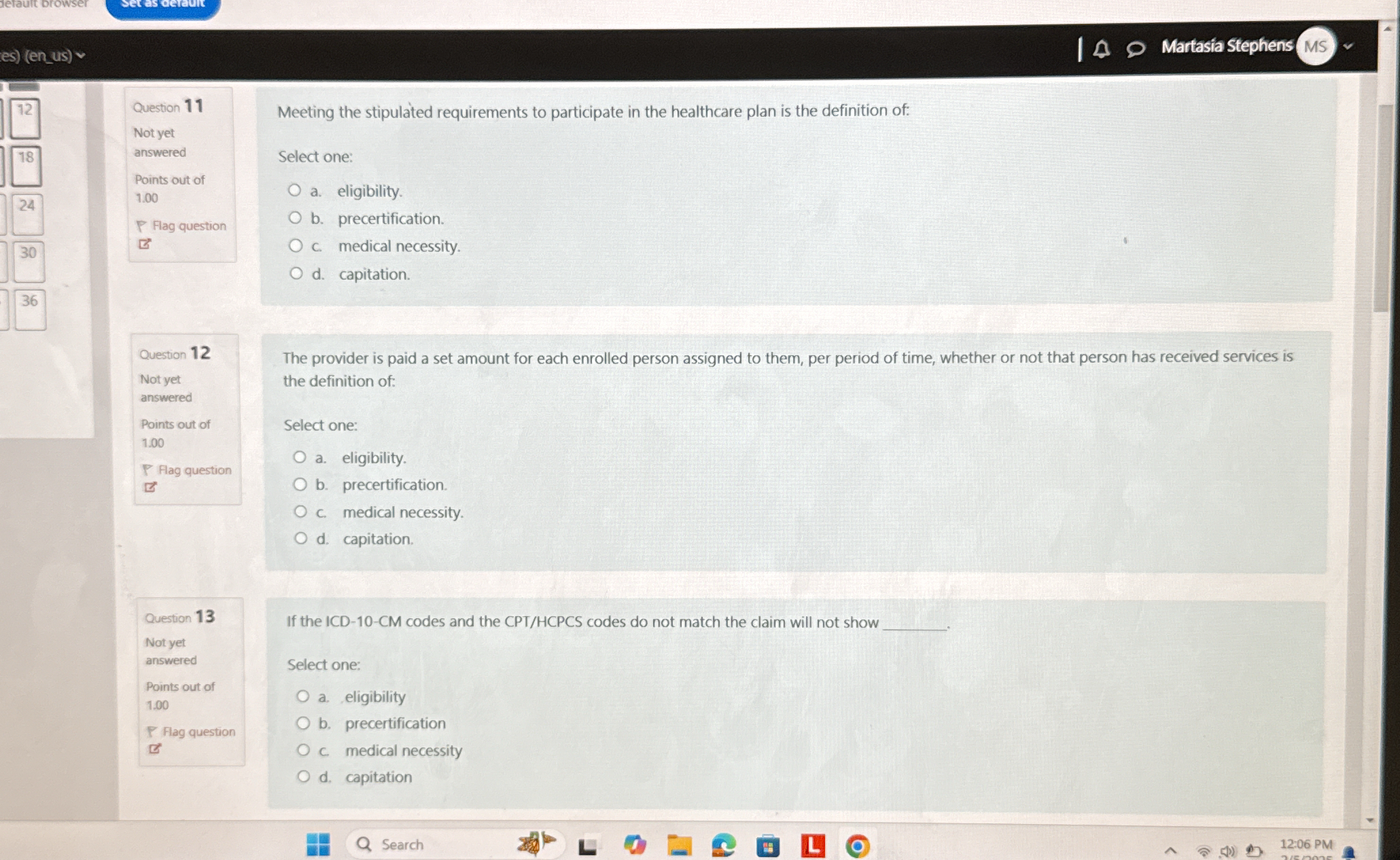
Meeting the stipulated requirements to participate in the healthcare plan is the definition of: Select one: a. eligibility b. precertification c. medical necessity d. capitation. T... Meeting the stipulated requirements to participate in the healthcare plan is the definition of: Select one: a. eligibility b. precertification c. medical necessity d. capitation. The provider is paid a set amount for each enrolled person assigned to them, per period of time, whether or not that person has received services is the definition of: Select one: a. eligibility b. precertification c. medical necessity d. capitation. If the ICD-10-CM codes and the CPT/HCPCS codes do not match the claim will not show: Select one: a. eligibility b. precertification c. medical necessity d. capitation.
Understand the Problem
The question presents multiple-choice queries related to healthcare terminology and concepts that determine various definitions and processes involved in healthcare plans and payments.
Answer
Eligibility; Capitation; Medical necessity.
Question 11: Eligibility. Question 12: Capitation. Question 13: Medical necessity.
Answer for screen readers
Question 11: Eligibility. Question 12: Capitation. Question 13: Medical necessity.
More Information
Eligibility refers to meeting requirements to join a healthcare plan. Capitation is a payment model where providers are paid per enrolled person. Medical necessity involves matching codes for claim approval.
Tips
A common mistake is confusing eligibility with medical necessity. Eligibility is about enrollment criteria, while medical necessity ensures care is appropriate.
AI-generated content may contain errors. Please verify critical information