Podcast
Questions and Answers
What is the primary function of the circulatory system?
What is the primary function of the circulatory system?
- To regulate body temperature
- To transport gases, nutrients, and waste products (correct)
- To provide a framework for the body
- To digest food and absorb nutrients
Which structure in the circulatory system is responsible for carrying blood away from the heart?
Which structure in the circulatory system is responsible for carrying blood away from the heart?
- Capillaries
- Veins
- Arteries (correct)
- Venules
What is a key difference between arteries and veins?
What is a key difference between arteries and veins?
- Veins have a larger total diameter than arteries (correct)
- Arteries carry blood toward the heart
- Arteries contain valves to prevent backflow
- Veins have thicker walls than arteries
What type of blood vessel leads directly into capillaries?
What type of blood vessel leads directly into capillaries?
What is the smallest blood vessel where materials are exchanged between blood and tissue fluid?
What is the smallest blood vessel where materials are exchanged between blood and tissue fluid?
What is the composition of the tunica media in blood vessels?
What is the composition of the tunica media in blood vessels?
Which layer of a blood vessel is closest to the lumen?
Which layer of a blood vessel is closest to the lumen?
What structure supplies blood to the walls of larger blood vessels?
What structure supplies blood to the walls of larger blood vessels?
What is the second main branch of the abdominal aorta?
What is the second main branch of the abdominal aorta?
Which arteries arise from the inferior mesenteric artery?
Which arteries arise from the inferior mesenteric artery?
What is the main low resistance flow pattern observed in the vascular structure?
What is the main low resistance flow pattern observed in the vascular structure?
Where does the inferior vena cava (IVC) begin?
Where does the inferior vena cava (IVC) begin?
Which statement about the renal arteries is accurate?
Which statement about the renal arteries is accurate?
What unique characteristic does the inferior vena cava have compared to other veins?
What unique characteristic does the inferior vena cava have compared to other veins?
What is the significance of different wave patterns observed pre and post prandial?
What is the significance of different wave patterns observed pre and post prandial?
What is the largest artery in the body?
What is the largest artery in the body?
Which of the following is a clinical reason for sonographic evaluation of the aorta?
Which of the following is a clinical reason for sonographic evaluation of the aorta?
What is the diameter of the abdominal aorta in men as presented in the data?
What is the diameter of the abdominal aorta in men as presented in the data?
Which of the following is NOT a risk factor for an abdominal aortic aneurysm?
Which of the following is NOT a risk factor for an abdominal aortic aneurysm?
Which symptom is associated with a rupture of an abdominal aortic aneurysm?
Which symptom is associated with a rupture of an abdominal aortic aneurysm?
What is a pseudoaneurysm?
What is a pseudoaneurysm?
Which condition can simulate a pulsatile abdominal mass?
Which condition can simulate a pulsatile abdominal mass?
Which of the following statements about abdominal aortic aneurysms is false?
Which of the following statements about abdominal aortic aneurysms is false?
Which type of aneurysm involves localized dilation and involves inflammation of the artery wall?
Which type of aneurysm involves localized dilation and involves inflammation of the artery wall?
Which of the following findings is NOT typically associated with an abdominal aortic aneurysm?
Which of the following findings is NOT typically associated with an abdominal aortic aneurysm?
What size abdominal aortic aneurysm typically requires surgical intervention?
What size abdominal aortic aneurysm typically requires surgical intervention?
What is a characteristic feature of a pseudoaneurysm?
What is a characteristic feature of a pseudoaneurysm?
Which type of aneurysm has a 95% occurrence rate in relation to being infrarenal?
Which type of aneurysm has a 95% occurrence rate in relation to being infrarenal?
What is the cumulative incidence of rupture for abdominal aortic aneurysms larger than 5 cm over 8 years?
What is the cumulative incidence of rupture for abdominal aortic aneurysms larger than 5 cm over 8 years?
Which treatment option is less invasive for abdominal aortic aneurysms?
Which treatment option is less invasive for abdominal aortic aneurysms?
Which of the following describes a mycotic aneurysm?
