Podcast
Questions and Answers
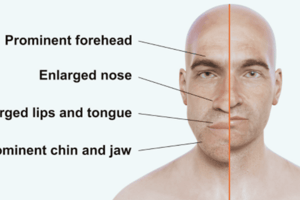
What is the most common cause of acromegaly?
What is the most common cause of acromegaly?
- Hypothalamic dysfunction
- Somatotroph adenoma (correct)
- Pancreatic adenoma
- Neuroendocrine tumor
Which of the following hormonal dysregulations can occur as a complication of acromegaly in men?
Which of the following hormonal dysregulations can occur as a complication of acromegaly in men?
- Increased thyroid hormone levels
- Decreased testosterone production (correct)
- Elevated cortisol levels
- Increased growth hormone secretion
What is the annual incidence of acromegaly?
What is the annual incidence of acromegaly?
- 2/1 million people
- 20/1 million people
- 50/1 million people
- 10/1 million people (correct)
What metabolic condition is associated with uncontrolled acromegaly?
What metabolic condition is associated with uncontrolled acromegaly?
Which cardiovascular condition is commonly seen in patients with acromegaly?
Which cardiovascular condition is commonly seen in patients with acromegaly?
What is a common complication related to the renal system in patients with acromegaly?
What is a common complication related to the renal system in patients with acromegaly?
What is the age range in which acromegaly is typically diagnosed?
What is the age range in which acromegaly is typically diagnosed?
Which condition is speculated to have an increased risk in patients with acromegaly?
Which condition is speculated to have an increased risk in patients with acromegaly?
What is the primary function of antidiuretic hormone (ADH)?
What is the primary function of antidiuretic hormone (ADH)?
Which IV fluid type would most likely be used to correct cellular dehydration?
Which IV fluid type would most likely be used to correct cellular dehydration?
In diabetes insipidus, what primary issue affects urine concentration?
In diabetes insipidus, what primary issue affects urine concentration?
What is the measured unit for osmolality?
What is the measured unit for osmolality?
What induces the release of antidiuretic hormone (ADH)?
What induces the release of antidiuretic hormone (ADH)?
Which fluid type increases extracellular fluid volume without changing solute concentration?
Which fluid type increases extracellular fluid volume without changing solute concentration?
What condition is typically associated with excessive plasma sodium concentration?
What condition is typically associated with excessive plasma sodium concentration?
What characteristic defines hypertonic IV fluids?
What characteristic defines hypertonic IV fluids?
What physiological state is characterized by a sodium level greater than 145 mEq/L?
What physiological state is characterized by a sodium level greater than 145 mEq/L?
What is a potential consequence of hypernatremia on the nervous system?
What is a potential consequence of hypernatremia on the nervous system?
Which type of Diabetes Insipidus is characterized by renal tubules failing to respond to ADH?
Which type of Diabetes Insipidus is characterized by renal tubules failing to respond to ADH?
What is a common cause of Central Diabetes Insipidus?
What is a common cause of Central Diabetes Insipidus?
Which kidney-related condition can lead to Nephrogenic Diabetes Insipidus?
Which kidney-related condition can lead to Nephrogenic Diabetes Insipidus?
What test can help diagnose Diabetes Insipidus by assessing urine concentration?
What test can help diagnose Diabetes Insipidus by assessing urine concentration?
What symptom is NOT typically associated with Diabetes Insipidus?
What symptom is NOT typically associated with Diabetes Insipidus?
Which of the following is a potential diagnosis method for Diabetes Insipidus?
Which of the following is a potential diagnosis method for Diabetes Insipidus?
What is the recommended duration of vigorous-intensity aerobic physical activity for adults per week?
What is the recommended duration of vigorous-intensity aerobic physical activity for adults per week?
Which of the following is NOT a technique used in cognitive behavioral therapy for changing dietary and physical activity behaviors?
Which of the following is NOT a technique used in cognitive behavioral therapy for changing dietary and physical activity behaviors?
What is the body mass index (BMI) threshold for considering pharmacological treatment for obesity in patients without related health diseases?
What is the body mass index (BMI) threshold for considering pharmacological treatment for obesity in patients without related health diseases?
Which of the following is a mechanism of action (MOA) for Orlistat?
Which of the following is a mechanism of action (MOA) for Orlistat?
What primarily contributes to the increased prevalence of metabolic syndrome in older populations?
What primarily contributes to the increased prevalence of metabolic syndrome in older populations?
Which side effect is commonly associated with the use of Orlistat?
Which side effect is commonly associated with the use of Orlistat?
Which of the following is NOT considered a notable symptom associated with metabolic syndrome?
Which of the following is NOT considered a notable symptom associated with metabolic syndrome?
What is a key recommendation for patients when considering behavioral lifestyle changes?
What is a key recommendation for patients when considering behavioral lifestyle changes?
Which of these medications is classified as an appetite suppressant for obesity treatment?
Which of these medications is classified as an appetite suppressant for obesity treatment?
What is the primary pathophysiological hypothesis explaining metabolic syndrome?
What is the primary pathophysiological hypothesis explaining metabolic syndrome?
What is a major challenge associated with maintaining weight loss?
What is a major challenge associated with maintaining weight loss?
What should be monitored to correlate with activity level in daily living?
What should be monitored to correlate with activity level in daily living?
Which factor is least likely to contribute to the development of metabolic syndrome?
Which factor is least likely to contribute to the development of metabolic syndrome?
How is metabolic syndrome most commonly diagnosed?
How is metabolic syndrome most commonly diagnosed?
What percentage of American women are estimated to experience hirsutism?
What percentage of American women are estimated to experience hirsutism?
What lifestyle change is indicated as a significant factor for combating metabolic syndrome?
What lifestyle change is indicated as a significant factor for combating metabolic syndrome?
Which hormone is considered to predominantly influence hirsutism in women?
Which hormone is considered to predominantly influence hirsutism in women?
Which condition shares many common characteristics with metabolic syndrome due to hormonal imbalances?
Which condition shares many common characteristics with metabolic syndrome due to hormonal imbalances?
Which ethnic group tends to exhibit less body hair than others, specifically in terms of hirsutism?
Which ethnic group tends to exhibit less body hair than others, specifically in terms of hirsutism?
Which of the following habits is most likely to exacerbate metabolic syndrome?
Which of the following habits is most likely to exacerbate metabolic syndrome?
In which condition is there an excess of circulating androgens resulting in symptoms of virilization?
In which condition is there an excess of circulating androgens resulting in symptoms of virilization?
What characteristic defines idiopathic hirsutism?
What characteristic defines idiopathic hirsutism?
How does androgen excess affect hair growth in androgen-sensitive sites?
How does androgen excess affect hair growth in androgen-sensitive sites?
Which condition is characterized by excessive male-pattern hair growth in women of reproductive age?
Which condition is characterized by excessive male-pattern hair growth in women of reproductive age?
Which of the following symptoms is commonly associated with Cushing Syndrome?
Which of the following symptoms is commonly associated with Cushing Syndrome?
In the evaluation of polycystic ovarian syndrome (PCOS), what is the primary criterion for diagnosis without the need for transvaginal ultrasound (TVUS)?
In the evaluation of polycystic ovarian syndrome (PCOS), what is the primary criterion for diagnosis without the need for transvaginal ultrasound (TVUS)?
The biphasic pattern observed on a basal body temperature chart indicates what?
The biphasic pattern observed on a basal body temperature chart indicates what?
Which diagnostic tool may be used in cases of suspected hyperandrogenism when menstrual cycles are normal?
Which diagnostic tool may be used in cases of suspected hyperandrogenism when menstrual cycles are normal?
What factor is NOT a common symptom observed in both oligomenorrhea and Cushing Syndrome?
What factor is NOT a common symptom observed in both oligomenorrhea and Cushing Syndrome?
What is the primary recommended goal for weight loss over six months?
What is the primary recommended goal for weight loss over six months?
Which of the following factors can indicate secondary obesity?
Which of the following factors can indicate secondary obesity?
In an initial workup for obesity, which lab test is NOT typically performed?
In an initial workup for obesity, which lab test is NOT typically performed?
What caloric intake is recommended for women to promote weight loss?
What caloric intake is recommended for women to promote weight loss?
What is considered the most effective behavioral approach to treat obesity?
What is considered the most effective behavioral approach to treat obesity?
Which dietary approach is noted to produce effective weight loss in the short term?
Which dietary approach is noted to produce effective weight loss in the short term?
What is a common pitfall in dietary intervention studies for obesity?
What is a common pitfall in dietary intervention studies for obesity?
Which condition could contribute to obesity through hormonal dysregulation?
Which condition could contribute to obesity through hormonal dysregulation?
Insulin therapy is essential for the treatment of which type of diabetes in adults?
Insulin therapy is essential for the treatment of which type of diabetes in adults?
What is the primary indicator that a patient should be presumed to have type 1 diabetes rather than LADA?
What is the primary indicator that a patient should be presumed to have type 1 diabetes rather than LADA?
Which screening timeframe is recommended for gestational diabetes in pregnant women?
Which screening timeframe is recommended for gestational diabetes in pregnant women?
What complication is associated with gestational diabetes that significantly affects neonates?
What complication is associated with gestational diabetes that significantly affects neonates?
Which factor increases the risk of developing preeclampsia in patients with gestational diabetes?
