Podcast
Questions and Answers
What is the primary function of the urinary system?
What is the primary function of the urinary system?
- Carrying oxygen throughout the body
- Digesting food for energy
- Ridding the body of waste products (correct)
- Regulating body temperature
In what order does urine pass through the urinary system before being eliminated?
In what order does urine pass through the urinary system before being eliminated?
- Bladder, kidneys, ureters, urethra
- Urethra, bladder, kidneys, ureters
- Ureters, kidneys, bladder, urethra
- Kidneys, bladder, urethra, ureters (correct)
What role do nurses play in relation to urinary elimination issues?
What role do nurses play in relation to urinary elimination issues?
- Minimal role compared to other healthcare professionals
- Mainly an administrative role
- Important role in prevention and management (correct)
- No role at all
How can urinary elimination problems affect a patient?
How can urinary elimination problems affect a patient?
What is stored in the bladder before being eliminated via the urethra?
What is stored in the bladder before being eliminated via the urethra?
Why is it essential for nurses to assess the urinary system?
Why is it essential for nurses to assess the urinary system?
What is the primary purpose of the ureters in the urinary system?
What is the primary purpose of the ureters in the urinary system?
How does urinary elimination contribute to maintaining bodily health?
How does urinary elimination contribute to maintaining bodily health?
What are some common challenges that may impact urinary elimination in patients?
What are some common challenges that may impact urinary elimination in patients?
How do nurses contribute to the management of urinary elimination issues?
How do nurses contribute to the management of urinary elimination issues?
Why is it important for nurses to understand factors that affect urinary elimination?
Why is it important for nurses to understand factors that affect urinary elimination?
In what part of the body is urine stored before being eliminated via the urethra?
In what part of the body is urine stored before being eliminated via the urethra?
What is the primary function of the kidneys in the genitourinary tract?
What is the primary function of the kidneys in the genitourinary tract?
Which of the following is a symptom commonly associated with benign prostatic hyperplasia (BPH)?
Which of the following is a symptom commonly associated with benign prostatic hyperplasia (BPH)?
In the genitourinary tract, what is the main function of the ureters?
In the genitourinary tract, what is the main function of the ureters?
What is a common health issue that can arise due to bladder capacity concerns?
What is a common health issue that can arise due to bladder capacity concerns?
Which component of the genitourinary tract is responsible for storing urine before elimination via the urethra?
Which component of the genitourinary tract is responsible for storing urine before elimination via the urethra?
What role does the urethra play in the genitourinary tract?
What role does the urethra play in the genitourinary tract?
What complications can arise from a blockage or inflammation of the ureters?
What complications can arise from a blockage or inflammation of the ureters?
What is the primary symptom of bladder dysfunction?
What is the primary symptom of bladder dysfunction?
What is the role of urethra in maintaining proper fluid balance?
What is the role of urethra in maintaining proper fluid balance?
How does overactive bladder (OAB) affect individuals?
How does overactive bladder (OAB) affect individuals?
What serious conditions can result from infections due to disruptions in the urethral pathway?
What serious conditions can result from infections due to disruptions in the urethral pathway?
What happens if the ureters contract rhythmically but cannot propel urine smoothly?
What happens if the ureters contract rhythmically but cannot propel urine smoothly?
What effect can muscle atrophy related to menopausal hormonal changes have on urinary elimination?
What effect can muscle atrophy related to menopausal hormonal changes have on urinary elimination?
How does the use of diuretics impact urinary elimination?
How does the use of diuretics impact urinary elimination?
Which condition may interfere with voluntary control of urination due to cognitive deficits and psychiatric conditions?
Which condition may interfere with voluntary control of urination due to cognitive deficits and psychiatric conditions?
How does the abuse of analgesics impact the kidneys in terms of urinary elimination?
How does the abuse of analgesics impact the kidneys in terms of urinary elimination?
In what way does prolonged periods of immobility affect urinary control?