Which of the following describes a mycotic aneurysm?
Which characteristic is true of an abdominal aortic aneurysm measuring over 6 cm?
Which characteristic is true of an abdominal aortic aneurysm measuring over 6 cm?
In a pseudoaneurysm, where does blood escape from?
In a pseudoaneurysm, where does blood escape from?
What are the different types of abdominal aortic aneurysms identified?
What are the different types of abdominal aortic aneurysms identified?
What impact does a larger abdominal aortic aneurysm size typically have on surgical risk?
What impact does a larger abdominal aortic aneurysm size typically have on surgical risk?
What is a common symptom of a rupture?
What is a common symptom of a rupture?
Which of the following is a characteristic of aortic dissection?
Which of the following is a characteristic of aortic dissection?
Which artery is not a branch of the celiac trunk?
Which artery is not a branch of the celiac trunk?
How does the celiac axis primarily supply blood?
How does the celiac axis primarily supply blood?
Which of the following arteries does not belong to the abdominal aortic branches?
Which of the following arteries does not belong to the abdominal aortic branches?
What does the presence of an 'intimal flap' on ultrasound indicate?
What does the presence of an 'intimal flap' on ultrasound indicate?
Which artery branches into the Splenic Artery, Left Gastric Artery, and Common Hepatic Artery?
Which artery branches into the Splenic Artery, Left Gastric Artery, and Common Hepatic Artery?
Which artery is classified as a parietal visceral branch of the abdominal aorta?
Which artery is classified as a parietal visceral branch of the abdominal aorta?
Which abdominal aortic branch is responsible for supplying blood to the intestines?
Which abdominal aortic branch is responsible for supplying blood to the intestines?
What major function does the abdominal aorta serve?
What major function does the abdominal aorta serve?
Flashcards
Arteries in the Abdomen
Arteries in the Abdomen
Hollow elastic tubes that carry blood away from the heart. They are enclosed within a sheath containing a vein and a nerve. Smaller arteries have less elastic tissue and more smooth muscles compared to larger arteries.
Veins in the Abdomen
Veins in the Abdomen
Hollow collapsible tubes carrying blood towards the heart. They have less elastic tissue and muscle than arteries and appear collapsed. They have a larger total diameter than arteries and move blood more slowly.
Tunica Intima
Tunica Intima
The inner layer of arteries and veins, composed of three parts: endothelial cells lining the lumen, delicate connective tissue, and an elastic layer formed by elastic fibers.
Tunica Media
Tunica Media
Signup and view all the flashcards
Tunica Adventitia
Tunica Adventitia
Signup and view all the flashcards
Capillaries
Capillaries
Signup and view all the flashcards
Arterioles
Arterioles
Signup and view all the flashcards
Venules
Venules
Signup and view all the flashcards
Aorta
Aorta
Signup and view all the flashcards
Aorta Sections
Aorta Sections
Signup and view all the flashcards
Sonography of the Aorta
Sonography of the Aorta
Signup and view all the flashcards
Abdominal Aortic Aneurysm (AAA)
Abdominal Aortic Aneurysm (AAA)
Signup and view all the flashcards
Aortic Ectasia
Aortic Ectasia
Signup and view all the flashcards
Pseudoaneurysm
Pseudoaneurysm
Signup and view all the flashcards
Aortic Aneurysm Rupture
Aortic Aneurysm Rupture
Signup and view all the flashcards
Aortic Dissection
Aortic Dissection
Signup and view all the flashcards
Atherosclerosis
Atherosclerosis
Signup and view all the flashcards
Risk Factors for AAA
Risk Factors for AAA
Signup and view all the flashcards
Aortic Rupture
Aortic Rupture
Signup and view all the flashcards
Abdominal Aorta
Abdominal Aorta
Signup and view all the flashcards
Celiac Axis
Celiac Axis
Signup and view all the flashcards
Abdominal Aortic Branches
Abdominal Aortic Branches
Signup and view all the flashcards
Splenic Artery
Splenic Artery
Signup and view all the flashcards
Left Gastric Artery
Left Gastric Artery
Signup and view all the flashcards
Common Hepatic Artery
Common Hepatic Artery
Signup and view all the flashcards
Low Resistance Flow in the Celiac Axis
Low Resistance Flow in the Celiac Axis
Signup and view all the flashcards
Mycotic Aneurysm
Mycotic Aneurysm
Signup and view all the flashcards
Fusiform Aneurysm
Fusiform Aneurysm
Signup and view all the flashcards
Saccular Aneurysm
Saccular Aneurysm
Signup and view all the flashcards
Bulbous Aneurysm
Bulbous Aneurysm
Signup and view all the flashcards
AAA location relative to renal arteries
AAA location relative to renal arteries
Signup and view all the flashcards
Infrarenal Aneurysm
Infrarenal Aneurysm
Signup and view all the flashcards
Endovascular Stent Graft
Endovascular Stent Graft
Signup and view all the flashcards
Rupture of Abdominal Aortic Aneurysm
Rupture of Abdominal Aortic Aneurysm
Signup and view all the flashcards
What is the SMA?
