Podcast
Questions and Answers
What is defined as a wound?
What is defined as a wound?
- A break in the continuity of any body tissue (correct)
- A condition that affects the circulation of blood
- Any type of skin abrasion or cut
- An injury that involves only skin damage
Which phase is NOT included in the three primary phases of wound healing?
Which phase is NOT included in the three primary phases of wound healing?
- Maturation
- Proliferation (or repair)
- Haemostasis (correct)
- Inflammation & Debridement
What influences the speed and completeness of wound healing?
What influences the speed and completeness of wound healing?
- Stress levels alone
- Nutritional status and age (correct)
- Environmental temperature only
- The use of antibiotics only
Which of the following statements about wounds is true?
Which of the following statements about wounds is true?
Which of the following best describes the phase of inflammation in wound healing?
Which of the following best describes the phase of inflammation in wound healing?
What is one of Halsted’s principles related to surgical technique?
What is one of Halsted’s principles related to surgical technique?
Which condition would suggest a need for delayed closure of a wound?
Which condition would suggest a need for delayed closure of a wound?
Why is preserving blood supply to a wound vital?
Why is preserving blood supply to a wound vital?
What does the 'golden period' refer to in wound care?
What does the 'golden period' refer to in wound care?
What should be considered about a patient's condition when assessing a wound?
What should be considered about a patient's condition when assessing a wound?
What factor is NOT critical when applying Halsted’s principles?
What factor is NOT critical when applying Halsted’s principles?
What is a common reason for excessive tension when attempting wound closure?
What is a common reason for excessive tension when attempting wound closure?
What effect does necrotic tissue have on wound healing?
What effect does necrotic tissue have on wound healing?
What is the primary function of granulation tissue?
What is the primary function of granulation tissue?
During which phase does myofibroblast contraction primarily lead to a reduction in wound size?
During which phase does myofibroblast contraction primarily lead to a reduction in wound size?
What significant structural change occurs during the maturation/remodeling phase of wound healing?
What significant structural change occurs during the maturation/remodeling phase of wound healing?
What might prevent contraction of the wound in the proliferative phase?
What might prevent contraction of the wound in the proliferative phase?
How long does the maturation/remodeling phase typically last?
How long does the maturation/remodeling phase typically last?
What is the role of fibroblasts in the wound healing process?
What is the role of fibroblasts in the wound healing process?
Which of the following is NOT a characteristic of granulation tissue?
Which of the following is NOT a characteristic of granulation tissue?
What clinical actions should be taken during the inflammation phase of wound healing?
What clinical actions should be taken during the inflammation phase of wound healing?
What occurs after three to five days post-injury in the wound healing process?
What occurs after three to five days post-injury in the wound healing process?
What is a potential consequence of excessive tension on a wound during contraction?
What is a potential consequence of excessive tension on a wound during contraction?
What phase occurs immediately after an elective wound is incurred?
What phase occurs immediately after an elective wound is incurred?
How does skin healing compare to fascia healing?
How does skin healing compare to fascia healing?
What is a consequence of poor nutritional status in patients during wound healing?
What is a consequence of poor nutritional status in patients during wound healing?
What is one of the factors that can affect wound healing at the wound level?
What is one of the factors that can affect wound healing at the wound level?
What surgical technique can enhance wound healing?
What surgical technique can enhance wound healing?
What effect do NSAIDs have on wound healing?
What effect do NSAIDs have on wound healing?
How does the bursting strength of an anastomosis change post-surgery?
How does the bursting strength of an anastomosis change post-surgery?
What is the recommended distance for sutures from the wound edge for proper security?
What is the recommended distance for sutures from the wound edge for proper security?
What is an effect of the removal of subcutaneous tissue on granulation tissue production?
What is an effect of the removal of subcutaneous tissue on granulation tissue production?
What is a key consideration for managing closed vs. open wounds?
What is a key consideration for managing closed vs. open wounds?
What is the primary function of the haemostatic plug in the early stages of wound healing?
What is the primary function of the haemostatic plug in the early stages of wound healing?
