Podcast
Questions and Answers
What is the primary reason for inserting drains near a wound?
What is the primary reason for inserting drains near a wound?
- To reduce swelling by absorbing excess fluid
- To facilitate wound healing by promoting drainage (correct)
- To monitor wound healing by collecting drainage
- To prevent infection by removing excess fluid
Increased pain and purulent drainage always indicate a delayed healing process.
Increased pain and purulent drainage always indicate a delayed healing process.
False (B)
What are the three main types of wound drainage described in the text?
What are the three main types of wound drainage described in the text?
Serous, sanguineous, and purulent
When a wound exhibits separation of its edges, it is referred to as ______.
When a wound exhibits separation of its edges, it is referred to as ______.
Match the wound care instructions with their corresponding benefit:
Match the wound care instructions with their corresponding benefit:
During which phase of wound healing does collagen synthesis peak?
During which phase of wound healing does collagen synthesis peak?
Scar tissue is more elastic than uninjured tissue.
Scar tissue is more elastic than uninjured tissue.
What are two important patient care considerations during the healing process?
What are two important patient care considerations during the healing process?
What effect do corticosteroids have on wound healing?
What effect do corticosteroids have on wound healing?
The final stage of healing begins about _____ weeks after the injury.
The final stage of healing begins about _____ weeks after the injury.
Chronic illnesses such as diabetes can impair wound healing.
Chronic illnesses such as diabetes can impair wound healing.
Which factor does NOT hinder wound healing?
Which factor does NOT hinder wound healing?
Match the phases of wound healing with their time frames and characteristics:
Match the phases of wound healing with their time frames and characteristics:
What is dehiscence?
What is dehiscence?
Overhydration of cells can lead to maceration.
Overhydration of cells can lead to maceration.
The presence of a __________ increases the risk for infection and fluid imbalances.
The presence of a __________ increases the risk for infection and fluid imbalances.
Which of the following patients is at higher risk for wound complications?
Which of the following patients is at higher risk for wound complications?
What happens to collagen during the maturation phase?
What happens to collagen during the maturation phase?
Match the wound complications with their descriptions:
Match the wound complications with their descriptions:
Patients undergoing __________ radiation therapy are at risk for delayed healing.
Patients undergoing __________ radiation therapy are at risk for delayed healing.
The appearance of a healing surgical wound should be swollen and deep red.
The appearance of a healing surgical wound should be swollen and deep red.
What type of wound is characterized by tearing of skin and tissue with blunt or irregular instruments?
What type of wound is characterized by tearing of skin and tissue with blunt or irregular instruments?
What is one of the primary reasons that edema interferes with wound healing?
What is one of the primary reasons that edema interferes with wound healing?
A clean-contaminated wound results from entry into a non-contaminated site.
A clean-contaminated wound results from entry into a non-contaminated site.
Infection aids the immune system's ability to repair and heal wounds.
Infection aids the immune system's ability to repair and heal wounds.
What is the process called that tissues undergo to heal after injury?
What is the process called that tissues undergo to heal after injury?
What are the two types of dead tissue that can delay wound healing?
What are the two types of dead tissue that can delay wound healing?
A ______ wound is characterized by the destruction of skin layers due to thermal, chemical, or irradiation factors.
A ______ wound is characterized by the destruction of skin layers due to thermal, chemical, or irradiation factors.
Adequate _____ is essential for wound healing and helps deliver nutrients and oxygen.
Adequate _____ is essential for wound healing and helps deliver nutrients and oxygen.
Match the type of wound with its description:
Match the type of wound with its description:
Which type of wound is defined as having devitalized tissue and possible fecal contamination?
Which type of wound is defined as having devitalized tissue and possible fecal contamination?
Match the nutrient to its role in wound healing:
Match the nutrient to its role in wound healing:
Abrasion is caused by a sharp instrument slicing through the skin.
Abrasion is caused by a sharp instrument slicing through the skin.
Which population is likely to heal more slowly due to physiological changes?