What is the SMA?
Signup and view all the flashcards
What are the renal arteries?
What are the renal arteries?
Signup and view all the flashcards
What is the IMA?
What is the IMA?
Signup and view all the flashcards
What is the IVC?
What is the IVC?
Signup and view all the flashcards
What is the 'hammocking' of the IVC?
What is the 'hammocking' of the IVC?
Signup and view all the flashcards
What is the hepatic vein?
What is the hepatic vein?
Signup and view all the flashcards
What is the portal vein?
What is the portal vein?
Signup and view all the flashcards
Study Notes
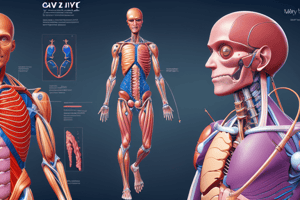
Abdominal Vasculature
- The abdominal vascular system is responsible for transporting gases, nutrients, and essential substances to tissues and removing waste products.
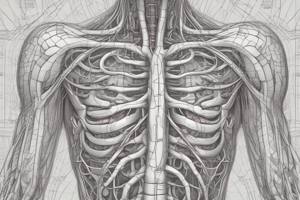
- Arteries are elastic tubes that carry blood away from the heart, often enclosed with a vein and nerve. Smaller arteries have less elastic tissue and more smooth muscle compared to larger ones.
- Arteries' elasticity is critical for maintaining steady blood flow. The pulsation of the abdominal aorta does not change with respiration.
- Veins are collapsible tubes with less tunica media. They appear collapsed and generally have a larger diameter than arteries. Veins have valves to prevent backflow and carry blood toward the heart. The IVC slightly expands with suspended respiration.
- Arteries branch into arterioles, then capillaries. Capillaries form a network where materials exchange between blood and tissue fluid.
- Venules collect blood from capillaries and form larger vessels that return blood to the heart.
- Arteries and veins consist of three layers: Tunica intima (inner), Tunica media (middle), and Tunica adventitia (outer). The vasa vasorum supplies the walls of blood vessels.
- The aorta is the largest artery in the body and divides into five sections: root, ascending aorta & arch, descending thoracic aorta, abdominal aorta, and bifurcation into iliac arteries.
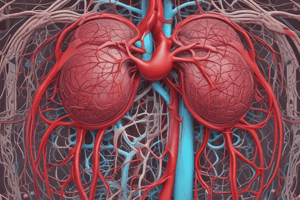
- The abdominal aorta supplies blood to various organs via branches (e.g., celiac trunk, superior mesenteric artery, renal arteries, inferior mesenteric artery).
Sonography of the Aorta
- Clinically, sonography is used to evaluate conditions like pulsating abdominal masses, abdominal pain, abdominal bruits, and hemodynamic compromise in the lower legs.
- The arterial system can be affected by calcification, aneurysm, infection, rupture, or thrombosis.
