Podcast
Questions and Answers
Which of the following best describes the role of the urinary system in waste excretion?
Which of the following best describes the role of the urinary system in waste excretion?
- Secretion of sweat to eliminate salts.
- Excretion of carbon dioxide from metabolism.
- Elimination of bile and pigments.
- Removal of urea, salts, water, and soluble waste products. (correct)
Which of the following is the best definition of diuresis?
Which of the following is the best definition of diuresis?
- The removal of excess fluid from the body. (correct)
- The production of concentrated urine.
- The process of conserving water in the body.
- The state of producing no urine.
How do the kidneys contribute to the maintenance of acid-base balance in the body?
How do the kidneys contribute to the maintenance of acid-base balance in the body?
- By secreting waste products into urine.
- By producing erythropoietin.
- By removing hydrogen and bicarbonate ions via the urine. (correct)
- By regulating the release of ADH.
What is the role of erythropoietin, produced by specialized renal cells, in maintaining homeostasis?
What is the role of erythropoietin, produced by specialized renal cells, in maintaining homeostasis?
Which of the following is the correct anatomical relationship of the kidneys in most domestic species (excluding pigs)?
Which of the following is the correct anatomical relationship of the kidneys in most domestic species (excluding pigs)?
What is the significance of the renal hilus?
What is the significance of the renal hilus?
Which of the following describes the function of the renal pelvis?
Which of the following describes the function of the renal pelvis?
What structural characteristic distinguishes the kidneys of cattle from those of dogs, horses, and cats?
What structural characteristic distinguishes the kidneys of cattle from those of dogs, horses, and cats?
Which component of the nephron is responsible for the first stage of urine production through blood filtration?
Which component of the nephron is responsible for the first stage of urine production through blood filtration?
What is the primary importance of the brush border in the proximal convoluted tubule (PCT)?
What is the primary importance of the brush border in the proximal convoluted tubule (PCT)?
How does the structure of the loop of Henle change as it makes its U-turn?
How does the structure of the loop of Henle change as it makes its U-turn?
What is the influence of ADH (antidiuretic hormone) on the collecting ducts?
What is the influence of ADH (antidiuretic hormone) on the collecting ducts?
How does the unique arrangement of efferent and afferent arterioles in the glomerulus contribute to its function?
How does the unique arrangement of efferent and afferent arterioles in the glomerulus contribute to its function?
What structural feature of the glomerular capillaries facilitates the transfer of plasma?
What structural feature of the glomerular capillaries facilitates the transfer of plasma?
Why is the presence of protein in the urine considered abnormal?
Why is the presence of protein in the urine considered abnormal?
What is the primary factor affecting glomerular filtration rate (GFR)?
What is the primary factor affecting glomerular filtration rate (GFR)?
How does the body reabsorb essential substances from the glomerular filtrate?
How does the body reabsorb essential substances from the glomerular filtrate?
Which transport mechanism is primarily responsible for reabsorbing glucose and amino acids in the proximal convoluted tubule (PCT)?
Which transport mechanism is primarily responsible for reabsorbing glucose and amino acids in the proximal convoluted tubule (PCT)?
How does aldosterone influence sodium reabsorption in the distal convoluted tubule (DCT) and collecting duct?
How does aldosterone influence sodium reabsorption in the distal convoluted tubule (DCT) and collecting duct?
What happens to the concentration of other substances in the tubular filtrate once water is reabsorbed?
What happens to the concentration of other substances in the tubular filtrate once water is reabsorbed?
What is the purpose of tubular secretion in the kidneys?
What is the purpose of tubular secretion in the kidneys?
What determines urine volume?
What determines urine volume?
What type of epithelium lines the ureters and urinary bladder, allowing them to stretch as urine passes through or accumulates?
What type of epithelium lines the ureters and urinary bladder, allowing them to stretch as urine passes through or accumulates?
How do the ureters prevent urine from backing up into the kidneys as the bladder fills?
How do the ureters prevent urine from backing up into the kidneys as the bladder fills?
What triggers the muscle contraction step in the process of urination?
What triggers the muscle contraction step in the process of urination?
What is the primary difference between the male and female urethra, besides length and location?
What is the primary difference between the male and female urethra, besides length and location?
Why is the kidney considered to be in the retroperitoneal space?
Why is the kidney considered to be in the retroperitoneal space?