Which factor increases the risk of developing preeclampsia in patients with gestational diabetes?
Which long-term risk is associated with gestational diabetes for maternal health?
Which long-term risk is associated with gestational diabetes for maternal health?
What is the importance of calorie restriction and physical activity for obese LADA patients?
What is the importance of calorie restriction and physical activity for obese LADA patients?
What risk is associated with uncontrolled glucose levels in pregnant women with gestational diabetes?
What risk is associated with uncontrolled glucose levels in pregnant women with gestational diabetes?
What is a significant neonatal morbidity risk associated with gestational diabetes?
What is a significant neonatal morbidity risk associated with gestational diabetes?
What immediate intervention is critical following a diagnosis of Latent autoimmune diabetes in adults (LADA)?
What immediate intervention is critical following a diagnosis of Latent autoimmune diabetes in adults (LADA)?
Which feature is least likely to be associated with MODY?
Which feature is least likely to be associated with MODY?
What is a common characteristic of patients with LADA?
What is a common characteristic of patients with LADA?
What criteria suggests that a patient may have MODY rather than type II diabetes?
What criteria suggests that a patient may have MODY rather than type II diabetes?
Which of the following statements about genetic testing in diabetes is correct?
Which of the following statements about genetic testing in diabetes is correct?
Which group is least likely to develop LADA?
Which group is least likely to develop LADA?
What test is most relevant in the diagnosis of LADA or type 1 diabetes when clinical presentation is uncertain?
What test is most relevant in the diagnosis of LADA or type 1 diabetes when clinical presentation is uncertain?
How does insulin resistance present in patients with MODY?
How does insulin resistance present in patients with MODY?
What risk factor is commonly evaluated before genetic testing for MODY?
What risk factor is commonly evaluated before genetic testing for MODY?
Which of the following best describes the progression of diabetes in LADA?
Which of the following best describes the progression of diabetes in LADA?
Which combination of features might suggest the diagnosis of MODY?
Which combination of features might suggest the diagnosis of MODY?
Which screening test is performed at 24-28 weeks gestational age for gestational diabetes?
Which screening test is performed at 24-28 weeks gestational age for gestational diabetes?
What constitutes an abnormal result in a 1-hour serum glucose test during the oral glucose challenge?
What constitutes an abnormal result in a 1-hour serum glucose test during the oral glucose challenge?
Which dietary macronutrient should be limited to ensure no more than 40% of the total caloric intake in gestational diabetes management?
Which dietary macronutrient should be limited to ensure no more than 40% of the total caloric intake in gestational diabetes management?
What is the primary goal for fasting blood sugar in gestational diabetes management?
What is the primary goal for fasting blood sugar in gestational diabetes management?
Which medication is considered the first-line treatment for patients with gestational diabetes who do not achieve adequate control with lifestyle modifications?
Which medication is considered the first-line treatment for patients with gestational diabetes who do not achieve adequate control with lifestyle modifications?
How is the glucose load administered during the 3-hour OGTT?
How is the glucose load administered during the 3-hour OGTT?
What is the key characteristic of dietary management in gestational diabetes?
What is the key characteristic of dietary management in gestational diabetes?
What blood sugar level indicates gestational diabetes after the 3-hour OGTT?
What blood sugar level indicates gestational diabetes after the 3-hour OGTT?
What is a primary physical activity recommendation for managing gestational diabetes?
What is a primary physical activity recommendation for managing gestational diabetes?
For which patient condition is glyburide recommended as an alternative treatment for gestational diabetes?
For which patient condition is glyburide recommended as an alternative treatment for gestational diabetes?
What genetic inheritance pattern is associated with Maturity Onset Diabetes of the Young (MODY)?
What genetic inheritance pattern is associated with Maturity Onset Diabetes of the Young (MODY)?
Which mutation is primarily associated with the mild form of MODY that may not require treatment?
Which mutation is primarily associated with the mild form of MODY that may not require treatment?
Latent Autoimmune Diabetes in Adults (LADA) typically develops into what condition over time?
Latent Autoimmune Diabetes in Adults (LADA) typically develops into what condition over time?
What is the primary distinction between gestational diabetes mellitus (GDM) and other types of diabetes?
What is the primary distinction between gestational diabetes mellitus (GDM) and other types of diabetes?
How common is Maturity Onset Diabetes of the Young (MODY) among all diabetes cases?
How common is Maturity Onset Diabetes of the Young (MODY) among all diabetes cases?
What condition may arise as a complication of hyperglycemia from HNF mutations in MODY?
What condition may arise as a complication of hyperglycemia from HNF mutations in MODY?
Which of the following statements about LADA is NOT true?
Which of the following statements about LADA is NOT true?
Which feature is characteristic of babies born to mothers with gestational diabetes?
Which feature is characteristic of babies born to mothers with gestational diabetes?
What is the recommended insulin dose based on a patient's weight for treating gestational diabetes?
What is the recommended insulin dose based on a patient's weight for treating gestational diabetes?
In the insulin regimen, what proportion of the total daily insulin dose is given in the morning prior to breakfast?
In the insulin regimen, what proportion of the total daily insulin dose is given in the morning prior to breakfast?
What method is used for fetal monitoring during labor in diabetic patients?
What method is used for fetal monitoring during labor in diabetic patients?
What is the maximum recommended daily dosage for PRN insulin in the context of gestational diabetes?
What is the maximum recommended daily dosage for PRN insulin in the context of gestational diabetes?
After delivery, what change occurs in insulin requirements for postpartum patients?
After delivery, what change occurs in insulin requirements for postpartum patients?
In managing gestational diabetes, which type of insulin should be given in the evening before dinner?
In managing gestational diabetes, which type of insulin should be given in the evening before dinner?
At what gestational age should serial biophysical profiling (BPP) begin for managing diabetes in pregnancy?
At what gestational age should serial biophysical profiling (BPP) begin for managing diabetes in pregnancy?
Which factor is not recommended for management of diabetes in patients with vascular disease?
Which factor is not recommended for management of diabetes in patients with vascular disease?
What imaging technique is known as the gold standard for evaluating pituitary masses?
What imaging technique is known as the gold standard for evaluating pituitary masses?
Which of the following hormonal evaluations is performed based on symptoms of hypopituitarism?
Which of the following hormonal evaluations is performed based on symptoms of hypopituitarism?
When should evaluation for a pituitary mass be considered?
When should evaluation for a pituitary mass be considered?
What defines a microadenoma in terms of size?
What defines a microadenoma in terms of size?
Which factor is NOT typically included when choosing laboratory evaluations for pituitary masses?
Which factor is NOT typically included when choosing laboratory evaluations for pituitary masses?
What is one of the main goals in the treatment of pituitary adenomas?
What is one of the main goals in the treatment of pituitary adenomas?
For which type of pituitary tumor is medical management using dopamine agonists particularly effective?
For which type of pituitary tumor is medical management using dopamine agonists particularly effective?
What imaging feature suggests the presence of a craniopharyngioma in a pituitary mass?
What imaging feature suggests the presence of a craniopharyngioma in a pituitary mass?
What surgical approach is typically desired for the resection of pituitary tumors?
What surgical approach is typically desired for the resection of pituitary tumors?
An incidental finding of a pituitary mass requires investigation for which of the following?
An incidental finding of a pituitary mass requires investigation for which of the following?
Which statement accurately describes the nature of most pituitary tumors?
Which statement accurately describes the nature of most pituitary tumors?
What is the first-line medical treatment for prolactinoma?
What is the first-line medical treatment for prolactinoma?
What outcome is indicative of successful treatment of a large invasive prolactinoma after starting cabergoline?
What outcome is indicative of successful treatment of a large invasive prolactinoma after starting cabergoline?
What condition is characterized by severe acute hemorrhage into the pituitary gland, often associated with a preexisting adenoma?
What condition is characterized by severe acute hemorrhage into the pituitary gland, often associated with a preexisting adenoma?
What is a common long-term consequence of Sheehan Syndrome in regards to the pituitary gland's appearance on MRI?
What is a common long-term consequence of Sheehan Syndrome in regards to the pituitary gland's appearance on MRI?
In which situation should patients be emergency-tested and treated concerning cortisol deficiency?
In which situation should patients be emergency-tested and treated concerning cortisol deficiency?
What is typically not a necessary follow-up procedure in evaluating Empty Sella Syndrome?
What is typically not a necessary follow-up procedure in evaluating Empty Sella Syndrome?
Which of the following statements about hypopituitarism is incorrect?
Which of the following statements about hypopituitarism is incorrect?
What is the recommended interval for follow-up MRI if no growth is noted after the first 6-12 month assessment for a macroadenoma?
What is the recommended interval for follow-up MRI if no growth is noted after the first 6-12 month assessment for a macroadenoma?
Which condition results from the herniation of arachnoid into the sella turcica, causing pressure on the pituitary gland?
Which condition results from the herniation of arachnoid into the sella turcica, causing pressure on the pituitary gland?
What is the incidence of Sheehan Syndrome globally?
What is the incidence of Sheehan Syndrome globally?
Which hormonal deficiency is most commonly associated with Sheehan Syndrome?
Which hormonal deficiency is most commonly associated with Sheehan Syndrome?
What is the primary cause of pituitary gland necrosis in Sheehan Syndrome?
