Podcast
Questions and Answers
What is the primary reason that acromegaly's physical changes are considered irreversible?
What is the primary reason that acromegaly's physical changes are considered irreversible?
- The body's decreased ability to regenerate tissue in adulthood.
- Growth hormone levels cannot be effectively controlled with current treatments.
- The condition primarily affects older adults.
- The skeletal and soft tissue changes have already occurred. (correct)
Why is early diagnosis of acromegaly often delayed?
Why is early diagnosis of acromegaly often delayed?
- Diagnostic tests for acromegaly are invasive and not routinely performed.
- Initial symptoms are attributed to other endocrine disorders.
- The slow progression of signs and symptoms makes it difficult to identify the onset. (correct)
- Acromegaly primarily affects older adults who are less likely to seek medical attention.
Which feature distinguishes gigantism from acromegaly regarding the pathophysiology of bone growth?
Which feature distinguishes gigantism from acromegaly regarding the pathophysiology of bone growth?
- Gigantism occurs before the closure of epiphyseal plates, leading to linear growth, whereas acromegaly occurs after closure, causing bone thickening. (correct)
- Gigantism primarily affects long bones, whereas acromegaly affects flat bones exclusively.
- Gigantism is caused by increased growth hormone, while acromegaly is caused by decreased somatostatin.
- Gigantism involves cartilage overgrowth, while acromegaly involves periosteal bone formation.
Why is the Oral Glucose Challenge Test definitive for diagnosing acromegaly?
Why is the Oral Glucose Challenge Test definitive for diagnosing acromegaly?
Considering the complications associated with surgical removal of a pituitary tumor, what is the most critical post-operative concern that requires continuous monitoring?
Considering the complications associated with surgical removal of a pituitary tumor, what is the most critical post-operative concern that requires continuous monitoring?
Why are proton beam therapy and gamma knife radiosurgery preferred over traditional radiation therapy for treating acromegaly?
Why are proton beam therapy and gamma knife radiosurgery preferred over traditional radiation therapy for treating acromegaly?
Given that acromegaly can cause enlargement of the heart (cardiomegaly), liver (hepatomegaly), and spleen (splenomegaly), how does this multi-organ involvement primarily impact patient management?
Given that acromegaly can cause enlargement of the heart (cardiomegaly), liver (hepatomegaly), and spleen (splenomegaly), how does this multi-organ involvement primarily impact patient management?
How does acromegaly's effect on muscle tissue typically manifest, and what are the potential long-term consequences of this?
How does acromegaly's effect on muscle tissue typically manifest, and what are the potential long-term consequences of this?
In the context of diabetes insipidus (DI), what is the underlying mechanism that leads to hypernatremia, and how does this impact the selection of appropriate nursing interventions?
In the context of diabetes insipidus (DI), what is the underlying mechanism that leads to hypernatremia, and how does this impact the selection of appropriate nursing interventions?
What is the rationale behind monitoring urine specific gravity in patients with diabetes insipidus (DI), and how does this parameter guide clinical decision-making?
What is the rationale behind monitoring urine specific gravity in patients with diabetes insipidus (DI), and how does this parameter guide clinical decision-making?
Why is it critical to differentiate between central and nephrogenic diabetes insipidus (DI) when determining a treatment plan, and what diagnostic approach is used to distinguish between these conditions?
Why is it critical to differentiate between central and nephrogenic diabetes insipidus (DI) when determining a treatment plan, and what diagnostic approach is used to distinguish between these conditions?
Considering the water deprivation test used in diagnosing diabetes insipidus (DI), what physiological parameters must be rigorously monitored, and why is it essential to assess these parameters before and during the test?
Considering the water deprivation test used in diagnosing diabetes insipidus (DI), what physiological parameters must be rigorously monitored, and why is it essential to assess these parameters before and during the test?
What is the rationale behind fluid restriction as a primary intervention in managing Syndrome of Inappropriate Antidiuretic Hormone (SIADH), and how does this restriction impact overall fluid and electrolyte balance?