Which type of leukocyte is the first to migrate into the wound after an injury?
Which type of leukocyte is the first to migrate into the wound after an injury?
During which stage of wound healing do fibroblasts transform into myofibroblasts?
During which stage of wound healing do fibroblasts transform into myofibroblasts?
What signs indicate the presence of inflammation as part of the healing process?
What signs indicate the presence of inflammation as part of the healing process?
Which of the following cytokines is associated with the vasodilation process during inflammation?
Which of the following cytokines is associated with the vasodilation process during inflammation?
What is the role of macrophages in wound healing?
What is the role of macrophages in wound healing?
What type of tissue initially fills the wound during the proliferative phase?
What type of tissue initially fills the wound during the proliferative phase?
How does angiogenesis contribute to wound healing?
How does angiogenesis contribute to wound healing?
What happens to collagen type III as the wound stabilizes?
What happens to collagen type III as the wound stabilizes?
What is a potential consequence of systemic inflammation during the wound healing process?
What is a potential consequence of systemic inflammation during the wound healing process?
How does the process of epithelialization occur in large wounds?
How does the process of epithelialization occur in large wounds?
During which phase is the provisional extracellular matrix (ECM) formed?
During which phase is the provisional extracellular matrix (ECM) formed?
What triggers the intrinsic coagulation cascade in response to endothelial damage?
What triggers the intrinsic coagulation cascade in response to endothelial damage?
What is the primary goal of debridement in the wound healing process?
What is the primary goal of debridement in the wound healing process?
Flashcards
What is a wound?
What is a wound?
A disruption in the continuity of any body tissue.
Haemostasis
Haemostasis
The first stage of wound healing involving clotting and inflammation.
Proliferation
Proliferation
The second stage of wound healing where new cells are made to fill the wound and rebuild tissue.
Maturation
Maturation
Signup and view all the flashcards
Healing
Healing
Signup and view all the flashcards
Gentle Tissue Handling
Gentle Tissue Handling
Signup and view all the flashcards
Meticulous Control of Haemorrhage
Meticulous Control of Haemorrhage
Signup and view all the flashcards
Strict Asepsis
Strict Asepsis
Signup and view all the flashcards
Elimination of Dead Space
Elimination of Dead Space
Signup and view all the flashcards
Accurate Tissue Apposition
Accurate Tissue Apposition
Signup and view all the flashcards
Minimal Tension
Minimal Tension
Signup and view all the flashcards
Golden Period
Golden Period
Signup and view all the flashcards
Factors Affecting Wound Healing
Factors Affecting Wound Healing
Signup and view all the flashcards
Granulation Tissue
Granulation Tissue
Signup and view all the flashcards
Wound Contraction
Wound Contraction
Signup and view all the flashcards
Proliferative Phase
Proliferative Phase
Signup and view all the flashcards
Wound Maturation/Remodeling
Wound Maturation/Remodeling
Signup and view all the flashcards
Remodeling Phase
Remodeling Phase
Signup and view all the flashcards
Days 3-10 post injury
Days 3-10 post injury
Signup and view all the flashcards
Wound Strength
Wound Strength
Signup and view all the flashcards
Maturation Phase
Maturation Phase
Signup and view all the flashcards
Managing Inflammation in Traumatic Wounds
Managing Inflammation in Traumatic Wounds
Signup and view all the flashcards
Managing Proliferation in Traumatic Wounds
Managing Proliferation in Traumatic Wounds
Signup and view all the flashcards
Inflammatory Phase
Inflammatory Phase
Signup and view all the flashcards
Weak Wound Seal
Weak Wound Seal
Signup and view all the flashcards
Skin Healing vs. Fascia Healing
Skin Healing vs. Fascia Healing
Signup and view all the flashcards
First Do No Harm & Healing Will Occur
First Do No Harm & Healing Will Occur
Signup and view all the flashcards
Wound Healing in Cats
Wound Healing in Cats
Signup and view all the flashcards
Wound Healing in Dogs
Wound Healing in Dogs
Signup and view all the flashcards
Wound Factors
Wound Factors
Signup and view all the flashcards
Patient Factors
Patient Factors
Signup and view all the flashcards
Surgeon Factors
Surgeon Factors
Signup and view all the flashcards
Inflammation Stage
Inflammation Stage
Signup and view all the flashcards
Leukocytes
Leukocytes
Signup and view all the flashcards
Neutrophils
Neutrophils
Signup and view all the flashcards
Monocytes
Monocytes
Signup and view all the flashcards
Macrophages
Macrophages
Signup and view all the flashcards
Debridement
Debridement
Signup and view all the flashcards
Angiogenesis
Angiogenesis
Signup and view all the flashcards
Fibroplasia
Fibroplasia
Signup and view all the flashcards
Epithelialization
Epithelialization
Signup and view all the flashcards
Chronic Wound
Chronic Wound
Signup and view all the flashcards
Study Notes
Learning Objectives
- Students should be able to demonstrate an understanding of the phases of wound healing
- Students should be able to describe influences on the speed and completeness of wound healing
What is a Wound?