What is the primary cause of pituitary gland necrosis in Sheehan Syndrome?
What physiological change during pregnancy increases the pituitary gland's vulnerability to ischemic injury?
What physiological change during pregnancy increases the pituitary gland's vulnerability to ischemic injury?
What is a potential pathology associated with the growth of a null cell pituitary adenoma?
What is a potential pathology associated with the growth of a null cell pituitary adenoma?
What is the most appropriate strategy for management of an incidental microadenoma if it is not causing symptoms or hormone secretion?
What is the most appropriate strategy for management of an incidental microadenoma if it is not causing symptoms or hormone secretion?
What is the primary consequence of a pituitary adenoma on hormone secretion?
What is the primary consequence of a pituitary adenoma on hormone secretion?
Which clinical manifestation is commonly associated with the mass effect of a pituitary tumor?
Which clinical manifestation is commonly associated with the mass effect of a pituitary tumor?
Which type of hormone is synthesized by the posterior pituitary gland?
Which type of hormone is synthesized by the posterior pituitary gland?
What is the typical progression of symptoms in patients with prolactinoma?
What is the typical progression of symptoms in patients with prolactinoma?
Which tumor type is presented as a benign growth from embryonic pituitary tissue, aside from adenomas?
Which tumor type is presented as a benign growth from embryonic pituitary tissue, aside from adenomas?
In the context of pituitary apoplexy, what primarily causes serious complications?
In the context of pituitary apoplexy, what primarily causes serious complications?
What condition is characterized by excessive secretion of growth hormone, leading to abnormal growth?
What condition is characterized by excessive secretion of growth hormone, leading to abnormal growth?
In terms of epidemiology, what is the prevalence of pituitary adenomas in the general population?
In terms of epidemiology, what is the prevalence of pituitary adenomas in the general population?
Which term describes a pituitary mass that is found incidentally and is asymptomatic?
Which term describes a pituitary mass that is found incidentally and is asymptomatic?
What is a potential effect of elevated adrenocorticotropic hormone (ACTH) from an ACTH-secreting pituitary adenoma?
What is a potential effect of elevated adrenocorticotropic hormone (ACTH) from an ACTH-secreting pituitary adenoma?
What demographic shows the highest incidence of Type 1 diabetes (T1D) according to epidemiological trends?
What demographic shows the highest incidence of Type 1 diabetes (T1D) according to epidemiological trends?
Which symptom is most indicative of Type 1 diabetes in the clinical presentation described?
Which symptom is most indicative of Type 1 diabetes in the clinical presentation described?
What mechanism is theorized to increase the susceptibility of pancreatic β cells to autoimmune attacks in Vitamin D deficiency?
What mechanism is theorized to increase the susceptibility of pancreatic β cells to autoimmune attacks in Vitamin D deficiency?
At what peak age range is Type 1 diabetes most commonly diagnosed?
At what peak age range is Type 1 diabetes most commonly diagnosed?
Which factor is NOT commonly associated with the epidemiology of Type 1 diabetes?
Which factor is NOT commonly associated with the epidemiology of Type 1 diabetes?
What fasting plasma glucose level is indicative of a positive diabetes test result?
What fasting plasma glucose level is indicative of a positive diabetes test result?
What is the benefit of using continuous glucose monitoring (CGM) compared to self-monitoring of blood glucose (SMBG)?
What is the benefit of using continuous glucose monitoring (CGM) compared to self-monitoring of blood glucose (SMBG)?
Which of the following conditions can indicate low endogenous insulin activity?
Which of the following conditions can indicate low endogenous insulin activity?
How can a reduction in A1C levels to below 7% affect diabetes complications?
How can a reduction in A1C levels to below 7% affect diabetes complications?
What is the recommended blood glucose target range for self-monitoring in diabetes management?
What is the recommended blood glucose target range for self-monitoring in diabetes management?
Which of the following antibodies can indicate autoimmune type 1 diabetes?
Which of the following antibodies can indicate autoimmune type 1 diabetes?
What aspect of C-Peptide testing is crucial for determining diabetes progression?
What aspect of C-Peptide testing is crucial for determining diabetes progression?
Which factor is NOT considered a diagnostic criterion for diabetes?
Which factor is NOT considered a diagnostic criterion for diabetes?
What is the recommended target for fasting plasma glucose (FPG) levels in pregnant patients to minimize complications?
What is the recommended target for fasting plasma glucose (FPG) levels in pregnant patients to minimize complications?
Which of the following treatments is most appropriate for patients with a GFR less than 30?
Which of the following treatments is most appropriate for patients with a GFR less than 30?
Which screening test is NOT recommended for evaluating distal symmetric polyneuropathy (DPN) in patients with diabetes?
Which screening test is NOT recommended for evaluating distal symmetric polyneuropathy (DPN) in patients with diabetes?
What is a consequence of neuropathy combined with poor perfusion due to atherosclerosis?
What is a consequence of neuropathy combined with poor perfusion due to atherosclerosis?
Which of the following medications may help improve sensation in patients with neuropathy?
Which of the following medications may help improve sensation in patients with neuropathy?
What is the recommended frequency for patients with T1D to be seen for appointments?
What is the recommended frequency for patients with T1D to be seen for appointments?
Which quick carbohydrate can be effectively used to raise blood sugar levels in an emergency situation?
Which quick carbohydrate can be effectively used to raise blood sugar levels in an emergency situation?
Which of the following is NOT a common sign or symptom of hyperglycemia?
Which of the following is NOT a common sign or symptom of hyperglycemia?
What can happen if a patient takes a 'slow' carbohydrate before consuming a 'quick' carbohydrate?
What can happen if a patient takes a 'slow' carbohydrate before consuming a 'quick' carbohydrate?
What is the appropriate strategy for insulin dosing when blood glucose is above 250 mg/dL?
What is the appropriate strategy for insulin dosing when blood glucose is above 250 mg/dL?
When administering a glucagon injection for severe hypoglycemia, what is a critical consideration?
When administering a glucagon injection for severe hypoglycemia, what is a critical consideration?
What does the correction factor (CF) formula for insulin dosing derive from?
What does the correction factor (CF) formula for insulin dosing derive from?
What is a significant risk if too much quick carbohydrate is consumed too rapidly?
What is a significant risk if too much quick carbohydrate is consumed too rapidly?
Which of the following describes the biochemical process leading to the accumulation of free fatty acids in DKA?
Which of the following describes the biochemical process leading to the accumulation of free fatty acids in DKA?
What is the primary mechanism of action of SGLT1/2 inhibitors in diabetes management?
What is the primary mechanism of action of SGLT1/2 inhibitors in diabetes management?
Which symptom is commonly associated with Diabetic Ketoacidosis (DKA)?
Which symptom is commonly associated with Diabetic Ketoacidosis (DKA)?
Which medication is specifically indicated as adjunctive therapy to insulin for post-prandial glucose control?
Which medication is specifically indicated as adjunctive therapy to insulin for post-prandial glucose control?
What potential adverse effect is associated with SGLT1/2 inhibitors in the Type 1 Diabetes population?
What potential adverse effect is associated with SGLT1/2 inhibitors in the Type 1 Diabetes population?
For a patient requiring more than 200 units of insulin daily, which strategy is recommended?
For a patient requiring more than 200 units of insulin daily, which strategy is recommended?
In the case of DKA, what initial treatment is primarily administered to address dehydration?
In the case of DKA, what initial treatment is primarily administered to address dehydration?
What is the primary reason for lowering mealtime insulin dosing when using synthetic amylin like Pramlintide?
What is the primary reason for lowering mealtime insulin dosing when using synthetic amylin like Pramlintide?
What is the target fasting plasma glucose (FPG) level in pregnant women to reduce the risk of pre/postnatal complications?
What is the target fasting plasma glucose (FPG) level in pregnant women to reduce the risk of pre/postnatal complications?
Which is an essential yearly assessment for managing renal complications in pregnant patients with diabetes?
Which is an essential yearly assessment for managing renal complications in pregnant patients with diabetes?
What is the most effective method to screen patients for distal symmetric polyneuropathy (DPN)?
What is the most effective method to screen patients for distal symmetric polyneuropathy (DPN)?
Which medication may help improve sensation in patients with neuropathy due to diabetes?
Which medication may help improve sensation in patients with neuropathy due to diabetes?
What condition can result from neuropathy combined with poor perfusion due to atherosclerosis in diabetic patients?
What condition can result from neuropathy combined with poor perfusion due to atherosclerosis in diabetic patients?
What action should you take when treating hyperglycemia with blood glucose greater than 250 mg/dL?
What action should you take when treating hyperglycemia with blood glucose greater than 250 mg/dL?
Which of the following is NOT a correct treatment for severe hypoglycemia?
Which of the following is NOT a correct treatment for severe hypoglycemia?
For the patient with T1D who presents with symptoms of acute sinusitis, what injection might another patient have received to feel better quickly?
For the patient with T1D who presents with symptoms of acute sinusitis, what injection might another patient have received to feel better quickly?
Which of the following symptoms is NOT characteristic of hyperglycemia?
Which of the following symptoms is NOT characteristic of hyperglycemia?
How would you calculate the correction factor (CF) for insulin dosing?
How would you calculate the correction factor (CF) for insulin dosing?
What should you do to immediately help lower blood glucose levels during an episode of hyperglycemia?