What is the rationale behind fluid restriction as a primary intervention in managing Syndrome of Inappropriate Antidiuretic Hormone (SIADH), and how does this restriction impact overall fluid and electrolyte balance?
Why is the administration of hypertonic saline a high-risk intervention in severe hyponatremia associated with Syndrome of Inappropriate Antidiuretic Hormone (SIADH), and what specific monitoring parameters are crucial during its infusion?
Why is the administration of hypertonic saline a high-risk intervention in severe hyponatremia associated with Syndrome of Inappropriate Antidiuretic Hormone (SIADH), and what specific monitoring parameters are crucial during its infusion?
How does the management of hyponatremia in Syndrome of Inappropriate Antidiuretic Hormone (SIADH) differ from that in other conditions causing low sodium levels, and why is this distinction critical?
How does the management of hyponatremia in Syndrome of Inappropriate Antidiuretic Hormone (SIADH) differ from that in other conditions causing low sodium levels, and why is this distinction critical?
Given that Thyroid Stimulating Hormone (TSH) levels are typically suppressed in hyperthyroidism, what additional diagnostic findings are crucial in differentiating between Graves' disease and toxic multinodular goiter as the underlying cause?
Given that Thyroid Stimulating Hormone (TSH) levels are typically suppressed in hyperthyroidism, what additional diagnostic findings are crucial in differentiating between Graves' disease and toxic multinodular goiter as the underlying cause?
Considering the potential for thyroid storm following manipulation of the thyroid gland, what immediate interventions are essential to mitigate the associated hypermetabolic state and prevent life-threatening complications?
Considering the potential for thyroid storm following manipulation of the thyroid gland, what immediate interventions are essential to mitigate the associated hypermetabolic state and prevent life-threatening complications?
Post-thyroidectomy patients are at risk for hypocalcemia due to potential parathyroid gland damage. Which assessment findings are the most reliable indicators of acute hypocalcemia, necessitating immediate intervention?
Post-thyroidectomy patients are at risk for hypocalcemia due to potential parathyroid gland damage. Which assessment findings are the most reliable indicators of acute hypocalcemia, necessitating immediate intervention?
How does pre-operative iodine administration contribute to reducing the risk of hemorrhage during subtotal thyroidectomy, and what underlying physiological mechanism facilitates this effect?
How does pre-operative iodine administration contribute to reducing the risk of hemorrhage during subtotal thyroidectomy, and what underlying physiological mechanism facilitates this effect?
What are the key clinical distinctions between thyroid storm and simple hyperthyroidism, and how do these differences guide immediate therapeutic interventions?
What are the key clinical distinctions between thyroid storm and simple hyperthyroidism, and how do these differences guide immediate therapeutic interventions?
Flashcards
Acromegaly Definition
Acromegaly Definition
Overproduction of growth hormone after puberty, once growth plates have closed.
Acromegaly Causes
Acromegaly Causes
Idiopathic hyperplasia or tumor growth, typically in the pituitary gland.
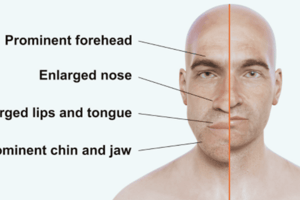
Acromegaly Facial/Skeletal Changes
Acromegaly Facial/Skeletal Changes
Enlargement of cranium/lower jaw, separation of teeth, bulging forehead, bulbous nose, thick lips, enlarged tongue, coarse facial features.