What is the significance of perirenal fat surrounding the kidneys?
What is the significance of perirenal fat surrounding the kidneys?
Which hormone helps to stimulate red blood cell production?
Which hormone helps to stimulate red blood cell production?
Where does tubular reabsorption occur?
Where does tubular reabsorption occur?
What percentage of the blood pumped by the heart goes to the kidneys?
What percentage of the blood pumped by the heart goes to the kidneys?
Where is the only place in the body where blood entering and leaving the capillaries is oxygenated?
Where is the only place in the body where blood entering and leaving the capillaries is oxygenated?
What is the term for the functional units of the kidneys?
What is the term for the functional units of the kidneys?
Which of the following is NOT something that each nephron does?
Which of the following is NOT something that each nephron does?
Where is the visceral layer located?
Where is the visceral layer located?
What is the main purpose of the distal convoluted tubule (DCT)?
What is the main purpose of the distal convoluted tubule (DCT)?
The mobility of the left kidney leaves it vulnerable to what?
The mobility of the left kidney leaves it vulnerable to what?
Aside from urine excretion, what other system process do the kidneys play an important role in?
Aside from urine excretion, what other system process do the kidneys play an important role in?
How does ADH (antidiuretic hormone) contribute to fluid balance regulation within the kidney?
How does ADH (antidiuretic hormone) contribute to fluid balance regulation within the kidney?
What is the functional significance of the unique arrangement of blood vessels in the kidney, where blood entering and leaving the capillaries is oxygenated?
What is the functional significance of the unique arrangement of blood vessels in the kidney, where blood entering and leaving the capillaries is oxygenated?
How do the kidneys respond to a state of acidosis (low blood pH) in the body?
How do the kidneys respond to a state of acidosis (low blood pH) in the body?
Under what circumstances might protein be present in the urine (proteinuria), and what does it indicate?
Under what circumstances might protein be present in the urine (proteinuria), and what does it indicate?
How do the unique structural characteristics of the transitional epithelium in the ureters and bladder contribute to their function?
How do the unique structural characteristics of the transitional epithelium in the ureters and bladder contribute to their function?
Flashcards
Waste Excretion
Waste Excretion
The metabolic processes produce waste products (carbon dioxide, nitrogenous wastes, bile salts, salts) that must be excreted.
Routes of Elimination
Routes of Elimination
Routes by which waste products are removed from the body. (respiratory tract, sweat glands, digestive system, and urinary system)
Urinary System Parts
Urinary System Parts
Two kidneys, two ureters, one urinary bladder, and one urethra.
Kidneys Role
Kidneys Role
Signup and view all the flashcards
Kidney Functions
Kidney Functions
Signup and view all the flashcards
Urine Production
Urine Production
Signup and view all the flashcards
Diuresis
Diuresis
Signup and view all the flashcards
Oliguria and Anuria
Oliguria and Anuria
Signup and view all the flashcards
Main control of fluid balance
Main control of fluid balance
Signup and view all the flashcards
Acid-Base Balance
Acid-Base Balance
Signup and view all the flashcards
Hormone Regulation by Kidneys
Hormone Regulation by Kidneys
Signup and view all the flashcards
Erythropoietin
Erythropoietin
Signup and view all the flashcards
Prostaglandin
Prostaglandin
Signup and view all the flashcards
Kidneys Location
Kidneys Location
Signup and view all the flashcards
Kidney Position
Kidney Position
Signup and view all the flashcards
Kidney Appearance
Kidney Appearance
Signup and view all the flashcards
Hilus
Hilus
Signup and view all the flashcards
Renal Pelvis
Renal Pelvis
Signup and view all the flashcards
Renal Cortex
Renal Cortex
Signup and view all the flashcards
Renal Medulla
Renal Medulla
Signup and view all the flashcards
Calyx
Calyx
Signup and view all the flashcards
Nephrons
Nephrons
Signup and view all the flashcards
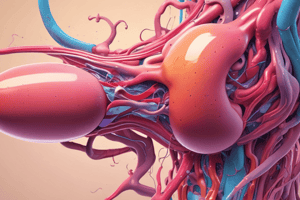
Renal Corpuscle
Renal Corpuscle
Signup and view all the flashcards
Glomerulus
Glomerulus
Signup and view all the flashcards
Bowman's Capsule
Bowman's Capsule
Signup and view all the flashcards
Renal Corpuscle Function
Renal Corpuscle Function
Signup and view all the flashcards
After blood is filtered, fluid becomes what?