Which population is likely to heal more slowly due to physiological changes?
Obesity generally enhances the speed of wound healing.
Obesity generally enhances the speed of wound healing.
What is the primary distinction of a clean wound?
What is the primary distinction of a clean wound?
What types of wounds typically heal slowly?
What types of wounds typically heal slowly?
What occurs immediately after the initial injury during the hemostasis phase?
What occurs immediately after the initial injury during the hemostasis phase?
During the inflammatory phase, white blood cells primarily move to the wound site to ingest bacteria and cellular debris.
During the inflammatory phase, white blood cells primarily move to the wound site to ingest bacteria and cellular debris.
What substance do platelets release to stimulate other cells to migrate to the injury?
What substance do platelets release to stimulate other cells to migrate to the injury?
The phase known for the formation of granulation tissue is the ______ phase.
The phase known for the formation of granulation tissue is the ______ phase.
Which of the following is characterized by heat, redness, swelling, and pain at the injury site?
Which of the following is characterized by heat, redness, swelling, and pain at the injury site?
Match the following phases of wound healing with their characteristics:
Match the following phases of wound healing with their characteristics:
Macrophages enter the wound area immediately after an injury.
Macrophages enter the wound area immediately after an injury.
What is the primary role of fibroblasts during the proliferation phase?
What is the primary role of fibroblasts during the proliferation phase?
Flashcards
Incision
Incision
A wound caused by a cutting or sharp instrument with aligned edges.
Contusion
Contusion
A blunt instrument injury causing intact skin and possible bruising.
Abrasion
Abrasion
A scraping injury affecting the top layer of skin due to friction.
Laceration
Laceration
Signup and view all the flashcards
Puncture
Puncture
Signup and view all the flashcards
Penetrating wound
Penetrating wound
Signup and view all the flashcards
Pressure ulcers
Pressure ulcers
Signup and view all the flashcards
Clean contaminated wound
Clean contaminated wound
Signup and view all the flashcards
Hemostasis
Hemostasis
Signup and view all the flashcards
Exudate
Exudate
Signup and view all the flashcards
Inflammatory Phase
Inflammatory Phase
Signup and view all the flashcards
Leukocytes
Leukocytes
Signup and view all the flashcards
Macrophages
Macrophages
Signup and view all the flashcards
Proliferation Phase
Proliferation Phase
Signup and view all the flashcards
Fibroblasts
Fibroblasts
Signup and view all the flashcards
Granulation Tissue
Granulation Tissue
Signup and view all the flashcards
Collagen Synthesis
Collagen Synthesis
Signup and view all the flashcards
Maturation Phase
Maturation Phase
Signup and view all the flashcards
Healing Timeline
Healing Timeline
Signup and view all the flashcards
Scar Formation
Scar Formation
Signup and view all the flashcards
Factors Affecting Healing
Factors Affecting Healing
Signup and view all the flashcards
Desiccation Impact
Desiccation Impact
Signup and view all the flashcards
Maceration Impact
Maceration Impact
Signup and view all the flashcards
Trauma Effect
Trauma Effect
Signup and view all the flashcards
Edema
Edema
Signup and view all the flashcards
Infection
Infection
Signup and view all the flashcards
Necrosis
Necrosis
Signup and view all the flashcards
Age and Healing
Age and Healing
Signup and view all the flashcards
Circulation and Oxygenation
Circulation and Oxygenation
Signup and view all the flashcards
Nutritional Status
Nutritional Status
Signup and view all the flashcards
Wound Condition
Wound Condition
Signup and view all the flashcards
Role of Zinc
Role of Zinc
Signup and view all the flashcards
Wound Drainage
Wound Drainage
Signup and view all the flashcards
Types of Exudate
Types of Exudate
Signup and view all the flashcards
Signs of Infection
Signs of Infection
Signup and view all the flashcards
Dehiscence
Dehiscence
Signup and view all the flashcards
Patient Education on Wound Care
Patient Education on Wound Care
Signup and view all the flashcards
Corticosteroids
Corticosteroids
Signup and view all the flashcards
Radiation therapy
Radiation therapy
Signup and view all the flashcards
Immunosuppression
Immunosuppression
Signup and view all the flashcards
Evisceration
Evisceration
Signup and view all the flashcards
Fistula formation
Fistula formation
Signup and view all the flashcards
Wound assessment
Wound assessment
Signup and view all the flashcards
Infection signs
Infection signs
Signup and view all the flashcards
Study Notes
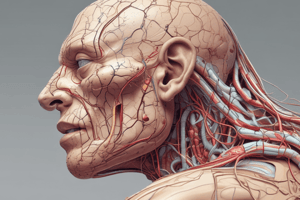
Wound Management
- Wound is defined as a break or disruption in the normal integrity of skin and tissues.