What should you do to immediately help lower blood glucose levels during an episode of hyperglycemia?
What common mistake should be avoided when administering quick carbohydrates?
What common mistake should be avoided when administering quick carbohydrates?
What is a key consideration when treating a patient with untreated hyperglycemia?
What is a key consideration when treating a patient with untreated hyperglycemia?
Which newly introduced insulin has the shortest half-life?
Which newly introduced insulin has the shortest half-life?
What is a critical requirement for the use of Teplizumab in delaying Type 1 Diabetes onset?
What is a critical requirement for the use of Teplizumab in delaying Type 1 Diabetes onset?
Which two medications are currently being studied for their potential application in Type 1 Diabetes management?
Which two medications are currently being studied for their potential application in Type 1 Diabetes management?
What ongoing management requirement is listed for individuals with Type 1 Diabetes?
What ongoing management requirement is listed for individuals with Type 1 Diabetes?
What is the primary reason for the accumulation of free fatty acids during Diabetic Ketoacidosis?
What is the primary reason for the accumulation of free fatty acids during Diabetic Ketoacidosis?
Which of the following symptoms is NOT typically associated with Diabetic Ketoacidosis?
Which of the following symptoms is NOT typically associated with Diabetic Ketoacidosis?
What critical supply is mentioned as necessary for individuals managing hypoglycemia?
What critical supply is mentioned as necessary for individuals managing hypoglycemia?
What is the route of administration for the medication Amylin (Symlin)?
What is the route of administration for the medication Amylin (Symlin)?
What is a common adverse effect of SGLT1/2 inhibitors in Type 1 Diabetes patients?
What is a common adverse effect of SGLT1/2 inhibitors in Type 1 Diabetes patients?
What is the initial treatment recommendation for a patient experiencing Diabetic Ketoacidosis?
What is the initial treatment recommendation for a patient experiencing Diabetic Ketoacidosis?
In which situation would a patient most likely require a higher dose of insulin?
In which situation would a patient most likely require a higher dose of insulin?
What is the main function of synthetic Amylin in diabetes management?
What is the main function of synthetic Amylin in diabetes management?
What potential condition can occur as a side effect of SGLT1/2 inhibitors?
What potential condition can occur as a side effect of SGLT1/2 inhibitors?
What is the A1C level that confirms a diabetes diagnosis?
What is the A1C level that confirms a diabetes diagnosis?
Which method is recommended for self-monitoring blood glucose levels?
Which method is recommended for self-monitoring blood glucose levels?
What is the primary purpose of measuring C-Peptide levels in diabetes diagnostics?
What is the primary purpose of measuring C-Peptide levels in diabetes diagnostics?
What is the target blood glucose level for most patients during self-monitoring?
What is the target blood glucose level for most patients during self-monitoring?
What is a potential disadvantage of Continuous Glucose Monitoring (CGM)?
What is a potential disadvantage of Continuous Glucose Monitoring (CGM)?
Which of the following tests is NOT a criterion for diagnosing diabetes?
Which of the following tests is NOT a criterion for diagnosing diabetes?
What is the recommended change interval for continuous glucose monitors?
What is the recommended change interval for continuous glucose monitors?
Which is a consequence of maintaining an A1C level below 7%?
Which is a consequence of maintaining an A1C level below 7%?
Flashcards are hidden until you start studying
Study Notes
Acromegaly
- Occurs from hypersecretion of growth hormone (GH)
- Annual Incidence: 10/1 million people
- Average age of diagnosis: 40 to 45
- Diagnosed late due to its gradual onset
- Gigantism: GH excess before fusion of epiphyseal growth plates in children/adolescents
Acromegaly Etiology
- Most common cause: Pituitary adenoma
- Somatotroph (GH-secreting) adenoma
- Represents approximately 1/3 of all hormone-secreting pituitary adenomas
- Somatotroph (GH-secreting) adenoma
Acromegaly Complications
-
Metabolic
- Hyperinsulinism
- Insulin resistance in 50% of patients, leading to Type 2 Diabetes Mellitus (T2DM)
- Hypertriglyceridemia
- Hypercalciuria
- Hyperphosphatemia (70%): Direct stimulation of renal tubular phosphate reabsorption
-
Visceral Organ Enlargement:
- Thyroid enlargement may be diffuse or multinodular
-
Cardiovascular Disease:
- Hypertension (50% of patients)
- Left ventricular hypertrophy & cardiomyopathy
- Valvular disease
- Arrhythmia
- Death from acromegaly is primarily due to cardiovascular disease
-
Obstructive Sleep Apnea
-
Increased Risk of Colonic Neoplasia
- Possible association with acromegaly
- Increased risk of adenomatous colonic polyps
- Increased prevalence of colorectal cancer
Osmosis
- Movement of fluid across a permeable membrane
- Fluid flows from areas of high water concentration to low water concentration
- This process results in equalized concentrations on either side of the membrane
Osmosis Definitions
- Solute: Dissolved substance in a solution (usually salt)
- Solvent: Liquid in which a solute is dissolved (usually water)
- Osmolality: Measurement of solute concentration per volume of solvent
- Tonicity: Measurement of osmotic pressure between two solutions
Types of IV Fluids
- Isotonic: 0.9% NaCl in H2O
- Does not promote osmosis
- Increases extracellular volume only
- Increases circulating volume without changing concentration
- Hypotonic: 0.45% NS (1/2 NS)
- Low sodium (solute) and high fluid (solvent)
- Promotes osmosis of extracellular fluid into cells
- Used to correct cellular dehydration, such as chronic hypernatremia or diabetic ketoacidosis (DKA)
- Hypertonic: 3% NS
- High sodium (solute) and low fluid (solvent)
- Promotes osmosis of fluid out of cells and into the extracellular space
- Used to correct sodium and circulating water deficits, such as severe hyponatremia or hypovolemia
Antidiuretic Hormone (ADH)
- Also known as vasopressin
- Promotes water retention
- Vasoconstriction increases blood pressure
- Synthesized by the paraventricular and supraoptic nuclei of the hypothalamus
- Released in response to hyperosmolality and/or hypovolemia
- Released from the posterior pituitary, enters the bloodstream, and travels to the renal tubule
Effects of ADH (Vasopressin)
Diabetes Insipidus
- Disorder of salt and water metabolism
- Pathophysiology: Inability to concentrate urine in the kidneys
- Causes excessive water loss, leading to increased plasma sodium concentration (hypernatremia)
- Increased sodium creates a hyperosmotic state, which can cause:
- Neuronal shrinkage from cellular dehydration and permanent damage
- Hypernatremia is defined as sodium greater than 145 mEq/L
- Increased water loss decreases intravascular volume (hypovolemia), which can cause circulation problems
Types of Diabetes Insipidus
- Central Diabetes Insipidus: Disease due to ADH insufficiency
- Nephrogenic Diabetes Insipidus: Condition in which the renal tubules fail to respond to normal levels of ADH
Central Diabetes Insipidus
- Disease due to insufficiency of ADH (arginine vasopressin)
- Etiology:
- Approximately 50% of cases are idiopathic
- Injury to the hypothalamic-pituitary area can result from:
- Trauma
- Tumor
- Neurologic procedures
- Less common causes: Sarcoidosis, syphilis, encephalitis, infiltrative diseases (such as Langerhans cell histiocytosis), Hand-Schuller-Christian Disease
Nephrogenic Diabetes Insipidis
- Renal tubules fail to respond to normal circulating levels of ADH
- Can occur in infancy and can be primary or secondary
- Due to conditions like chronic renal disease, sickle cell anemia, amyloidosis, hypokalemia, hypercalcemia, or use of certain medications (lithium, demeclocycline, cidofovir, foscarnet, orlistat, amphotericin B)
Diabetes Insipidus Presentation
- Polyuria:
- In the absence of ADH, the kidneys are unable to reabsorb free water
- Loss of the ability to concentrate urine (dilute urine)
- Large volumes of dilute urine (3-5 liters per day)
- Nocturia
- Polydipsia: Thirst results, leading to increased fluid intake
- Altered mental status
- Visual field defects
Diabetes Insipidus Diagnostic Testing
- Lab Tests:
- CMP (Complete Metabolic Panel): Sodium, calcium, potassium, BUN (Blood Urea Nitrogen), glucose
- Urine Dipstick: Specific gravity and glucose
- 24-hour urine for volume and osmolality
- Imaging:
- Pituitary MRI (Magnetic Resonance Imaging) or CT (Computed Tomography)
Diabetes Insipidus Laboratory Findings
- 24-hour urine volume greater than 40 mL/kg body weight
- Dilute urine: Urine osmolality will be low
Waist Circumference & Adipose Tissue
- Varying distribution of adipose tissue (subcutaneous vs. visceral) at the same waist circumference can lead to different health risks.
Metabolic Syndrome - Prevalence
- Prevalence in the US is 34.7%.
- Prevalence increases with age:
- 21.3% at ages 20-39 years
- 48.6% at ages over 60 years
- Prevalence is generally equal in women and men.
- Varies across different populations.
Metabolic Syndrome - Etiology
- Insulin resistance: most widely accepted explanation for the pathophysiology of metabolic syndrome.
- Obesity epidemic:
- Over-nutrition
- Atherogenic diet (high in fats, sugars, and salt)
- Sedentary lifestyles
- Genetic contributions.