After blood is filtered, fluid becomes what?
Signup and view all the flashcards
PCT Lining
PCT Lining
Signup and view all the flashcards
Loop of Henle
Loop of Henle
Signup and view all the flashcards
After the filtrate flows through the Loop of Henle where does it flow next?
After the filtrate flows through the Loop of Henle where does it flow next?
Signup and view all the flashcards
Collecting Ducts
Collecting Ducts
Signup and view all the flashcards
Kidney Control
Kidney Control
Signup and view all the flashcards
Renal Blood Supply
Renal Blood Supply
Signup and view all the flashcards
What are the Renal Capillaries located in between?
What are the Renal Capillaries located in between?
Signup and view all the flashcards
Afferent Glomerular Arterioles Carry to
Afferent Glomerular Arterioles Carry to
Signup and view all the flashcards
Glomerular Capillaries
Glomerular Capillaries
Signup and view all the flashcards
Efferent Glomerular Arterioles Carry
Efferent Glomerular Arterioles Carry
Signup and view all the flashcards
Oxygenated Capillaries
Oxygenated Capillaries
Signup and view all the flashcards
Peritubular Capillaries
Peritubular Capillaries
Signup and view all the flashcards
Mechanisms of Renal Action
Mechanisms of Renal Action
Signup and view all the flashcards
Blood Filtration
Blood Filtration
Signup and view all the flashcards
Glomerular Filtration Rate (GFR)
Glomerular Filtration Rate (GFR)
Signup and view all the flashcards
Reabsorption
Reabsorption
Signup and view all the flashcards
ADH (Antidiuretic Hormone)
ADH (Antidiuretic Hormone)
Signup and view all the flashcards
Aldosterone function
Aldosterone function
Signup and view all the flashcards
Study Notes
Waste Excretion
- Metabolic processes produce waste that must be excreted
- Waste products include carbon dioxide, nitrogenous wastes, bile salts and pigments, and salts
- Carbon dioxide is excreted through the lungs
- Nitrogenous wastes, particularly urea, are excreted from protein metabolism
- Bile salts and pigments result from red cell breakdown
- Salts derive from tissue breakdown and excess consumption
Routes of Waste Elimination
- The respiratory tract eliminates carbon dioxide and water vapor
- Sweat glands eliminate salts
- The digestive system removes bile and pigments
- The urinary system removes urea, salts, water, and soluble waste products
- The kidneys can remove drug metabolites made water-soluble by hepatic enzymes
Components of the Urinary System
- Two kidneys
- Two ureters
- One urinary bladder (absent in birds and reptiles: urine flows directly to the colon)
- One urethra
Kidney Function
- "Nephro-" and "Reno-" are parts of medical terms for kidneys
- The kidneys produce urine for excretion and play a role in homeostasis
- Kidneys regulate plasma composition, acid-base status, and fluid and electrolyte balance
- Maintaining homeostasis is the kidneys' most vital function
Homeostasis
- Blood filtration, reabsorption and secretion are essential for this
- Useful substances are returned to circulation
- Waste products are secreted from circulation into urine
Regulation of Fluids
- The amount of urine produced affects the amount of water in the body
- Diuresis removes excess fluid
- Oliguria (little urine) and anuria (no urine) are ways of conserving water
- Anuric renal failure compromises fluid balance
Primary fluid control
- Controlled by antidiuretic hormone (ADH) from the pituitary gland
- Controlled by aldosterone from the adrenal glands
Acid-Base Balance
- Kidneys remove hydrogen and bicarbonate ions which alters blood pH levels
- Hydrogen ions make blood more acidic
- Bicarbonate ions makes blood more alkaline
Hormones
- Kidneys help regulate ADH release from the posterior pituitary and aldosterone from the adrenal cortex
- Specialized renal cells produce erythropoietin
- Erythropoietin is necessary for red blood cell formation by the bone marrow
- Prostaglandin production provides protective and inflammatory functions
- Prostaglandins causes increased blood flow to the kidneys
Anatomical Location
- Kidneys are located in the dorsal abdomen in the retroperitoneal space
- Kidneys are outside the parietal peritoneum and tucked under the vertebrae
- Kidneys are surrounded by a thick layer of perirenal fat for protection
- In all domestic species except the pig, the right kidney is more cranial than the left
Right Kidney Position