Acromegaly Symptoms
Acromegaly Symptoms
Signup and view all the flashcards
Acromegaly Diagnosis
Acromegaly Diagnosis
Signup and view all the flashcards
Acromegaly Treatment
Acromegaly Treatment
Signup and view all the flashcards
Gigantism Definition
Gigantism Definition
Signup and view all the flashcards
Gigantism Treatment
Gigantism Treatment
Signup and view all the flashcards
Dwarfism Definition
Dwarfism Definition
Signup and view all the flashcards
Dwarfism Etiology
Dwarfism Etiology
Signup and view all the flashcards
Dwarfism Characteristics
Dwarfism Characteristics
Signup and view all the flashcards
Dwarfism Treatment
Dwarfism Treatment
Signup and view all the flashcards
Diabetes Insipidus (DI)
Diabetes Insipidus (DI)
Signup and view all the flashcards
Diabetes Insipidus Etiology
Diabetes Insipidus Etiology
Signup and view all the flashcards
Diabetes Insipidus Urine
Diabetes Insipidus Urine
Signup and view all the flashcards
Diabetes Insipidus Electrolytes
Diabetes Insipidus Electrolytes
Signup and view all the flashcards
SIADH Cause
SIADH Cause
Signup and view all the flashcards
SIADH Definition
SIADH Definition
Signup and view all the flashcards
SIADH and Sodium Levels
SIADH and Sodium Levels
Signup and view all the flashcards
Hyperthyroidism Definition
Hyperthyroidism Definition
Signup and view all the flashcards
Study Notes
- Acromegaly is marked by growth hormone overproduction post-puberty after growth plates seal, leading to physical changes, mostly affecting adults.
Key Points of Acromegaly
- Is defined as growth hormone overproduction after puberty and growth plate closure
- Causes irreversible physical changes
- Can be caused by idiopathic hyperplasia or tumor growth, typically in the pituitary gland
- Has an insidious onset, with symptoms developing slowly over years
- Onset typically begins in the third or fourth decade of life (30s or 40s)
- Diagnosis may be delayed by 7-9 years from symptoms' onset
Signs and Symptoms of Acromegaly
- Skeletal changes include enlargement of the cranium and lower jaw, teeth separation due to jaw growth, and a prominent, bulging forehead
- Facial features include a bulbous nose, thick lips, enlarged tongue (macroglossia), and coarsening facial features
- Extremities exhibit enlargement of hands and feet and tufted fingertips with a clubbed appearance
- Organ enlargement may include enlargement of the heart (cardiomegaly), liver (hepatomegaly), and spleen (splenomegaly)
- Musculoskeletal symptoms include muscle weakness and joint hypertrophy and pain
- Reproductive effects include impotence (erectile dysfunction) in males
- Reproductive effects for females include a deepened voice, increased facial hair (hirsutism), and amenorrhea (absence of menstruation)
- Neurological symptoms include visual changes (partial or complete blindness) due to optic nerve pressure and severe headaches
Diagnosis of Acromegaly
- Includes assessing changes noticed by the patient through history and a physical exam
- Observe characteristic signs and symptoms
- Use CT scans and MRIs to detect tumors
- Cranial radiographic evaluation (X-rays of the cranium) can be used
- Assess for visual field defects in a visual exam
- Lab tests are used to confirm elevated growth hormone levels
- The Oral Glucose Challenge Test is definitive, where GH levels don't fall as expected after glucose administration; patients must be NPO for 10-12 hours prior to the test
Treatment of Acromegaly
- Pharmacological options include dopamine agonists to suppress growth hormone
- Surgical options include surgical removal of the pituitary tumor
- Surgery increases the risk for diabetes insipidus post-surgery
- Radiation therapy like proton beam therapy (gamma knife radiosurgery) is less destructive to surrounding tissues than traditional radiation
Complications of Acromegaly
- Can include cardiovascular issues like hypertension, heart failure, and cardiomyopathy (enlarged, poorly functioning heart)
Nursing Interventions for Acromegaly
- Assess and support the patient's ability to perform Activities of Daily Living (ADLs)
- Provide assistance as needed, especially as the condition progresses
- Offer a soft and easy-to-chew diet, allow adequate time for meals, and encourage fluid intake
- Manage pain with non-opioid analgesics
- Address visual impairment by decluttering the room and keeping frequently used items within easy reach
- Monitor vital signs, including heart and lung sounds
- Assess fluid status, monitoring for signs of heart failure
- Monitor weight, encouraging a healthy weight
- Address psychological distress and provide emotional support
- Encourage exercise and range of motion exercises to maintain joint mobility
Gigantism
- Gigantism results from excessive growth hormone, leading to overgrowth of bones, muscles, and organs.