- Normal aorta and iliac diameters vary based on sex (Men 2.0 ± 2.5 cm, Women 1.7 ± 1.5 cm for aorta, Men 1.3 ± 2.0 cm, Women 1.2 ± 1.3 cm for common iliac arteries)
Pathology of the Aorta: Abdominal Aortic Aneurysm (AAA)
- AAA involves dilation of the abdominal aorta exceeding 3 cm and affecting all three vessel layers (bulbous, saccular, fusiform).
- Aortic locations are categorized as suprarenal, at renal level, and infrarenal.
- 95% of AAAs are infrarenal.
- Risk factors include tobacco use, hypertension, vascular disease, COPD, family history of AAA, and genetic disorders (Marfan's, Ehlers-Danlos syndrome).
- Symptoms include palpable abdominal mass, back pain, and a drop in hematocrit (rupture).
- "Pseudo-pulsatile" abdominal masses include retroperitoneal tumors, large fibroid uteri, and paraaortic nodes (transmissions of pulsations from the aorta).
- Aortic dissection involves separation between the vessel's layers, often diagnosed with an ultrasound showing an "intimal flap".
Size and Treatment
- Treatment options depend on the aneurysm size. Aneurysms <4 cm are monitored every 6 months; symptomatic aneurysms are considered for intervention.
- 4-5 cm aneurysms usually undergo surgical intervention.
- Aneurysms > 6 cm are considered high risk for surgery.
- Endovascular stent grafts (less invasive) can be utilized for patients who are higher risk for surgery; endovascular grafts are often recommended with renal and iliac vessel involvement.
Pseudoaneurysm
- A pseudoaneurysm is a pulsatile hematoma resulting from blood leakage into soft tissue surrounding a ruptured artery, contained by deeper vessel layers.
- Doppler ultrasound is employed to visualize the neck and internal anatomy of the aneurysm, guiding potential thrombin injection treatments
Rupture of Aortic Aneurysm
- Aortic rupture has a 50% mortality rate. Rupture risk increases with aneurysm size (>5 cm has a 25% cumulative rupture chance over 8 years).
- Rupture symptoms include excruciating abdominal pain, shock, and expanding abdominal mass.
Aortic Dissection
- Aortic dissection is diagnosed by identifying vessel wall layer separation, particularly the visualization of "intimal flap" on ultrasound scans.
Abdominal Aortic Branches: Visceral
- Celiac axis/trunk, superior mesenteric, renal, and inferior mesenteric arteries comprise visceral branches, vital for visceral organ perfusion.
Abdominal Aortic Branches: Parietal
- Inferior phrenic arteries, lumbar arteries, median sacral artery, gastroduodenal artery, and splenic artery provide necessary parietal branches.
Abdominal Veins
- The major abdominal vein is the inferior vena cava (IVC), which receives blood from the lower body, carrying it to the heart.
- The IVC formation occurs at the union of common iliac veins at L5 vertebral level, then ascends through the retroperitoneum on the right, passing behind the liver, and entering the heart's right atrium at the inferior thoracic region.
- Tributaries of the IVC include three anterior hepatic veins, three lateral (suprarenal, renal, and testicular/ovarian), five lateral abdominal wall, and three veins of origin (common iliac veins, median sacral veins).
Portal Venous System
The portal venous system carries blood from the digestive tract to the liver. This system consists of various veins, including the portal vein, superior and inferior mesenteric veins, and splenic vein. Crucially, it should be noted that the portal venous system differs from the systemic veins in its flow towards the liver, unlike systemic blood flow towards the heart.
Renal Veins
The renal veins carry blood from the kidneys to the inferior vena cava. The right renal vein typically flows directly into the posterior aspect of the IVC without significant tributaries.
Doppler Flow Patterns
- Abnormal portal vein flow patterns can be identified using Doppler examinations. A chronic obstruction of the portal vein, as well as various other conditions, can manifest with hepatofugal flow (opposite direction from normal, towards the liver).
- Various conditions, including liver cirrhosis, hepatic vein obstruction, and IVC blockage or prolonged heart failure, can contribute negatively toward the flow characteristic.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.