- The right kidney is immediately caudal to the liver
- This results in a concave renal impression on the liver
Kidney Mobility
- The left caudal kidney is somewhat mobile
- Both kidneys move slightly caudal with each contraction of the diaphragm
- The left kidney's mobility makes it vulnerable to iatrogenic trauma
Gross Appearance
- Kidneys are "bean" shaped and brownish in color
- Cattle have nodular kidneys
- The kidney parenchyma is covered by a fibrous connective tissue capsule
- The hilus is the medial indentation where vessels and the ureter leave the kidney
Renal Pelvis
- The pelvis is a funnel-shaped area for urine collection, connecting the hilus and forming the ureter
- Cattle do not have this
- The renal cortex is the outer portion of the kidney, reddish-brown and granular
- The renal medulla is the inner portion surrounding the renal pelvis
- The medulla has a smooth appearance and dark purple exterior, sending rays into the cortex
- It features a pale, gray/red interior that extends into the renal pelvis
Medulla Structure
- Multilobular or multipyramidal structure of cattle and pigs have multiple pyramid shaped areas with the apex directed towards the pelvis or ureter
- Unilobar or unipyramidal structure of dogs, horses and cats have the medullary pyramids fused to occupy the entire inner area
- The calyx is a cuplike extension of the renal pelvis connecting to the medullary pyramids
Microscopic Anatomy
- Nephrons which are the functional units of the kidneys
- Thousands of nephrons are in each kidney
- Nephrons filter, reabsorb, and secrete
Nephron Components
- Each nephron consists of a renal corpuscle, proximal convoluted tubule, loop of Henle, and distal convoluted tubule
Renal Corpuscle
- The glomerulus and Bowman's capsule make up this structure
- The glomerulus is a tuft of capillaries for filtration with mostly fluid and without protein
- Bowman's capsule surrounds the glomerulus with an inner visceral and outer parietal layers
- The space between the layers is a capsular space continuous with the proximal convoluted tubule
- The renal corpuscle's function is to filter blood in the first stage of urine production
- Glomerular filtrate is the filtered fluid from the blood
Proximal Convoluted Tubule (PCT)
- The continuation of the capsular space
- The longest portion of the tubular part of the nephron
- It has cuboidal epithelium and a brush border to increase surface area
- This increased surface area is important for reabsorption and secretion
- As the glomerular filtrate travels through the PCT, it is called tubular filtrate
Loop of Henle
- It continues from the PCT descending into the renal medulla then returning to the cortex
- It is lined with cuboidal cells brush borders
- Thinner tube with lined simple squamous epithelial cells without a brush border
- Distal Convoluted Tubule (DCT): continuation of the ascending portion of the loop of Henle
- DCT twists through the renal cortex
Collecting Ducts
- Nephrons empty the DCT into these
- These collecting ducts carry tubular filtrate through the medulla to the renal pelvis
- These ducts affect urine volume and regulates potassium and acid-base
Renal Nerves
- Kidneys are primarily controlled by the sympathetic portion of the autonomic nervous system
- Nerves control blood flow to the glomerular capillaries
Blood Supply
- Kidneys receive a large blood supply, about 25% of the heart's output
- All circulating blood flows through the kidneys every 4–5 minutes
- Renal arteries branch off the abdominal aorta and enter the kidney at the hilus
- These arteries subdivide into afferent glomerular arterioles
Glomerular Arterioles
- Blood is carried to the glomerular capillaries of the renal corpuscle
- Glomerular capillaries filter plasma where some will deposit into Bowman's capsule, creating filtrate
Blood Filtrate
- Blood leaves the glomerulus via efferent glomerular arterioles still oxygenated
- The location where blood entering and leaving the capillaries is oxygenated
- The efferent glomerular arterioles divide into a network surrounding the nephron for oxygen transfer and reabsorption
- The glomerular filtrate will be reabsorbed into circulation
Vessels
- Peritubular capillaries surround the nephron
- These merge to form venules, which merge to form the renal vein, which exits the kidney at the hilus and enters the caudal vena cava.