Key Points of Gigantism
- Etiology is excess growth hormone
- Diagnosed via growth hormone suppression test, baseline levels of growth hormone are high
- Treat with surgical removal or irradiation of the anterior pituitary gland and post-surgery hormone replacement therapy
- Complications include hypertension and heart failure, osteoporosis and thickened bones, delayed sexual development, self-esteem issues, and shorter lifespan
- Andre the Giant had gigantism
Dwarfism
- Dwarfism involves a shorter stature than peers
Key points of Dwarfism
- Etiology: Hypopituitary dwarfism, genetic mutations, and idiopathic causes
- Characteristics: Shorter stature, underdeveloped jaws, delayed but normal sexual development, and normal intelligence
- Individuals with dwarfism can still produce normal-sized offspring
- Treatment: surgery if a tumor is present, or replacement of growth hormone via injection
- Nursing assessment: Plot height and weight on growth charts to identify children below the third percentile for height, and referral to a provider for further testing if growth is below the third percentile
- Complications: Self-esteem issues and musculoskeletal and cardiovascular complications due to a disproportionately small torso
- Diagnosis: Radiographic evaluation of the skull and skeleton to assess bone age, MRI and CT scans to check for pituitary tumors, and decreased growth hormone levels are definitive; NPO past midnight before testing.
- Genetic counseling is recommended for family planning to assess the risk of dwarfism in offspring
- Signs and Symptoms: Onset of growth retardation, headaches, visual disturbances, and behavioral changes
- Nursing care: Encourage age-appropriate clothing, emphasize abilities and strengths, and address psychosocial needs
- Most clients can lead fairly normal lives and can have normal-sized children
- Potential complications: Musculoskeletal and cardiovascular system issues
Diabetes Insipidus
- Is a metabolic disorder of the posterior pituitary
- The disorder is characterized by a deficiency in antidiuretic hormone (ADH) and is distinct from diabetes mellitus
Key Points of Diabetes Insipidus
- The pathophysiology of Diabetes Insipidus is a deficiency in ADH, which leads to excessive urine output
- Can be transient or permanent
- Etiology can be primary or secondary to conditions like head injuries, intracranial tumors, aneurysms, or infections (encephalitis, meningitis)
- Clinical manifestations include polyuria (marked increase in urine output) and polydipsia (intense thirst due to fluid loss), which can lead to dehydration
- Urine characteristics: Very dilute urine and low specific gravity (measures the urine concentration)
- Urine output: Ranges from 5 to 20 liters in 24 hours, with a minimum of 200 mL per hour for greater than two hours
- Fluid intake: Patients crave ice water and may need to drink 4 to 20 liters of fluid per day
- Electrolyte imbalance: Hypernatremia (elevated sodium levels) results from dehydration
Key Differences Between Gigantism, Dwarfism, and Diabetes Insipidus
- Hormone related to each condition:
- Gigantism: Excess Growth Hormone
- Dwarfism: Deficiency in Growth Hormone
- Diabetes Insipidus: Deficiency in Antidiuretic Hormone (ADH)
- Key symptom for each condition:
- Gigantism: Excessive Growth
- Dwarfism: Short Stature
- Diabetes Insipidus: Polyuria (excessive urination)
- Other symptoms:
- Gigantism: Hypertension and thickened bones
- Dwarfism: Underdeveloped jaws and delayed sexual development
- Diabetes Insipidus: Polydipsia (excessive thirst) and dehydration and hypernatremia
- Treatment:
- Gigantism: Surgery, irradiation, and hormone replacement
- Dwarfism: Growth hormone replacement, surgery if a tumor is present
- Diabetes Insipidus: Fluid replacement and medication to manage ADH levels
Diabetes Insipidus (DI) Additional Information
- DI may result from the body's inability to regulate fluid balance, leading to excessive urination, its mismanagement can cause severe dehydration and electrolyte imbalances
- Characterized by excessive urination where patients urinate frequently and in large volumes
- Caused by the inability to keep up orally, meaning in severe cases, patients cannot drink enough water to compensate for losses through urination
- Hypovolemic shock can occur because of the body's inability to conserve water, leading to low blood pressure, elevated heart rate, and elevated respirations
- Electrolyte imbalances occur, changes in the level of consciousness can occur due to electrolyte changes, particularly hypernatremia
- Symptoms include: Hypernatremia, tachycardia, hypotension, weakness, tiredness, and lethargy
Nursing Interventions for Diabetes Insipidus
- Check skin turgor frequently on the chest or forehead to assess hydration status
- Maintain a bedside commode to reduce the risk of falls due to frequent trips to the bathroom
- Administer IV fluids to help maintain hydration
Safety, Assessment, and Monitoring of Diabetes Insipidus Patients
- Safety: Ensure patient safety due to weakness, tiredness, and lethargy
- Urine assessment: Note the color and specific gravity of the urine using a dipstick or sending it to the lab
- Monitor for constipation due to water loss in the large intestine
- Daily weight: Weigh the patient daily in the early morning before breakfast, using the same scale, amount of clothes, and time of day
- Nocturia: Determine the presence of nocturia, which can worsen weakness, tiredness, and lethargy.
