Podcast
Questions and Answers
What is the primary role of the urinary system?
What is the primary role of the urinary system?
- To ensure optimal properties of blood (correct)
- To facilitate digestion
- To filter nutrients from food
- To produce hormones
Which of the following hormones is secreted by the kidneys?
Which of the following hormones is secreted by the kidneys?
- Testosterone
- Cortisol
- Insulin
- Erythropoietin (correct)
What process do the kidneys use to maintain blood pH levels?
What process do the kidneys use to maintain blood pH levels?
- Excretion of glucose
- Filtration of proteins
- Reabsorption of bicarbonate (correct)
- Secretion of magnesium
What structure is formed at the upper end of the ureter?
What structure is formed at the upper end of the ureter?
What is the functional tissue of the kidney known as?
What is the functional tissue of the kidney known as?
During periods of fasting, what role do the kidneys play?
During periods of fasting, what role do the kidneys play?
What is the role of renin in the urinary system?
What is the role of renin in the urinary system?
What effect does the conversion of vitamin D in the kidneys have?
What effect does the conversion of vitamin D in the kidneys have?
Which component of the urinary system is primarily responsible for the excretion of metabolic wastes?
Which component of the urinary system is primarily responsible for the excretion of metabolic wastes?
What primarily surrounds the renal pelvis and calyces in the kidneys?
What primarily surrounds the renal pelvis and calyces in the kidneys?
What is the primary function of mesangial cells in the glomerulus?
What is the primary function of mesangial cells in the glomerulus?
Which statement correctly describes the structure of the proximal convoluted tubule?
Which statement correctly describes the structure of the proximal convoluted tubule?
What is the purpose of the slit diaphragms found in the nephron structure?
What is the purpose of the slit diaphragms found in the nephron structure?
How does the structure of ureters contribute to their function?
How does the structure of ureters contribute to their function?
What initiates the urge to urinate when the bladder reaches a certain volume?
What initiates the urge to urinate when the bladder reaches a certain volume?
What role do uroplakins play in the transitional epithelium of the bladder?
What role do uroplakins play in the transitional epithelium of the bladder?
What is the main function of the distal convoluted tubule?
What is the main function of the distal convoluted tubule?
What is the composition of the muscularis layer in the urinary bladder?
What is the composition of the muscularis layer in the urinary bladder?
Which feature distinguishes male urethra from female urethra?
Which feature distinguishes male urethra from female urethra?
What type of epithelium is found in the mucosa of the ureters?
What type of epithelium is found in the mucosa of the ureters?
What structures separate renal pyramids within the kidney?
What structures separate renal pyramids within the kidney?
Which part of the nephron is primarily involved in the reabsorption of water and nutrients?
Which part of the nephron is primarily involved in the reabsorption of water and nutrients?
What is the function of the afferent arteriole in the renal corpuscle?
What is the function of the afferent arteriole in the renal corpuscle?
What hormone regulates sodium reabsorption in the distal convoluted tubule?
What hormone regulates sodium reabsorption in the distal convoluted tubule?
Which structure collects urine formed by tubules in one renal lobe?
Which structure collects urine formed by tubules in one renal lobe?
What is the primary role of the vasa recta in the kidney?
What is the primary role of the vasa recta in the kidney?
Which layer of the glomerular capsule is responsible for filtration?
Which layer of the glomerular capsule is responsible for filtration?
What primarily occurs in the loop of Henle?
What primarily occurs in the loop of Henle?
How does the renal vein differ from the renal artery?
How does the renal vein differ from the renal artery?
What process primarily helps maintain the acid-base balance in the kidneys?
What process primarily helps maintain the acid-base balance in the kidneys?
Flashcards are hidden until you start studying
Study Notes
Overview of the Urinary System
- Comprises 2 kidneys, 2 ureters, bladder, and urethra.
- Key functions include blood property regulation, water and electrolyte balance, acid-base balance, and excretion of metabolic wastes.
Functions of the Urinary System
- Regulates fluid balance by adjusting water secretion.
- Maintains proper cell function by controlling inorganic ion levels (e.g., sodium).