Learning Objectives
- Define wound
- Describe different types of wounds
- Describe the physiology of wound healing
- Identify factors affecting wound healing
- Outline wound complications
- Describe wound management
- Health educate patients on wound healing promotion
Types of Wounds
- Incision: Cutting or sharp instrument; wound edges are close to each other and aligned.
- Contusion: Blunt instrument; overlying skin remains intact; injury to underlying soft tissue; possible bruising, and/or hematoma.
- Abrasion: Friction; rubbing or scraping epidermal layers of skin; top layer of skin is abraded.
- Laceration: Tearing of skin and tissue with blunt or irregular instrument. Tissue is not aligned; often with loose flaps of skin and tissue.
- Puncture: Blunt or sharp instrument puncturing the skin; intentional (e.g., venipuncture), or accidental.
- Penetrating: Foreign object entering the skin or mucous membrane and lodging in underlying tissue. Fragments may scatter.
- Burns: (thermal, chemical, irradiation) destroy the layers of skin.
- Pressure ulcers: Compromised circulation secondary to pressure or pressure combined with friction.
Classifications of Wounds
-
Clean: Non-traumatic site, uninfected, no inflammation, no break in aseptic technique.
-
Clean-contaminated: Entry into respiratory, alimentary, genitourinary, or oropharyngeal tracts without unusual contamination. Minor break in aseptic technique; mechanical drainage.
-
Contaminated: Open, newly experienced traumatic wounds. Gross spillage from gastrointestinal tract. Major break in aseptic technique; entry into genitourinary or biliary tract when urine or bile is infected.
-
Dirty: Traumatic wound with delayed repair, devitalized tissue, foreign bodies, or fecal contamination. Acute inflammation and purulent drainage.
Physiology of Wound Healing
- Wound healing is a tissue response to injury.
- Mechanisms repair injured tissue by regenerating functioning cells and replacing connective tissue with scar tissue.
- Wound healing has phases.
Phases of Wound Healing
Phase 1: Hemostasis
- Occurs immediately after injury.
- Involved blood vessels constrict.
- Blood clotting begins through platelet activation and clustering.
- Blood vessels dilate after constriction.
- Increased capillary permeability allows plasma and blood components to leak out; forming exudate (liquid).
- Accumulation of exudates causes swelling, pain, increased perfusion results in heat and redness.
- Blood clot forms (hard scab) to protect the injury.
- Platelets release substances that stimulate other cells to participate in healing.
Phase 2: Inflammatory Phase
- Follows hemostasis.
- Lasts about 4-6 days.
- White blood cells move to the wound.
- Leukocytes arrive to ingest bacteria and cellular debris.
- Macrophages enter the wound area, about 24 hours after injury, and remain for an extended period.
- Macrophages ingest debris and release growth factors for epithelial cells and new blood vessels.
- Growth factors attract fibroblasts, which help fill in the wound.
- Acute inflammation characterized by pain, heat, redness, and swelling.
- Patient experience generalized body response; including mildly elevated temperature, leukocytosis (increased white blood cells), and generalized malaise.
Phase 3: Proliferative Phase
- Known as the fibroblastic or regenerative phase.