- Monitor for dehydration by assessing mucous membranes and skin turgor
- Monitor and document vital signs
- Avoid alcohol and caffeine because they are diuretics and can worsen the condition
- Closely monitor lab results
Diagnostic Findings of DI
- Specific gravity is usually below 1.003 due to very dilute urine.
- Serum sodium is higher than 145 mEq/L due to hypernatremia.
- Serum osmolality is greater than 300 mOsm/kg due to dehydration.
Water Deprivation Test for DI
- Procedure: Withhold fluids for 12 hours, then measure urine specific gravity and serum osmolality frequently; monitor orthostatic vital signs and weight before and after the test
- A CT scan of the sella turcica (depression in the sphenoid bone where the pituitary gland is located) may be performed
- ADH measurement: Urinary ADH measurement
Syndrome of Inappropriate Secretion of Antidiuretic Hormone (SIADH)
- SIADH is the opposite of Diabetes Insipidus, involving excessive release of antidiuretic hormone (ADH), leading to water retention, decreased urine output, and expanded vascular fluid volume without edema
Key Points of SIADH
- Excessive ADH release where the pituitary gland releases too much ADH
- Kidneys reabsorb water, decreasing urine output
Fluid Balance and Symptoms of SIADH
- Fluid Volume Expansion: Increased fluid volume in the vascular space (arteries and veins) without edema
- No Edema: Fluid overload occurs in the vessels, not in the tissues, so there is no edema
- Hyponatremia: Low sodium levels due to excess water in the blood
- Hemodilution occurs as the blood is dilute
- Water intoxication can lead to cerebral edema due to excess water
- Early symptoms (Sodium < 125 mEq/L): Nausea and vomiting, tremors, cramping, anorexia, headaches, confusion, and irritability
- Worsening symptoms: Seizures, stupor, coma, and pathologic reflexes
Pathophysiology of Water Intoxication Relating to SIADH
- Fluid Intake vs. Output: Fluid intake exceeds urine output with no edema.
- Serum Hypotonicity: The serum becomes more hypotonic.
- Brain Cell Swelling: Brain cells swell or expand due to hypotonicity.
- Neurological Changes: Leads to lethargy and personality changes due to swelling in the brain.