- A wound is a break in the continuity of any body tissue
- A wound does not always mean broken skin
- Wounds can be created through surgical procedures
Healing
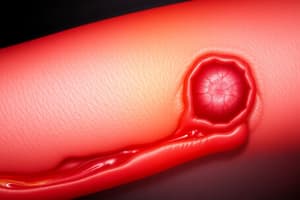
- Images displayed show examples of wounds in various stages of healing
Stages of Wound Healing
- Wound healing is divided into three overlapping phases: Inflammation, Proliferation, and Maturation/Remodeling
- Some texts describe four stages, including haemostasis as a stage within inflammation
- Inflammation & Debridement:
- Haemostasis
- Proliferation (or repair)
- Maturation and Remodel
- Microscopic events allow the wound to heal
- The macroscopic appearance of the wound gives insights into the stage of healing
Inflammation & Haemostasis
- Inflammatory phase starts with haemostasis
- First few minutes after injury
- Damage to blood vessels
- Blood and lymph escape, filling the wound
- Cleansing and preventing further contamination
- Reflex vasoconstriction (catecholamines, serotonin, bradykinin, histamine)
- Reduces blood loss
- Endothelial damage activates platelets, resulting in a platelet plug
- Vasodilation
- Increase in oxygen, white blood cells, and proteins to the area
- Endothelial damage exposes tissue factor
- Intrinsic coagulation cascade
- Fibrin plug forms
- Blood clot
- Barriers to infection
- Prevents further fluid loss
- Provisional Extracellular Matrix (ECM) framework
- Binding sites for neutrophils, macrophages and connective tissue cells
- Minimal wound strength but stabilises wound edges
- Dries to form scab
- Allows healing of deeper tissues
Inflammation & Debridement
- Migration of leukocytes into the wound within 6 hours
- Neutrophils (0-48 hours):
- Destroy bacteria
- Phagocytose
- Release toxic oxygen species (NO)
- Cause vasodilation
- Component of pus
- Monocytes (48-72 hours):
- Essential for wound healing
- Transform into activated macrophages
- Phagocytose/destroy bacteria
- Remove clot
- Debride necrotic tissue by phagocytosis and release enzymes (collagenase)
- Produce pro-inflammatory mediators
- Stimulates repair (growth factors)
- Fibroplasia (tissue repair)
- Angiogenesis (formation of new blood vessels)
- Epithelialisation
Gross Signs of Inflammation
- Heat, redness, swelling, pain, loss of function
- Open wound, blood clots, pus/serosanguineous discharge
- Vasodilation
- Increased permeability/extravasation of fluid
- Obstruction of lymphatic channels
- Stimulation of nerve endings due to pressure, stretching, or chemical stimulation (bradykinin)
Chronic Wounds
- Big inflammatory focus
- Not enough proteins/leukocytes for proper inflammatory response throughout the area
- Prolonged pro-inflammatory phase
- Persistent inflammatory focus
- Systemic inflammatory effects (SIRS)
- Continued vasodilation → hypotension
- CVS changes (tachycardia, vasoconstriction of non-essential organs = GIT)
- Barrier of GIT reduced
- Bacteria translocate into the Liver
- Hepatic inflammation → further systemic inflammation
- Renal failure, hepatic failure (MODS)
- Inappropriate Coagulation (DIC)
- Brain starved of nutrients
- Death
Summary of Inflammation and Debridement Stage
- Occurs immediately after the wound is created
- Generally lasts 2-5 days, though can be longer
- Immediate haemostasis (5-10 minutes) as platelets form a plug
- Acts as a barrier for further contamination
- Later, vasodilation occurs
- Neutrophils first, followed by monocytes which become tissue macrophages after 46-96 hours
- macrophages stimulate repair (fibroplasia, angiogenesis, epithelialisation)
- Debride necrotic tissue and phagocytose bacteria
Proliferation and Repair
- Restores skin integrity by filling the wound with new tissue