- Polycystic Ovarian Syndrome (PCOS): shares many characteristic features with metabolic syndrome.
Metabolic Syndrome - Principles
- Increased overweight/obese population leads to higher incidence of metabolic syndrome.
- No single, common cause identified.
- Reflects sedentary lifestyle and over-nutrition, contributing to excess adiposity in modern society.
- Endothelial dysfunction and atherosclerosis increase the risk of cardiovascular disease (CVD) and Type II Diabetes.
- Diagnosing metabolic syndrome identifies individuals at high risk for CVD and diabetes.
Metabolic Syndrome - History & Physical Examination
- Past medical history:
- Type II Diabetes, hypertension, hyperlipidemia, insulin resistance, HIV infection.
- Medications: glucocorticoids, antipsychotics, anti-viral drugs for HIV.
- Family history:
- CVD, type II DM, hyperlipidemia, obesity, PCOS.
- Social history:
- Low exercise levels, high-calorie consumption, alcohol intake, smoking.
- Physical examination:
- Symptoms: Polyuria, polydipsia, weight loss, angina, PCOS, obstructive sleep apnea.
- Blood pressure, body mass index (BMI), waist and hip circumference, waist-to-hip ratio.
- Examination of cardiovascular system, respiratory system, and abdomen.
- Signs: Corneal arcus, xanthelasma, hepatomegaly, hirsutism, acne, acanthosis nigricans.
Corneal Arcus & Xanthelasma
- Corneal arcus: caused by lipid deposits.
- Xanthelasma: Multiple creamy-orange, slightly elevated dermal papules on the eyelids, even in individuals with normal lipid levels.
Acanthosis Nigricans & Skin Tags
- Acanthosis nigricans: dark, velvety thickening of the skin, often in skin folds.
- Skin Tags: multiple small, pedunculated acrochordons (skin tags) in the neck crease.
Obesity - Evaluation
- Initial workup:
- Measurements:
- Blood pressure
- Weight and height to calculate BMI
- Waist circumference
- Labs:
- Thyroid stimulating hormone (TSH) and free T4
- Fasting lipid panel
- Fasting glucose
- Measurements:
Obesity - Differential Diagnosis
- Increased caloric intake (due to life changes)
- Fluid retention (heart failure, cirrhosis, renal failure)
- Hypothyroidism
- Type 2 Diabetes
- Medications (antipsychotics, antidepressants, corticosteroids)
- Insulinoma (tumor of the pancreas)
- Binge eating disorder
Obesity Treatment - Primary Approach
- If no underlying medical condition:
- Diet and exercise
- Diet and exercise
- Diet and exercise
- Goal:
- Decrease in 10% body weight over 6 months, or 1-2 lbs per week.
- Example: 15 lbs off 150 lbs, 20 lbs off 200 lbs, 30 lbs off 300 lbs.
- Reassess treatment plan after 6 months.
- To achieve weight loss, caloric expenditure must exceed caloric intake.
Obesity Treatment - Caloric Intake Recommendations
- Guidelines from the American Heart Association/American College of Cardiology/The Obesity Society (AHA/ACC/TOS):
- Produce a 500-750 kcal/day deficit from the habitual diet, or:
- Consume 1200-1700 kcal/day for women.
- Consume 1500-1800 kcal/day for men.
- Adjust calorie consumption based on individual body weight.
- Produce a 500-750 kcal/day deficit from the habitual diet, or:
Fast Food Calorie Content
- McDonalds Big Mac Meal: 1320 calories
- Burger King Whopper Meal: 1430 calories
- KFC 4 piece Chicken Meal: 1690 calories
Weight Loss Diets
- No single diet stands out as superior for long-term weight loss (over 1 year).
- The Mediterranean diet has shown benefits in reducing the risk of atherosclerotic cardiovascular disease (ASCVD).
- Low-carbohydrate/high-protein diets often result in greater weight loss in the first 6 months.
- Challenges for dietary studies include inconsistency and inaccuracy in adherence to diet plans and calorie intake reporting by patients.
Obesity Treatment - Exercise
- Combining dietary modification with exercise is the most effective behavioral approach for obesity treatment.
- Exercise alone is generally not effective for sustained weight loss (over 1 year).
Physical Activity Guidelines
- The 2008 Physical Activity Guidelines for Americans recommend that adults engage in:
- 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity aerobic physical activity per week.
- Performed in episodes of at least 10 minutes, preferably spread throughout the week.
Incorporating Exercise into Daily Life
- Focus on simple ways to increase physical activity:
- Brisk walking
- Using stairs
- Doing housework and yard work
- Participating in sports
- Wear a pedometer or accelerometer to monitor steps or calories burned.
- Step counts correlate strongly with activity levels.
Obesity Treatment - Adjunctive Behavioral Therapy
- Cognitive behavioral therapy strategies help change and reinforce new dietary and physical activity behaviors:
- Self-monitoring techniques (journaling, weighing and measuring food and activity)
- Stress management
- Stimulus control (smaller plates, not eating in front of the TV or in the car)
- Social support
- Problem solving
- Cognitive restructuring for positive and realistic self-perception.
- Before recommending any behavioral change, inquire about the "what, when, where, and how" of the change to ensure successful implementation.
Obesity Treatment - Adjunctive Pharmacological Therapy
- Consider pharmacological therapy for patients with:
- BMI ≥ 30 kg/m2
- BMI ≥ 27 kg/m2 with obesity-related diseases where dietary and exercise therapy has been unsuccessful.
Pharmacologic Options
- Gastrointestinal fat blockers: Orlistat (Xenical, Alli)
- Dosage: 120 mg PO tid with meals
- Potential weight loss: 5% body weight
- Mechanism of action: reduces fat absorption in the gastrointestinal tract.
- Side effects: GI distress (diarrhea, cramping, flatulence). A low-fat diet can reduce side effects and motivate patients to adhere to dietary recommendations.
- Appetite suppressants (anorexiants):
- Lorcaserin (Belviq)
- Dosage: 10 mg PO bid
- Potential weight loss: 5% body weight.
- Phentermine + topiramate
- Naltrexone + bupropion
- Liraglutide (Saxenda, Victoza)
- Lorcaserin (Belviq)
Obesity - Summary
- Achieving weight loss requires caloric expenditure exceeding caloric intake.
- Maintaining weight loss is challenging and requires permanent behavior modification in diet and exercise.
Hirsutism (Excessive Hair Growth)
- Hirsutism is excessive male-pattern hair growth in women of reproductive age.
- Affects 5-10% of females of reproductive age.
- Most common cause: Polycystic Ovarian Syndrome (PCOS).
Hirsutism - Definition
- Clinical presentation: Course, pigmented hair growth on the face, chest, abdomen, back in a female.
Hirsutism - Epidemiology
- 20% of American women experience hirsutism.
- 80% of women with androgen excess have hirsutism, but not all women with hirsutism have androgen excess.
- Extent of hair growth varies by ethnicity:
- East Asian and Native American women tend to have less body hair
- Southern European women (Mediterranean) tend to have more body hair.
- Hirsutism can occur with virilization (signs of masculinization):
- Male pattern alopecia (hair loss), voice deepening, increased muscle bulk, clitoromegaly.
- Virilization indicates moderate to severe androgen excess.
Hirsutism - Etiology
- Idiopathic hirsutism:
- Women with hirsutism but normal androgen concentrations.
- No menstrual irregularities.
- No identifiable cause for the hirsutism.
- Androgens & Androgen action:
- Hirsutism results from the interaction of circulating serum androgens and the sensitivity of hair follicles to those androgens, as well as local growth factors.
Androgens
- Testosterone: primarily from ovarian origin.
- Dehydroepiandrosterone sulfate (DHEAS): predominantly from adrenal gland origin.
- Androstenedione: produced by the adrenal gland or ovaries.
Androgens & Hair Growth
- Scalp, eyebrow, and eyelash hair growth occurs independently of androgens.
- At other body sites (face, armpits, pubic area, arms, legs, trunk, and ears), androgens increase hair growth.
- Androgen excess in females leads to increased hair growth in the most androgen-sensitive areas (upper lip, chin, midsternal area, upper abdomen, back, and buttocks).
- Paradoxically, this can lead to scalp hair loss due to the increased time that hairs spend in the anagen phase (growth phase).
Hirsutism - Evaluation
- Initial workup:
- History:
- Menstrual cycle regularity
- Galactorrhea (breast milk production)
- Family history of hirsutism, PCOS, or endocrine disorders
- Medication history (include steroids and androgenic medications)
- Physical examination:
- Assess hair growth pattern
- Vital signs
- Signs of virilization (clitoromegaly, voice deepening, increased muscle mass)
- Signs of Cushing syndrome (round face, buffalo hump, striae)
- Signs of hypothyroidism (weight gain, fatigue, constipation, cold intolerance)
- Labs:
- Serum free testosterone
- Serum DHEAS
- Serum androstenedione
- Prolactin
- Thyroid-stimulating hormone (TSH) and free T4
- 17-hydroxyprogesterone if adrenal issues are suspected
- 24-hour urinary free cortisol if Cushing syndrome is suspected
- Note: It's important to rule out other causes of hirsutism such as medications, thyroid issues, and Cushing syndrome.