Comparing Diabetes Insipidus (DI) and SIADH
- ADH Levels:
- DI: Decreased or ineffective ADH
- SIADH: Increased ADH
- Urine Output:
- DI: Increased (polyuria)
- SIADH: Decreased (oliguria)
- Serum Sodium:
- DI: Increased (hypernatremia)
- SIADH: Decreased (hyponatremia)
- Serum Osmolality:
- DI: Increased
- SIADH: Decreased
- Urine Specific Gravity:
- DI: Decreased (dilute urine)
- SIADH: Increased (concentrated urine)
- Fluid Volume Status:
- DI: Dehydration
- SIADH: Fluid overload (without edema in early stages)
- Key Problem:
- DI: Water loss
- SIADH: Water retention
- Complications:
- DI: Dehydration, electrolyte imbalance, hypovolemic shock
- SIADH: Water intoxication, cerebral edema, seizures, coma
- Edema:
- DI: Absent
- SIADH: Absent (initially), but can occur with severe water intoxication
Additional key points of SIADH include:
- Is a condition where the body retains too much fluid
- If not addressed, can lead to seizures, coma, and even death
- Labs:
- Sodium levels will be lower than 135 mEq/L, typically 135-145 mEq/L
- BUN (Blood Urea Nitrogen) and creatinine levels will be low to normal, indicating the problem typically isn't kidney damage
- Urine specific gravity will be high (greater than 1.032), indicating concentrated urine
- Urine sodium will be elevated
- Sodium levels will be lower than 135 mEq/L, typically 135-145 mEq/L
- Treatment:
- Fluid restriction, aiming for intake to equal output
- Hypertonic saline IV infusion, administered slowly to avoid complications
- Diuretics to help the kidneys excrete excess fluid
- Medications like declomycin or lithium carbonate to interfere with antidiuretic hormone action, promoting polyuria
- Surgical resection, radiation, or chemotherapy may be necessary if the cause is a tumor or malignancy
Nursing interventions for SIADH include:
- Neurological exams based on the patient's condition
- Hydration assessments
- Monitoring breath sounds for adventitious sounds like rails, crackles, or rhonchi
- Strict fluid restriction
- Lab monitoring
- Daily weight and I&O (intake and output) monitoring
- Avoidance of salty foods to minimize thirst
- Frequent oral care
- The presentation of SIADH can vary greatly from person to person
Hyperthyroidism
- Is a condition characterized by increased activity of the thyroid gland, leading to an overproduction of thyroid hormones T3 and T4
- Can result in an increased metabolism
- Other names include Graves' disease, exophthalmic goiter, and thyrotoxicosis
Key Points of Hyperthyroidism
- Physiological effects include increased metabolism due to elevated T3 and T4 levels and visible edema of the anterior neck due to thyroid gland enlargement (goiter)
- Exophthalmos, or bulging of the eyeballs, could lead to incomplete eye closure, corneal dryness, corneal ulcers, and vision loss
- Is more commonly seen in women, typically between 20 and 50 years of age
Signs and Symptoms of Hyperthyroidism
- Dysphagia (difficulty swallowing) due to swelling in the neck
- Hoarseness
- Jitteriness and nervousness
- Weight loss despite a good appetite
- Insomnia
- Emotional lability and overreaction to situations
- Rapid pulse and elevated blood pressure
- Bruit over the thyroid gland (audible upon auscultation)
- Heart palpitations and shortness of breath
- Difficulty with mental focus and concentration/short-term memory loss
- Warm, flushed skin
- Cessation of menstrual periods
- Elevated temperature and heat intolerance
- Profuse diaphoresis (sweating)
- Tremors of the hands
- Hyperactivity and clumsiness
- Think of the patient as "exercising 24 hours a day" to remember the signs and symptoms
Diagnosis, Medical, and Treatment interventions of Hyperthyroidism
- Diagnosis includes decreased TSH (Thyroid Stimulating Hormone) levels because T3 and T4 levels are high, and when those are high, TSH production is suppressed
- Radioactive iodine is taken up by the thyroid gland to destroy the hyperactive thyroid tissue, with full affect typically seen within 6-8 weeks. After this medical intervention, the patient is highly likely to develop hypothyroidism.