- Supports pH balance by excreting hydrogen ions and reabsorbing bicarbonate.
- Filters metabolic wastes and excess electrolytes into urine via the ureters.
- Secretes renin (involved in blood pressure regulation) and erythropoietin (stimulates red blood cell production).
- Converts vitamin D to its active form, calcitriol, essential for calcium absorption.
- Engages in gluconeogenesis during starvation, aiding blood sugar maintenance.
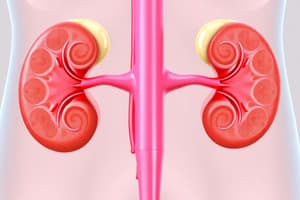
Anatomy of the Kidneys
- Each kidney contains a hilum for entry of nerves and exit of ureters.
- Surrounded by a fibrous layer; outer layer consists of fibroblasts, inner layer consists of myofibroblasts.
- Renal pelvis branches into major calyces, which further divide into minor calyces.
Kidney Structure
- Parenchyma (functional tissue) divided into renal cortex (outer, darker) and renal medulla (inner region with tubules).
- Renal cortex contains renal corpuscles and tubules along with intestinal cells.
- Renal medulla consists of renal pyramids (8-15) and renal columns between them.
Nephrons: The Functional Units
-
Each nephron consists of a renal corpuscle and a long renal tubule.
-
Renal Corpuscle:
- Glomerulus: Capillary tuft for initial blood filtration.
- Bowman's Capsule: Collects filtrate; contains visceral and parietal layers.
-
Renal Tubule:
- Proximal Convoluted Tubule: Major site for reabsorption of water, ions, glucose, and amino acids.
- Loop of Henle: Involved in the reabsorption of water (descending limb) and salts (ascending limb).
- Distal Convoluted Tubule: Regulates further reabsorption influenced by hormones like aldosterone.
- Collecting Duct: Concentrates urine, regulated by antidiuretic hormone (ADH).
Blood Flow in Kidneys
- Renal arteries supply oxygenated blood; renal veins return deoxygenated blood to the heart.
- Blood flow follows the pathway: renal artery → segmental arteries → interlobar arteries → arcuate arteries → interlobular arteries → afferent arterioles → glomerulus → efferent arterioles → peritubular capillaries → renal vein.
Renal Corpuscle Structure
- Contains glomerulus surrounded by glomerular capsule (visceral and parietal layers).
- Mesangial cells provide structural support, contract in response to blood pressure, and contribute to immune defense.
Proximal Convoluted Tubule Characteristics
- Specialized cells for reabsorption with a dense brush border, abundant mitochondria, and extensive membrane invaginations.
- Critical for maintaining body homeostasis.
Loop of Henle Morphology
- Thin descending and ascending limbs: simple squamous epithelium.
- Thick ascending limb: simple cuboidal epithelium with many mitochondria.
Distal Convoluted Tubule Role
- Lined by simple cuboidal cells; not as tall as proximal cells.
- Responsible for regulated reabsorption under hormonal control (aldosterone).
Ureters Structure and Function
- Muscular tubes transporting urine from kidneys to bladder.
- Composed of three layers: mucosa (transitional epithelium), muscularis (smooth muscle for peristalsis), and adventitia (connective tissue).
Urinary Bladder Composition
- Hollow organ with expandable walls: mucosa (transitional epithelium), muscularis (detrusor muscle), and adventitia/serosa.
- Stores 400-600 mL of urine; expels it during micturition.
Urethra Structure
- Male Urethra: 3-4 cm long through the prostate.
- Female Urethra: 3-5 cm, lined with transitional epithelium and then stratified squamous epithelium.
- Conducts urine from bladder; allows semen passage in males.
Urine Transport and Storage
- Ureters move urine via peristaltic contractions; bladder stores urine until fullness triggers urination.
- Detrusor muscle contracts to expel urine.
Cellular and Structural Adaptations
- Transitional epithelium: umbrella cells adapt surface area during bladder filling.
- Smooth muscle contractions facilitate urine movement; detrusor muscle essential for urination.
- Highly vascularized lamina propria and submucosa ensure organ function and health.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.