- Angiogenesis
- Fibroplasia
- Epithelialisation
- Granulation tissue
- Contraction
Proliferation: Fibroplasia
- Fibroblasts proliferate and migrate into the wound
- Differentiate into myofibroblasts
- Migrate along the extracellular matrix
- Synthesise collagen
- Initially collagen in the wound is Type III
- Type I collagen is stronger than Type III
- Once the wound is stable, fibroblasts stop producing collagen
- Capillaries regress and granulation tissue becomes a scar
- Requires oxygen and nutrition; perfusion must be good
Proliferation: Angiogenesis
- New capillaries form from existing vessels at the wound edges
- Endothelial cells migrate into the ECM
- Capillaries are fragile and highly permeable
Proliferation: Epithelialisation
- Migration of epidermal cells at the margin of the wound
- Proliferation of epidermal cells behind the leading edges
- Epidermis can only come from wound margins after granulation tissue has formed
- New epidermis may be visible 4-5 days after wounding
- In large wounds, healing may not complete in the middle
- Can be thin and easily traumatized in the middle of large wounds
- Adnexal structures do not regenerate
- Pigmentation is variable
- Healing occurs side to side, not top to bottom; long incisions heal as fast as short ones
Proliferation: Granulation Tissue
- Combination of new capillaries, fibroblasts, and connective tissue
- Fills wound beneath the scab/bandage
- Protects the wound
- No active dressing needed
- Barrier to infection
- No further antibiotics needed
- Surface for epithelialisation
- Contains myofibroblasts (help with contraction)
- Occurs (transition from ECM) ~4-5 days after injury
- Can take weeks to fill a large wound
Proliferation: Contraction
- Days 5-9 post injury
- Reduction in wound size
- Contraction of myofibroblasts
- Surrounding skin stretches (may look stellate)
- Can be a problem over joints/body openings
- Loss of function
- Continues until wound edges meet
- Negative feedback
- May cease if tension in surrounding tissue is too high
Summary of Proliferative Phase
- Occurs between days 4-21, dependent on contamination
- Fibroblasts enter the wound
- These can differentiate to myofibroblasts
- Collagen is formed
- Angiogenesis/neovascularisation occurs
- This results in the formation of new epithelium and fibrous tissue
- This will contract and lead to closure of the wound
Maturation/Remodelling
- Increases mechanical strength of the wound
- Reorganization of connective tissue
- Rearrangement of collagen bundles - crosslinking
- Reduction in collagen content
- Remodelling takes years
- Rate of remodelling differs between tissues
- Initial wound strength is weak (sutures, fibrin clot, epithelialisation)
- After 3-5 days, granulation tissue contributes (friable)
- After 7-10 days, collagen and scar tissue are present
Wound Strength Over Time
- Wound strength increases over time
- Inflammatory/debridement phase: low strength
- Repair/proliferative phase: moderate strength
- Maturation phase: high strength
- 80% normal strength after 1-2 years
Wound Healing Phases
- Vasoconstriction
- Vasodilation
- Inflammatory phase
- Cellular response
- Proliferative phase
- Re-epithelialisation
- Fibroplasia: collagen synthesis
- Wound contraction
- Maturation/remodelling phase
- Scar: collagen remodelling
Factors Affecting Wound Healing: Cats vs. Dogs
- 7 days post-skin incision
- Cat wound bursting strength is ~50% of dog's
- Granulation tissue appears slower in cats (6.3 days), compared to dogs (4.5 days)
- Time to cover wound completely with granulation tissue is longer in cats (19 days) than in dogs (7.5 days)