- Treatment options include:
- PTU (Propylthiouracil) and Tapazole (Methimazole) which suppress the thyroid gland's hormone production
- Suubtotal Thyroidectomy
- Thyroidectomy:
- Is less common now due to other available treatments
- Can lead to complications including hemorrhage, hypoparathyroidism (due to parathyroid gland damage), and vocal cord paralysis
- Pre-Operative Considerations:
- Delay surgery until the thyroid is back to a normal size using PTU or Tapazole which reduces the risk of thyroid crisis during surgery
- Thyroid Crisis (Thyroid Storm):
- Can occur during surgery due to manipulation of the thyroid gland, causing a surge of thyroid hormones into the bloodstream
- Considered the ‘gold standard’ treatment
- Destroys thyroid tissue, ultimately eliminating the need for surgery
- May be preceded by PTU or Tapazole
- Radiation Safety Precautions:
- Generally low levels of radiation, but pregnant individuals and nurses should avoid contact with patients undergoing radioactive iodine treatment
- Hypothyroidism Post-Treatment:
- Patients may require lifelong thyroid hormone replacement (e.g., levothyroxine)
- Dietary Recommendations: High-calorie, high-protein diet with vitamins and minerals, along with soft, easily swallowed foods, especially if dysphagia is present; also avoid caffeine
- Pre-operative Iodine Administration:
- Decreases vascularity and size of the thyroid gland to reduce hemorrhage risk during subtotal thyroidectomy
- Pre-operative Teaching:
- Teach to support the head while turning + teaching to maintain a neutral anatomic position and move as a log to avoid stressing the incision incision
- Post-operative Care:
- Avoid side-to-side head movements
- Deep breathing exercises, but limit coughing also keep the environment: Clear, Cool, and quiet with limited visitors.
- Encourage food and fluids also set patient in Semi-Fowler's position and avoid hyperextending the head
- Regular voice checks to monitor for vocal cord paralysis; notify the provider immediately if the patient cannot make a sound and keep suction and tracheostomy tray available for emergencies
- Humidifier at the bedside to soothe the throat and prevent coughing also always assess and monitor vital signs with a focus on respirations to monitor for breathing difficulties and signs and symptoms of hemorrhage, including checking behind the neck for pooling blood
Hypocalcemia Post-Thyroidectomy
- Following a thyroidectomy due to potential damage to, or removal of, the parathyroid glands puts a patient at risk for hypocalcemia.
Key Terms and important points
- Parathyroid glands are located on the back of the thyroid gland and accidental removal or damage during thyroidectomy can lead to hypocalcemia
- Hypocalcemia is defined as a calcium level less than 9
- Signs and symptoms of hypocalcemia include:
- Carpopedal spasms: Spasms of the wrists and feet
- Laryngeal spasm or stridor: Closing of the larynx, causing difficulty breathing
- Chvostek's sign: Abnormal spasm of facial muscles elicited by tapping the facial nerve
- Trousseau's sign: Carpal spasm induced by inflating a blood pressure cuff above the systolic pressure for three minutes
- Testing Chvostek's Sign: Tapping on the facial nerve elicits facial spasms is indicative of hypocalcemia
- Testing Trousseau's Sign: Inflating a BP cuff above systolic pressure for 3 minutes, Carpal spasm indicates hypocalcemia
- Untreated Hypocalcemia: Can lead to seizures and lethal cardiac arrhythmias, thus, the treatment for hypocalcemia is Calcium gluconate IV
Thyroid Crisis (Thyroid Storm)
- This section describes thyroid crisis, a severe and life-threatening condition that can occur post-thyroidectomy due to the sudden release of large amounts of thyroid hormones.
Key Terms and important points
- Thyroid Crisis/Storm is a severe form of hyperthyroidism, often triggered by manipulation of the thyroid gland during surgery; it’s characterized by a massive release of T3 and T4 hormones typically occurs within the first 12 hours post-op
- Signs and Symptoms: Nausea and vomiting, severe tachycardia, severe hypertension, hyperthermia (up to 106°F), restlessness, cardiac dysrhythmias, and delirium
- Treatment: IV fluids, sodium iodide, corticosteroids, antipyretics to reduce fever, PTU or Tapazole and Oxygen PRN
- Thyroid crisis requires immediate treatment to prevent severe complications and death
Thyroidectomy Post-Op Complications and Actions
- Hemorrhage:
- Sign: Bleeding at the incision site
- Symptom: Swelling and hematoma formation
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.