ducts into the duodenum, the first segment of the small intestine.
Endocrine Function (Hormonal)
- Pancreatic Islets, also known as islets of Langerhans, are clusters of cells scattered throughout the pancreas.
- These islets are responsible for the production of key hormones, including:
- Insulin: lowers blood sugar levels by facilitating glucose uptake by cells
- Glucagon: increases blood sugar levels by promoting the release of glucose stored in the liver
- Hormones produced by the pancreatic islets are released directly into the bloodstream, making this a ductless function.
Typical Endocrine Gland Structure
- Islets of Langerhans are surrounded by a delicate, thin connective tissue capsule.
- Cells within the islets are supported by a fine network of reticular fibers.
- This network contains numerous highly branched fenestrated capillaries that facilitate hormone secretion into the bloodstream.
- Each islet receives blood supply from as many as three arterioles.
- Glandular cells within the islets form small clusters and have a pale-stained granular cytoplasm.
- In contrast, larger cells in the surrounding exocrine pancreatic acini exhibit strong staining, highlighting their functional differences.
Pancreas: Islets of Langerhans Cells
- Islets function as endocrine units within the pancreas, producing hormones such as insulin and glucagon.
- These hormones play crucial roles in regulating blood glucose levels and metabolism.
- The cellular composition of the islets includes several types of hormone-secreting cells, each with distinct functions.
Islets of Langerhans Overview
- Located in the pancreas, Islets of Langerhans are groups of endocrine cells.
- They play a crucial role in regulating blood glucose levels through hormone secretion.
Types of Cells and Their Functions
-
α (Alpha) Cells:
- Secrete glucagon.
- Responsible for increasing blood glucose levels during fasting or between meals.
-
β (Beta) Cells:
- Secrete insulin.
- Functions to lower blood glucose levels by facilitating the uptake of glucose by cells.
-
δ (Delta) Cells:
- Produce somatostatin.
- Inhibits the secretion of glucagon, insulin, and pancreatic polypeptide, helping to regulate overall hormone balance.
-
F (PP) Cells:
- Secrete pancreatic polypeptide.
- Unclear function, but may be involved in appetite regulation.
-
C Cells and E Cells:
- C cells may produce calcitonin similar to thyroid function; E cells have unspecified roles.
Hormonal Imbalance in Islets of Langerhans
- Hormonal imbalances can significantly affect glucose homeostasis.
- Dysregulation of insulin and glucagon levels can lead to conditions like diabetes mellitus.
- Proper functioning of all types of cells in the islets is critical for maintaining metabolic balance.
Islets of Langerhans and Hormonal Imbalance
- Islet cells' inability to produce insulin or insufficient insulin production leads to diabetes mellitus.
- Diabetes mellitus is categorized into:
- Type I Diabetes: Often caused by autoimmune destruction of insulin-producing beta cells.
- Type II Diabetes: Generally associated with insulin resistance and insufficient insulin secretion.
Pancreatic Regulation of Blood Glucose
- The pancreas plays a critical role in maintaining blood glucose levels through hormone secretion.
- Key pancreatic cells involved:
- Alpha Cells: Secrete glucagon.
- Beta Cells: Secrete insulin.
Hormonal Effects on Blood Glucose Levels
- Glucagon:
- Triggers conversion of glycogen to glucose in the liver.
- Stimulates gluconeogenesis by forming glucose from lactic acid and amino acids.
- Insulin:
- Promotes facilitated diffusion, allowing glucose to enter cells more efficiently.
- Accelerates conversion of glucose to glycogen for storage.
- Enhances amino acid uptake, boosting protein synthesis.
- Facilitates the synthesis of fatty acids.
- Inhibits glycogenolysis (breakdown of glycogen) and gluconeogenesis (creation of glucose).
Feedback Mechanism
- When blood glucose levels decrease, alpha cells increase glucagon production to elevate blood glucose.
- Conversely, when blood glucose levels rise, beta cells increase insulin secretion to lower blood glucose levels back to normal.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.