- Filtration, reabsorption, and secretion are the mechanisms of renal action
- Filtration occurs in the renal corpuscle with capillaries between two arterioles under high pressure
- This pressure forces plasma into Bowman's capsule through fenestrations
Glomerular Filtrate
- It is similar to plasma but lacks proteins
- Plasma proteins are too large to escape unless there is damage to the endothelium of the glomerulus
- Protein in the urine indicates glomerular disease
Glomerular Filtration Rate
- GFR measures how fast plasma is filtered
- GFR depends on blood flow, which is affected by systemic blood pressure and disease
Reabsorption
- Once plasma is filtered and enters the capsular space, it is considered outside the body proper
- Glomerular filtrate contains both waste products and substances the body needs
- Includes sodium, potassium, calcium, magnesium, glucose, amino acids, chloride, bicarbonate, and water
- Reabsorption moves these substances from the glomerular filtrate back into the peritubular capillaries
Process
- Filtrate enters the PCT and becomes tubular filtrate
- Substances move out of the tubular lumen, through epithelial cells, into the interstitial fluid, and then peritubular capillaries
- Some passively; others actively use transport
- Sodium is actively pumped out of the tubular filtrate in the PCT back into the blood along with a carrier protein
- Glucose and amino acids use passive sodium cotransport
Additional Reabsorption
- Sodium ions are reabsorbed in the ascending loop of Henle and DCT in exchange for hydrogen, ammonium, or potassium
- The adrenal cortex controls this exchange via aldosterone
- Potassium moves out of the tubular filtrate in the PCT, the ascending loop of Henle, and the DCT by influence
- Calcium moves through tubular cells under influence of vitamin D, parathyroid hormone and calcitonin
- Magnesium is reabsorbed from the PCT, ascending loop of Henle, and collecting ducts
Sodium Balance
- When sodium is pumped into the interstitial space, it creates a negative charge
- Chloride ions then diffuse out of the tubular filtrate to maintain electrical neutrality
- Sodium, glucose, amino acids, and chloride leaves, water leaves the filtrate by osmosis
- The filtrate causes the concentrations of other substances to increase, therefore diffusing back into the blood
Urea
- Urea maintains a certain blood level
- 65% of tubular resorption occurs in the PCT, reabsorbing 80% of water, sodium, chloride, and bicarbonate, and 100% of glucose and amino acids
- Loop of Henle, DCT, and collecting ducts handles the rest of reabsorption
Secretion
- In this process, substances not adequately filtered in the blood,
- Substances move from the peritubular capillaries to the interstitial fluid, then to the tubular epithelial cells and tubular filtrate in the DCT
- Hydrogen, potassium, ammonia, and drugs like penicillins are eliminated
Urine Volume Regulation
- The presence of water in tubular filtrate determines it volume
- ADH regulates urine volume by acting on the DCT and collecting ducts to promote water reabsorption
- Volume will be lost without ADH (a state called polyuria)
- Aldosterone increases sodium reabsorption into the blood in the DCT and collecting duct to increase water back into the blood
- Water needs ADH to move out of these though
Tubular Movement
- Glomerular and tubular filtrate moves through the tubules and into the renal pelvis because of the pressure gradient
- Pressure in Bowman's capsule is high, and pressure in the renal pelvis is low
Ureters
- Ureters are the tubes that leave the renal pelvis and connect to the urinary bladder
- The tubes consist of three layers: the outer fibrous layer, the inner muscular layer, and an inner epithelial layer that is lined with transitional epithelium
- Transitional epithelium is used to allow that ureter to stretch when urine passes
- Ureters move urine continuously from the renal pelvis to the urinary bladder by peristaltic contractions
- Ureters enter the bladder at an angle
- The opening collapses when the bladder is full so that urine cannot back up into the ureter when the bladder is full
Urinary Bladder
- Periodically stores urine for release from the body
- Consists of a muscular sac and the neck
- It is lined with transitional epithelium that stretches as the bladder fills
- Bundles of smooth muscle contract and urine is expelled
- The neck of the bladder is attached to the urethra
- The neck is surrounded by sphincter muscles composed of skeletal muscle that enables urine control
Bladder State
- When the bladder is empty its walls are thick
- As it fills, it turns pear shaped and extends cranially into the abdominal cavity and stretches thin
Micturition Process
- Urination involves two to three steps and also known as micturition or uresis
- Urine accumulation occurs until stretch receptors activate in the bladder wall
- Muscle contraction occurs when the trigger is reached and a spinal reflex is activated that returns movement to the bladder muscles
- Sphincter muscle is voluntary to eliminate waste
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.