- History:
- Transvaginal Ultrasound: This exam can be used to assess for Polycystic Ovarian Morphology (PCOM) and can play a role in the diagnosis of PCOS.
PCOS Diagnostic Evaluation - Transvaginal US
- Transvaginal ultrasound (TVUS) can be used to determine if a woman has Polycystic Ovarian Morphology (PCOM).
- This is not always necessary for the PCOS diagnosis.
- If a woman has both oligomenorrhea (irregular periods) and evidence of hyperandrogenism (excess male hormones), and other causes have been ruled out, she meets the criteria for a PCOS diagnosis, and an ultrasound is not required.
- TVUS is often performed in women with hyperandrogenic symptoms and normal menstrual cycles. This helps to look for PCOM.
Basal Body Temperature Chart (BBT)
- A biphasic pattern on a basal body temperature chart suggests ovulation.
- Refer to the provided image for an example.
Monogenic Diabetes (MODY)
- A group of single gene disorders that affect pancreatic beta cell function
- Often presents before the age of 25
- Most commonly diagnosed in 2-5% of diabetes sufferers
- This is a non-insulin requiring form of diabetes
- Autosomal dominant inheritance, several gene abnormalities on different chromosomes
- Mutations in GCK (glucokinase) & HNF (hepatocyte nuclear factor) genes are most common
- GCK mutations cause mild, stable fasting hyperglycemia without the need for treatment, often manageable with diet
- However, during pregnancy, treatment may be required
- HNF mutations often cause progressive pancreatic beta-cell dysfunction and hyperglycemia that can contribute to microvascular complications. Most patients respond well to Sulfonylureas
- Patients often have mild, stable, fasting hyperglycemia
- They are typically not obese
- Patients may have a family history of diabetes, be insulin independent and lack ketoacidosis when insulin is omitted for up to 5 years following diagnosis
- They do not have autoantibodies for pancreatic antigens
- Patients have evidence of endogenous insulin production
- Insulin resistance is not a feature of MODY
- The presence of autoantibodies is suggestive of an alternative diagnosis
- Diagnosis requires genetic DNA testing
Latent Autoimmune Diabetes in Adults (LADA)
- Slowly developing type I diabetes, often misdiagnosed as type II
- Patients are initially non-insulin dependent and do not experience ketoacidosis
- Insulin dependence develops over time, as beta-cell function declines
- Patients have autoantibodies directed against pancreatic beta cells
- Presents as a slowly progressive form of Type I diabetes
- Accounts for just a small portion of diabetes patients
- Despite the presence of islet autoantibodies at diagnosis, the progression of autoimmune beta-cell failure is slow
- Patients do not require insulin initially, however, within 6 years of diagnosis they will likely require insulin
- LADA often occurs in 10% of those over 35 and 25% of obese individuals with islet antibodies
- LADA can also present in childhood
- Considered a slowly progressive variant of type 1 diabetes
Gestational Diabetes (GDM)
- Occurs during the second or third trimester of pregnancy
- Occurs in patients who were not previously diabetic
- Occurs in approximately 4% of pregnancies
- Screening is performed between 24 and 28 weeks of pregnancy
- Hormones during pregnancy contribute to insulin resistance
- Increased risk of developing preeclampsia, gestational hypertension and polyhydramnios compared to general obstetric population
- Patients with GDM exhibit a higher risk of delivering a stillborn baby
- Associated with high maternal & perinatal morbidity
Risk Factors for Gestational Diabetes
- Family history of diabetes
- Personal history of impaired glucose tolerance
- A HbA1c > 5.7
- Pre-pregnancy BMI > 30
- Significant or rapid weight gain between pregnancies
- Older maternal age (over 40)
GDM Complications
- Increased risk of operative delivery (c-section)
- Large for gestational age infants (LGA), macrosomia and related complications
- Neonatal morbidity
- Hypoglycemia, hyperbilirubinemia, hypocalcemia, hypomagnesemia, polycythemia, respiratory distress, &/or cardiomyopathy
- Delayed pulmonary, hepatic, & neurologic organ maturity
- Congenital defects (heart, neural tube, renal)
- Abnormal fetal heart rate patterns
- Intrauterine fetal growth retardation, & intrauterine fetal distress
- Maternal infections
- Maternal hypoglycemia, diabetic coma, ketoacidosis
- Maternal cardiac, renal , ophthalmic, & peripheral vascular injuries
Long-Term Consequences of GDM
- Increased risk of developing type II diabetes
- Increased risk of diabetes-related vascular disease
- Increased risk of offspring developing obesity, impaired glucose tolerance, & diabetes
GDM Screening
- Initial prenatal visit: Obtain HbA1c as part of the prenatal laboratory studies
- Manage as diabetic if HbA1c is above 6.5%
- At 24-28 weeks of gestation: perform an oral glucose tolerance test (OGTT)
- An initial 50 gram, 1-hour OGTT
- A serum glucose level above 140mg/dL is considered abnormal and progression to a 3-hour OGTT is recommended
- A serum glucose level of 200mg/dL is considered positive for GDM
- If the 1-hour OGTT is abnormal, a 3-hour OGTT should be performed
- Fasting blood sugar is obtained prior to the start of the test
- A 100 gram oral glucose load is administered
- Positive GDM diagnosis if 2 or more of the values obtained during the 3-hour test are abnormal
GDM Management
- Requires a team approach with the patient, obstetrician, maternal-fetal medicine (MFM) specialist, and a nutritionist
- Goal is to achieve euglycemia:
- FBS < 95 mg/dl
- 1 hr PP glucose < 140 mg/dl
- 2 hr PP glucose < 120 mg/dl
GDM Treatment
- Diet adjustments recommended: 30-35 kcal/kg/d
- 3 small to moderate-sized meals with 2 snacks
- Limit carbohydrates to no more than 40% of the diet, ensuring ketosis does not develop
- Recommended dietary breakdown: 40% carbohydrate, 20% protein, 40% fat with a generous amount of fiber
- Encourage mild to moderate aerobic exercise (walking) after meals
- Preventing gestational weight gain is crucial to controlling GDM
- Glucose Monitoring Required: Fasting and 1-2 hours postprandial blood glucose at least 4 times per day
- Insulin is the preferred treatment for patients who are unable to manage GDM with diet and exercise: Combination of short-term (lispro or aspart) pre-meal and intermediate (NPH) insulin is often preferred
- Basal insulin (glargine & detemir) are also safe and effective but need further study.
- Metformin & glyburide are alternative options to Insulin:
- Metformin: Initial 500 mg daily or bid, max 2-2.5 g daily in two divided doses
- Glyburide: 2.5–5 mg PO daily, increase 2.5 mg/wk PRN to Max. 20 mg/day
- Both drugs cross the placenta
Insulin Therapy in GDM
- Starting Insulin Dose 0.7-1.0 U/kg/d (based on the patient's current pregnant weight)
- A combination of intermediate and short-acting insulin is often necessary.
- 2/3 of total insulin dosage is given in the morning before breakfast: 2/3 NPH, 1/3 regular insulin
- 1/3 of total daily dose is given in the evening before dinner: ½ regular insulin, ½ NPH insulin
Diabetes Management in Pregnancy
- Antepartum care:
- Detailed ultrasonic study of the fetus, including an echocardiogram to screen for fetal congenital heart malformations
- Weekly Biophysical Profiles (BPP) beginning at 32-34 weeks of gestational age
- Delivery:
- Spontaneous labor and vaginal delivery at term is preferred if fetal stability is maintained
- Cesarean delivery may be recommended for large fetuses (>4500 g = 10 lbs)
- Intrapartum care:
- Glucose Control: Monitor maternal glucose levels every hour, maintaining maternal euglycemia (80-120 mg/dl) during labor. Continuous IV infusion or PRN SQ doses of regular insulin are given to address elevated glucose levels
- Fetal Monitoring: Continuous electronic fetal heart rate monitoring is recommended
- Postpartum care:
- After delivery of the fetus and placenta, insulin requirements drop sharply.
- Monitor plasma glucose levels QID (FBS and 1 hr postprandial)
- Treat elevated glucose levels with lispro or regular insulin PRN
- Screen for type II DM 6 weeks postpartum with a 2-hour OGTT
- Counseling on the use of ADA diet is recommended
- Estrogen containing OCPs are not recommended for DM with vascular disease
Pituitary Function
- The anterior pituitary gland produces:
- Luteinizing Hormone (LH) & Follicle-Stimulating Hormone (FSH)
- Prolactin
- Thyroid Stimulating Hormone (TSH)
- Adrenocorticotropic Hormone (ACTH)
- Growth Hormone (GH)
- The posterior pituitary gland produces:
- Oxytocin: crucial for childbirth & lactation
- ADH: important for water balance
- Central Diabetes Insipidus and SIADH (Syndrome of inappropriate ADH) occur due to dysfunction in ADH production or regulation
Pituitary Tumors
- Pituitary tumors account for 10% of all intracranial tumors.
- Most pituitary tumors are benign.
- Tumor growth in the sella and suprasellar regions can cause neurological damage.
- Pituitary adenomas: the most common pituitary mass.
- 22% of the population has a pituitary mass, and 16% has a pituitary adenoma.
- Most pituitary masses and adenomas are clinically silent.
Pituitary Adenoma
- Benign tumor of glandular tissue.