- Removal of subcutaneous tissue significantly reduces granulation tissue production in both species
Factors Affecting Wound Healing - Wound Factors
- Type of injury (forces applied); trauma vs. surgery
- Perfusion, blood supply, tissue viability, haematoma/seroma
- Contamination
- Anatomical location
- Movement, pressure, skin tension/availability
- Neoplasia
- Following tumor resections
Factors Affecting Wound Healing: Patient Factors
- Concurrent trauma
- Hypovolemic shock
- Poor nutritional status
- Other life-threatening injuries
- Consumption of platelets
- Pre-existing concurrent disease: Diabetes mellitus, hypothyroidism, HAC, infection, anaemia/coagulopathies, uraemia, hypoproteinaemia/poor nutrition, neoplasia
- Obesity
- Current medication: Immunosuppressive drugs/chemotherapy, radiation therapy
- Species: cat vs dog
- Wound interference
Factors Affecting Wound Healing: Surgeon Factors
- Technique: appropriate debridement, choice of lavage solution or an open wound management, Halsted's principles (meticulous haemostasis, obliteration of dead space, tension-free apposition of tissues), judicious and appropriate use of anti-microbials, avoiding prolonged anaesthesia and keeping surgical time as short as possible
- Decision-making in wound treatment
- Manage open vs. closed
- Type of closure
Fascia
- Slow healing due to fewer blood vessels
- No strength from healing tissue for 1-2 weeks (just sutures)
- Active zone up to 2 mm away from wound
- Sutures should be ~3 mm away from wound edge for security
Gastrointestinal Tract
- Anastomosis bursting strength decreases over first 48 hours
- Weakened tissue during inflammatory phase of healing allows for dehiscence (peristalsis)
- Lag phase; 3-5 days post-surgery
- Pre-existing septic peritonitis: less suture-holding capacity; already weakened at time of surgery
- Perfusion to anastomosis site is key
- CARE with drugs – NSAIDS – Can delay healing
- These patients often have hypoproteinaemia
Decision-Making with a Wound
- Can we attempt primary closure?
- Can we apply Halsted's principles?
- Would healing by granulation be a better option?
- Good communication with the owner is imperative.
What are Halsted's Principles?
- Gentle tissue handling
- Meticulous control of haemorrhage
- Strict asepsis
- Elimination of dead space
- Accurate tissue apposition
- Minimal tension
Underlying Disease for Healing?
- Does the patient have underlying disease conditions that could affect healing?
- Is it on any drugs that could affect healing?
- How long ago did this wound occur? (Golden period up to 6 hours)
- Was there blunt trauma?
- Was there a sharp penetration?
When Consider Delayed Closure?
- Long time since wounding (>6 hrs/golden period)
- Presence of gross contamination or infection
- Presence of necrotic tissue/devitalised/disrupted blood supply to skin edges/crushing injury
- Excessive tension on surrounding skin with attempted closure
- Excessive skin defect/degloving
Why is Blood Supply Important?
- Preserves blood supply, brings oxygen and leucocytes to the wound
- Leucocytes (neutrophils, monocytes, T-cells, B-cells, platelets) support tissue macrophages
- Tissue macrophages are essential for inflammatory response
- Provides acute phase proteins (complement and antibodies) that combat infection
- Fluid medium for inflammatory cells
- Maintains glucose delivery and metabolic waste removal
- Allows systemic response to inflammation (e.g., hyperthermia)
References
- BSAVA Manual of Canine and Feline Wound Management and Reconstruction
- Veterinary Clinics Small Animal Practice
- Stages of Wound Healing and Their Clinical Relevance
- Giselle Hosgood, BVSc, MS, PhD
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.