- Tissue formation to fill the wound gap.
- Primarily occurs through fibroblasts.
- Capillaries grow across the wound, providing oxygen and nutrients for continued healing.
- Fibroblasts form fibrin that stretches through the clot.
- Thin layer of epithelial cells forms across the wound.
- Blood flow resumes (reinstituted) across the wound.
- Granulation tissue formation (basis for scar tissue).
- Highly vascular, red, easily bleeds.
- Collagen synthesis and accumulation peak in 5-7 days.
- Collagen deposit continues for weeks or years depending on the wound size.
- Majority of white blood cells leave the wound area towards the end of the second week.
- Wound lighter in color (wound area).
Phase 4: Maturation Phase
- The final stage of healing.
- Begins about 3 weeks after injury.
- Continues for months or years.
- Collagen that was haphazardly deposited is remodeled for a stronger wound; like adjacent tissue.
- New collagen continuously deposited, which compresses blood vessels (in the healing wound).
- Scar (avascular collagen tissue) becomes flat and thin and does not sweat, grow hair, or tan.
- Scar tissue is strong but less elastic than uninjured tissue.
Factors Affecting Wound Healing
-
Local Factors:
- Pressure disrupts blood supply; interferes with blood flow to the tissue; delays healing.
- Desiccation (drying up): cells dehydrate and die in a dry environment; causes crusting; delays healing.
- Maceration (overhydration of cells): occurs due to moisture, pH of skin changes, overgrowth of bacteria and infection, and skin erosion from friction on moist skin.
-
Systemic factors:
- Age: Children and healthy adults heal faster; older adults have slowed fibroblastic activity and circulation, and more chronic illnesses; impede the healing process.
- Circulation and Oxygenation: Adequate blood flow is needed to deliver nutrients and oxygen; and to remove toxins, bacteria, and debris. Certain conditions (obesity) can affect the outcome of healing due to fat tissue hindering healing and elevating infection risk.
- Nutritional status: adequate proteins, carbohydrates, fats, vitamins (A & C), minerals, and calories essential for rebuilding cells. Zinc plays a role in proliferation. Poor nutrition and fluid balance can negatively affect wound healing.
-
Other factors: - Trauma: Repeated trauma to a wound area results in delayed healing.
- Edema: Edema at a wound site interferes with blood supply (to the area), resulting in an inadequate supply of oxygen and nutrients. - Infection:-Infection requires large amounts of energy from immune system to fight microorganisms; leaving little, or no reserve energy to focus on repair. Toxins from bacteria interfere with wound healing and cell death. - Necrotic tissue: Presence of necrotic or dead tissue in wound inhibits healing (slough, moist yellow stringy tissue and/or eschar).
Wound Complications
- Infection: Bacteria invades wound at time of trauma, surgery, or anytime after.
- Hemorrhage: Bleeding from a slipped suture, a dislodged clot, stress on the suture line, infection, or a blood vessel erosion by a foreign body (e.g., a drain).
- Dehiscence: Partial or total disruption of wound layers.
- Evisceration: Protrusion of viscera (organs) through the incision.
- Fistula formation: Abnormal passage from internal organ to skin, or internal organ to another; often from delayed healing; manifested by drainage; increases risk of infection, fluid, and electrolyte imbalances.
Nursing Management of Wound
- Assessment: Assess wound edges, color, condition (dehiscence or evisceration), drains, tubes, sutures, presence of infection.
- Drainage: Assess amount, color, odor, consistency, using wound, dressing, drainage bottles, or under patient.
- Pain: Pain can increase. Pain accompanied by increased drainage suggest delayed healing or infection.
Educating the Patients on Wound Care
- Keep wound dry and clean (and change dressings when necessary).
- Report any signs of infection (redness, swelling, tenderness, warmth around the wound, pus/discharge, and foul odor).
- Elevate affected part to heart level to reduce swelling.
- Dry cool packs or analgesics/pain medicine for pain.
- Plenty of food rich in protein and vitamin C should be consumed.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.