- Can cause hypersecretion or hyposecretion of pituitary hormones.
- Epidemiology: 15% of all intracranial neoplasms, prevalence of 80/100,000.
- At autopsy, up to 1/4th of all pituitary glands harbor an unsuspected microadenoma.
Pituitary Mass/Adenoma: Clinical Features
- Asymptomatic/incidentaloma: incidental finding on MRI or CT.
- Neurologic Manifestations (mass effect):
- Headache (common)
- Visual Disturbance (Optic chiasm compression)
- Mental status changes
- CN abnormalities (dural sinus)
- Vomiting
- Papilledema
- Pituitary apoplexy
- Hypersecretion of Hormones:
- Prolactinoma: hypogonadism (oligo/amenorrhea, galactorrhea, infertility, decreased libido).
- GH secreting: Acromegaly, gigantism.
- ACTH secreting: adrenal hyperplasia → Cushingoid features (weight gain, hirsutism, amenorrhea, decreased libido, unexplained osteopenia).
- TSH secreting: Goiter, palpitations, tremor etc.
When to Evaluate for Pituitary Mass
- Consider evaluation for pituitary mass when there is:
- Hypersecretion of one or more anterior pituitary hormones
- Hypopituitarism (slow onset)
- Vision changes and headache (mass effect)
- Complex hormonal excess and/or deficiencies
Pituitary Mass Evaluation
- Laboratory Evaluation:
- Labs chosen based on symptoms of hormonal excess or insufficiency.
- Consider: CBC, UA, ESR, CRP, Serum Na, Alpha-fetoprotein & HCG, Auto-antibodies, Surgical Bx
- Imaging:
- MRI: T1 weighted with & without gadolinium is the gold standard.
- Skull radiograph: may show enlargement or distortion of the sella if tumors > 10 mm in diameter.
- CT: may show some macroadenomas.
Pituitary Adenoma Treatment
-
Three primary goals:
- Reducing hormone hypersecretion and its clinical manifestations
- Decreasing tumor size to improve symptoms of mass effect
- Correcting hormone deficiencies
-
Prolactinoma:
- Diagnosis: Basal prolactin level of > 200 ng/mL & brain MRI
- Medical Treatment: Dopamine agonists (bromocriptine & cabergoline) decrease prolactin levels.
-
GH & ACTH secreting tumors: Medical management is less effective than for prolactinomas. Surgery is often preferred.
-
Surgery:
- Transsphenoidal approach is preferred.
- Transfrontal Resection may be necessary for tumors with optic chiasm compression or those extending beyond the sella turcica.
-
Radiation Therapy: Used alone or with surgery to decrease tumor size and hormone production.
Management of Incidental Pituitary Adenoma
- When a pituitary mass is found incidentally, investigate its cause.
- If there is no mass effect on MRI and the tumor is not secreting excess hormone:
- Repeat MRI in 6 months for macroadenoma and 12 months for microadenoma to assess for growth.
- If no growth, repeat MRI every 1-2 years for 3 years then intermittently.
- Biochemical testing: not recommended unless the tumor enlarges, or the patient develops symptoms.
Hypopituitarism
- Conditions that can cause hypopituitarism:
- Null cell pituitary adenoma: destruction of normal gland by tumor growth.
- Sheehan Syndrome.
- Empty Sella Syndrome: incompetent diaphragm sella allowing CSF herniation.
- Pituitary Apoplexy.
- Other: surgery, radiation, inflammation, DIC, sickle cell, necrosis from increased ICP.
Sheehan's Syndrome
- Infaction of the anterior pituitary gland during childbirth leading to pituitary necrosis and hypopituitarism.
- Caused by maternal hemorrhage and hypotension resulting in hypoperfusion.
- Incidence: improved due to better delivery and postpartum care.
- Rare in industrialized nations but occurs in about 1/100,000 live births globally.
Sheehan's Syndrome Pathophysiology
- Pregnancy causes the pituitary gland to increase in size and prolactin-secreting cells, but blood supply doesn't increase.
- Hypotension during childbirth can compromise blood flow to the anterior pituitary, leading to infarction and hypopituitarism.
Sheehan's Syndrome Clinical Features
- Loss of all pituitary hormones: 56%.
- Selective loss of pituitary hormones: 44% (GH deficiency is the most common).
- Symptoms: lethargy, anorexia, weight loss, inability to lactate due to prolactin deficiency.
- Treatment: lifelong hormonal replacement.
Empty Sella Syndrome
- Diagnosed when the normal pituitary gland is not seen or is excessively small on MRI.
- Radiologic finding without a distinct clinical condition.
- Causes: increased CSF in the sella, previous surgery, radiation, infarction, congenital.
- Evaluation: to determine if there is a cause or if the patient has signs of pituitary hormone deficiency.
Pituitary Apoplexy
- Acute hemorrhage into the pituitary gland, often at the site of a pre-existing adenoma.
- Can cause acute pituitary hormone deficiency or mass effect.
- Symptoms: severe headache, visual loss, diplopia, hypopituitarism.
Vitamin D Deficiency
- May involve increased gut permeability through gut flora modification
- Theorists believe inadequate vitamin D levels leave pancreatic β cells more susceptible to autoimmune attack
T1D Epidemiology
- Can be diagnosed at any age and in people of every race, shape, and size
- Peak incidence in 5-7 year olds and puberty
- Equal among males and females
- Highest incidence in Finland (overwhelmingly)
- 65 new cases per 100,000 children aged <20 per year, while Sweden, at 2nd, comes in at 30 per 100,000
Clinical Scenario
- 9 year old boy presents with polyuria, polydipsia, and unintentional weight loss despite increased appetite for 3-6 months
- Mother confirms history and admits to a subtle change in mood and energy, and a worsening over the past couple of weeks
- RPG = 450 mg/dL, A1C = 9%
T1D Diagnostics
- Diagnostic criteria includes A1c, FPG, RPG, antibodies, and C-peptide
- Antibody testing includes IAA, GADA, ZnT8A, ICA, etc.
- C-peptide levels determine the level of endogenous insulin levels/activity or disease progression
Self Monitoring of Blood Glucose (SMBG)
- Uses a small blood sample via finger prick to test serum glucose levels
- Tests glucose to see if insulin doses are keeping patients in target
- Target range is 80-120 mg/dL
- Frequency: 3 to 4 times daily
- Brands: One Touch, Freestyle, Contour, Accu-Check
Continuous Glucose Monitoring (CGM)
- Sensor with an electrode placed SQ measures glucose in interstitial fluid with readings every 5 minutes
- Pros: More readings and trends, less finger sticks, alarms for lows/highs
- Cons: Expense, +/- delay in BG’s in real time
- Change sensor: ~ 10 days depending on brand
- Brands: Dexcom, Medtronic, Freestyle
Glycemic Goals
- A1c < 7% decreases microvascular complications and, if implemented soon after dx, is associated with a reduction in macrovascular disease
- Patients with T1D are usually seen every 3-6 months depending on A1c and change in treatment
"Quick" Carbs
- Simple carb that is readily available to get in the bloodstream
- Examples: 4 oz juice or regular soda, 1 juice box, 4 glucose tabs, 1 gummy pack, 1 glucose gel pack, 1 tablespoon honey or sugar
Hyperglycemia
- High blood glucose > 150 mg/dL
- Signs/Symptoms: Polyuria, polydipsia, polyphagia, blurry vision, fatigue
- Causes: Miscalculation of insulin dose, missing a dose/non-compliance, stress, illness, age/hormones
- Treatment: Correction Factor (CF) = 1800/TDD, then (BG – target)/CF for the number of units given for correction dose
Inpatient Hyperglycemia Setting
- Example of order set for inpatient setting for treatment of hyperglycemia
- Ere on the side of caution to prevent hypoglycemia
- Time and fluids are key
Diabetic Ketoacidosis (DKA)
- Blood turning acidic due to dehydration and high blood glucose
- Signs/Symptoms: Fruity breath, Kussmaul’s respirations, weakness, n/v, abdominal pain, fatigue, extreme dehydration
- Causes: Pump malfunction/occlusion, non-compliance, comorbidities, sickness, undiagnosed T1D
- Treatment: Fluids (1L of 0.9% NS per hour initially) + insulin drip (0.1 U/kg/hr) +/- potassium
Amylin
- Symlin© (Pramlintide)
- Synthetic Amylin hormone produced by pancreatic β-cells
- Adjunctive therapy to insulin for post-prandial glucose control
- Injectable pen device, starting dose of 15 mcg (up to 120 mcg) with each meal of at least 30g carbs or 250 calories
SGLT1/2 Inhibitors
- Farxiga© (Dapagliflozin), Jardiance© (Empagliflozin), Zynquista© (Sotagliflozin)
- SGLT1 inhibitor that inhibits the reabsorption of glucose in the kidneys
- Adjunctive therapy to insulin for A1C and FPG/RPG reduction
- 1 pill PO daily in different dosage forms
Insulin for Special Populations
- Insulin Resistant: Use insulin with higher potency/concentration (i.e., Humalin R U-500 vial, Tresiba U-200 pen)
- Pregnancy: Tighter control is needed to prevent pre/postnatal complications, general goals = FPG’s < 90 mg/dL, PPG’s < 120 mg/dL
Diabetic Nephropathy
- Microalbuminuria (30-300 μg/min or >200 μg/min) confirmed on at least 2 occasions 3-6 months apart
- Progressive decline in GFR
- ↑ arterial BP
- Treatment: Yearly measurement of creatinine, urinary albumin excretion, K, consider ACE/ARB, insulin dose adjustments based on GFR & refer to nephrology if GFR < 30
Diabetic Neuropathy
- Stocking-and-glove distribution in distal extremities
- Loss of balance, especially with the eyes closed
- Painless injuries due to loss of sensation
- Test with pinprick, vibration tuning fork, 10-g monofilament, & ankle reflexes
- All pts should be screened for distal symmetric polyneuropathy (DPN) at dx of type 2 and 5 yrs after dx of type 1 and at least yearly thereafter
- Medications: Pregabalin (Lyrica), Gabapentin (Neurontin), TCAs, topical lidocaine or capsaicin
- Neuropathy + poor perfusion → non-healing foot ulcers, amputations, refer to wound care or podiatry
Type 1 Diabetes (T1D) Diagnosing
- A1c > 6.5%
- measured in 3 month increments to reflect RBC life
- Fasting Plasma Glucose (FPG) > 126 mg/dL
- no caloric intake for at least 8 hours
- Random Plasma Glucose (RPG) > 200 mg/dL
- Antibodies present for more than 1
- Insulin autoantibodies (IAA), Glutamic Acid Decarboxylase autoantibodies (GADA), Zinc transporter-8 autoantibodies (ZnT8A), islet cell cytoplasmic autoantibodies (ICA), etc.
