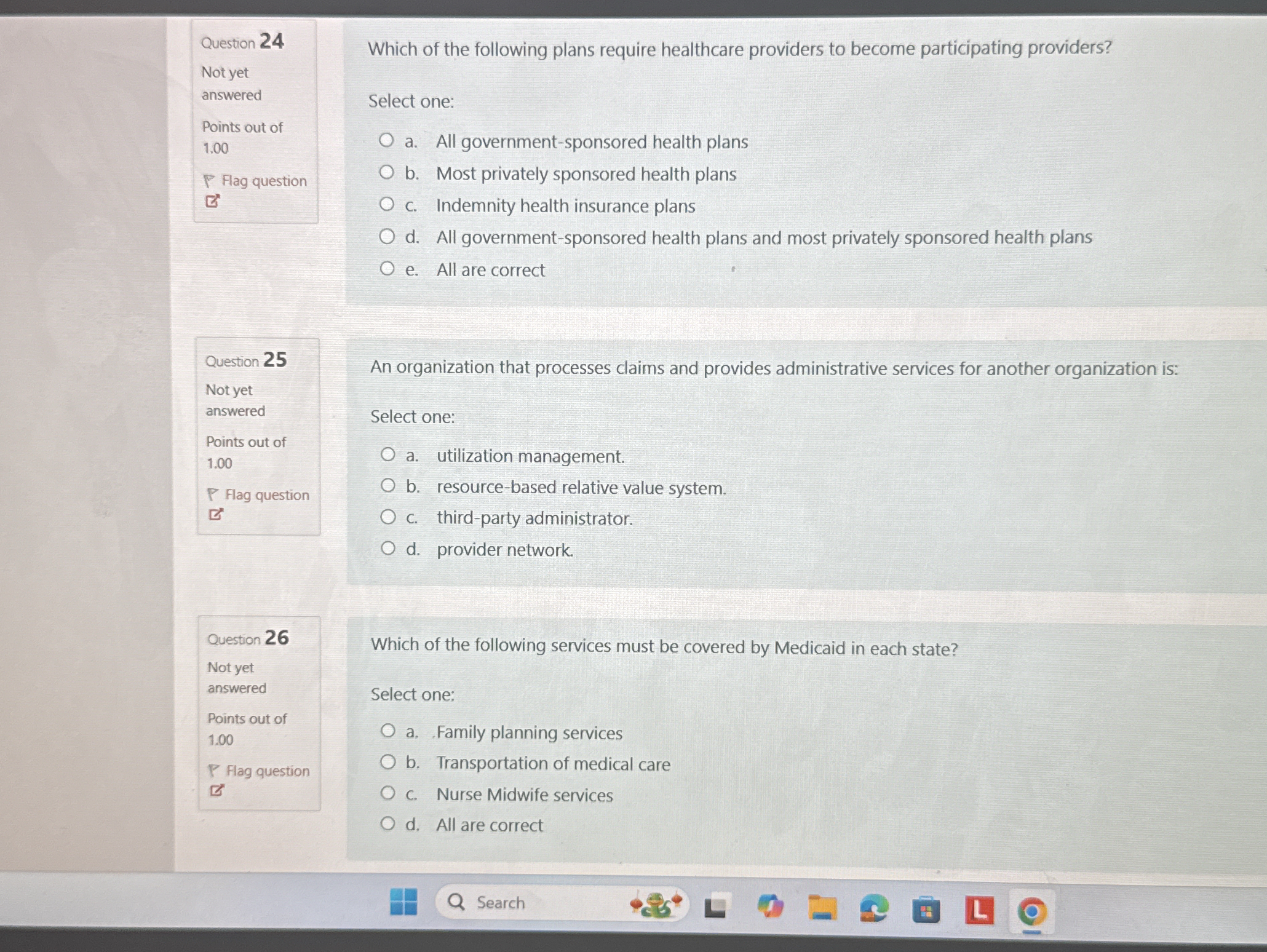
Which of the following plans require healthcare providers to become participating providers? An organization that processes claims and provides administrative services for another... Which of the following plans require healthcare providers to become participating providers? An organization that processes claims and provides administrative services for another organization is: Which of the following services must be covered by Medicaid in each state?
Understand the Problem
The image contains several multiple-choice questions related to healthcare plans and Medicaid coverage. It is presenting questions that seem to evaluate knowledge in healthcare administration and public health policies.
Answer
24: D, 25: C, 26: A
The answers are D, C, and A. Question 24: D (All government-sponsored health plans and most privately sponsored health plans). Question 25: C (third-party administrator). Question 26: A (Family planning services).
Answer for screen readers
The answers are D, C, and A. Question 24: D (All government-sponsored health plans and most privately sponsored health plans). Question 25: C (third-party administrator). Question 26: A (Family planning services).
More Information
In Medicaid, family planning services must be covered as they are federally mandated. Third-party administrators handle claims and administration, and many health plans require providers to be participating.
Tips
A common mistake is misunderstanding the required coverage items for Medicaid; ensure to check federally mandated services.
Sources
- Medicaid Administrative Claiming - medicaid.gov
- 10 Things to Know About Medicaid Managed Care - KFF - kff.org
- Provider payment and delivery systems - MACPAC - macpac.gov
AI-generated content may contain errors. Please verify critical information