- C-peptide < 0.2 nmol/L
- Hyperglycemia in the presence of antibodies
- C-peptide levels determine the level of endogenous insulin levels/activity or disease progression
T1D Monitoring
- Self Monitoring of Blood Glucose (SMBG)
- Small blood sample via finger prick to test serum glucose levels
- Test glucose to see if insulin doses are keeping patients in target
- Target is 80-120 mg/dL
- Check blood glucose 3 to 4 times daily
- Continuous Glucose Monitoring (CGM)
- Sensor with an electrode placed subcutaneously (SQ) measures glucose in the interstitial fluid with readings every 5 minutes
- Pros: More readings and trends, less finger sticks, alarms for low's/high's
- Cons: Expense, +/- delay in BG's in real time
- Change sensor approximately every 10 days depending on brand
T1D Glycemic Goals
- A1c < 7%
- Decreases microvascular complications
- Associated with a reduction in macrovascular disease if implemented soon after diagnosis
- Patients with T1D are usually seen every 3-6 months depending on A1c and change in treatment
- Glucagon injection for severe hypoglycemia
- "Mini" Gluc protocol
“Quick” Carbs
- Simple carbs readily available to get into the bloodstream
- 4 oz. juice or regular soda
- 1 juice box
- 4 glucose tabs
- 1 gummy pack
- 1 glucose gel pack
- 1 tablespoon honey or sugar
- Common Mistakes
- Giving too much too quickly results in rebound hyperglycemia
- Giving a "slow" carb before a "quick" carb
- Quick carb won't absorb and it'll take longer for blood glucose levels to come up (e.g. chocolate milk before juice)
Hyperglycemia
- High blood glucose > 150 mg/dL
- Signs/Symptoms:
- Polyuria, polydipsia, polyphagia, blurry vision, fatigue
- Think of the undiagnosed T1D patient
- Causes:
- Miscalculation of insulin dose, missing a dose/non-compliance, stress, illness, age/hormones
- Treatment:
- Correction Factor (CF)* = 1800/TDD
- Then (BG – target)/CF for number of units given for correction dose
- Example: BG is 250 with a goal of 150 and a weight of 144 lbs, how much insulin to give?
- Wait 1-2 hours before giving another dose and do not give the full dose
- Remember the duration of action (DOA) for rapid acting insulin is 4 hours
- Correction Factor (CF)* = 1800/TDD
- Check for ketones when BG's > 250 mg/dL
- Increase fluid intake to help BG's come down
Inpatient Hyperglycemia Setting
- Example of order set for inpatient setting for treatment of hyperglycemia
- Err on the side of caution to prevent hypoglycemia
- Time and fluids are crucial
Diabetic Ketoacidosis (DKA)
- Blood turning acidic due to dehydration and high blood glucose, creating a harmful environment for the body
- Dehydration + increased blood glucose - insulin (a counter-regulatory hormone) = accumulation of free fatty acids (β-hydroxybutyric acid and acetoacetic acid) which then dissociate to hydrogen ions that bind to bicarb = decreased bicarb and increased anion gap
- Signs/Symptoms:
- Fruity breath/odor, Kussmaul’s Respirations, weakness, n/v, abdominal pain, weakness/fatigue, extreme dehydration
- Causes:
- Pump malfunction/occlusion, non-compliance, comorbidities, sickness, undiagnosed T1D
- Treatment:
- Fluids (1L of 0.9% NS per hour initially) + insulin drip (0.1 U/kg/hr) +/- potassium
- Replace with bicarb?
Other "T1D" Medications
-
Amylin
- Symlin© (Pramlintide)
- Synthetic Amylin, a hormone produced by pancreatic ß-cells
- Adjunctive therapy to insulin for post-prandial glucose control
- Injectable pen device, Starting Dose of 15 mcg (up to 120 mcg) with each meal of at least 30g carbs or 250 calories
- Not used a lot in the US, more so in Europe
- Side effects: Severe hypoglycemia, nausea, vomiting, stomach upset
-
SGLT1/ 2 Inhibitors
- Farxiga© (Dapagliflozin), Jardiance© (Empagliflozin), Zynquista© (Sotagliflozin)*
- SGLT1 inhibitor, which inhibits the reabsorption of glucose in the kidneys
- Adjunctive therapy to insulin for A1C and FPG/RPG reduction
- 1 pill PO daily in different dosage forms
- Not approved yet, but used off-label
- Side effects: Hypotension, Acute Kidney Injury, DKA in the Type 1 Diabetes Population, Yeast Infections, Acute pharyngitis, changes in urinary habits
Insulin for Special Populations
- Insulin Resistant:
- Think of the obese patient requiring more than 200 units daily or more than 100 units per dose
- Use insulin with higher potency/concentration (i.e.Humalin R U-500 vial, Tresiba U-200 pen)
- Pregnancy:
- Tighter control is needed to prevent pre/postnatal complications
- General goals: FPG's < 90 mg/dL, PPG's 300 mg/d or >200 μg/min)
Diabetic Nephropathy
- Causes:
- Persistent hyperglycemia
- Elevated blood pressure
- Diagnosis:
- Albuminuria (>30 mg/d or >200 μg/min) confirmed on at least 2 occasions 3-6 months apart
- Progressive decline in GFR
- ↑arterial BP
- Treatment:
- Yearly measurement of creatinine, urinary albumin excretion, K
- Consider ACE/ARB
- Insulin dose adjustments based on GFR
- Refer to nephrology if GFR < 30
Diabetic Neuropathy
- Stocking-and-glove distribution in distal extremities
- Loss of balance, especially with the eyes closed, and painless injuries due to loss of sensation
- Test with pinprick, vibration tuning fork, 10-g monofilament, & ankle reflexes
- All patients should be screened for distal symmetric polyneuropathy (DPN) at diagnosis of type 2 and 5 years after diagnosis of type 1 and at least yearly thereafter.
- Prevention and regular foot exams are best, but some medications may help sensation:
- Pregabalin (Lyrica)
- Gabapentin (Neurontin)
- TCAs (amitryptilline, nortryptilline, imipramine)
- Topical lidocaine or capsaicin can help
- Neuropathy + poor perfusion (due to atherosclerosis/PAD) → non-healing foot ulcers, amputations
- Refer to wound care or podiatry!
- CHECK YOUR PATIENT'S FEET!
New Insulin & T1D Delay
- 2023 Advanced Technologies and Treatments for Diabetes (ATTD) Conference in Berlin shared information on two new Once Weekly Insulins in studies:
- Icodec (Novo Nordisk, ½ life 7-8 days) and Efsitora (Lilly, ½ life 17 days)
- Demonstrating promise with less hypoglycemia & more TIR
- Studied in Type 2 diabetes
- Teplizumab is FDA approved for delay of T1D Onset:
- First of its kind with more in the pipeline from other companies
- From ProventionBio & Sanofi, Expensive for full course of treatment
- Delays onset for about 2 years
- Must be in “Stage 2” or detectable antibody positive without seroconversion to T1D
- Studying T2DM medications for T1D:
- Metformin and GLP-1 Agonists
- Reduces insulin requirements & decreases hepatic glucose production
- Metformin and GLP-1 Agonists
T1D Supplies
- T1D Medical Alert ID
- Insulin (basal and bolus) through some sort of delivery device
- Needles to deliver the insulin
- +/- skin adhesive for pumps
- Blood glucose monitoring through some sort of device
- +/- testing strips (which are expensive), lacets for the meter, skin adhesives for CGM's
- UTD Glucagon Injection (expires each year)
- Supplies for low's on hand
- Alcohol preps
T1D Follow Up
- Quarterly visits including A1c and neuro/podiatry checks
- Yearly funduscopic exams
- Health plans to attend school
- Extra supplies should pump sites fail or insulin degrades in the hot car
- Extra insulin for when BG's go out of control
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.