In what way does prolonged periods of immobility affect urinary control?
How can congenital urinary tract abnormalities impact urinary elimination?
How can congenital urinary tract abnormalities impact urinary elimination?
What may result from a diminished ability of the kidneys to concentrate urine?
What may result from a diminished ability of the kidneys to concentrate urine?
How does decreased bladder contractility affect urine elimination?
How does decreased bladder contractility affect urine elimination?
What effect does fluid overload have on urine excretion?
What effect does fluid overload have on urine excretion?
How do alcoholic beverages impact urine production?
How do alcoholic beverages impact urine production?
Which food and beverage consumption leads to decreased urine formation?
Which food and beverage consumption leads to decreased urine formation?
What is the correct order of techniques for abdominal assessment, starting from the first step?
What is the correct order of techniques for abdominal assessment, starting from the first step?
What visual characteristics should a nurse look for during abdomen inspection?
What visual characteristics should a nurse look for during abdomen inspection?
What might be indicated by abnormal findings like asymmetry or abdominal swelling during palpation?
What might be indicated by abnormal findings like asymmetry or abdominal swelling during palpation?
How should a nurse palpate the abdomen during examination?
How should a nurse palpate the abdomen during examination?
What should be noted when palpating each quadrant of the abdomen?
What should be noted when palpating each quadrant of the abdomen?
In what sequence should a nurse perform abdominal palpation if a patient complains of pain in a specific area?
In what sequence should a nurse perform abdominal palpation if a patient complains of pain in a specific area?
What is the primary difference between a regular bedpan and a fracture bedpan?
What is the primary difference between a regular bedpan and a fracture bedpan?
Why do male patients usually prefer using the urinal for voiding when confined to bed?
Why do male patients usually prefer using the urinal for voiding when confined to bed?
Why is it important to promote comfort and normalcy when assisting a patient with using a bedpan?
Why is it important to promote comfort and normalcy when assisting a patient with using a bedpan?
What guideline should be followed when positioning a regular bedpan under a patient's buttocks?
What guideline should be followed when positioning a regular bedpan under a patient's buttocks?
Which type of patients often use a fracture bedpan?
Which type of patients often use a fracture bedpan?
Why is it essential to provide skin care, perineal hygiene, and hand hygiene after a patient uses a bedpan?
Why is it essential to provide skin care, perineal hygiene, and hand hygiene after a patient uses a bedpan?
For which client would using powder on a bedpan be contraindicated?
For which client would using powder on a bedpan be contraindicated?
What discomfort might a client experience if powder is used on a bedpan?
What discomfort might a client experience if powder is used on a bedpan?
When is the use of powder on a bedpan generally considered acceptable?
When is the use of powder on a bedpan generally considered acceptable?
Why might using powder on a bedpan pose a potential problem for a client?
Why might using powder on a bedpan pose a potential problem for a client?
Which client situation would NOT pose a risk if powder is used on a bedpan?
Which client situation would NOT pose a risk if powder is used on a bedpan?
What is the most important concept for a nurse to remember when assisting a client with a bedpan post-abdominal surgery?
What is the most important concept for a nurse to remember when assisting a client with a bedpan post-abdominal surgery?
In the context of assisting a client with a bedpan post-abdominal surgery, what is the primary consideration regarding client privacy?
In the context of assisting a client with a bedpan post-abdominal surgery, what is the primary consideration regarding client privacy?
Why is it important for a nurse to prioritize client dignity over safety when assisting with a bedpan post-abdominal surgery?
Why is it important for a nurse to prioritize client dignity over safety when assisting with a bedpan post-abdominal surgery?
What aspect should a nurse focus on to enhance the client's experience when using a bedpan post-abdominal surgery?
What aspect should a nurse focus on to enhance the client's experience when using a bedpan post-abdominal surgery?
How can a nurse effectively demonstrate respect for a client's privacy and dignity when assisting them with a bedpan post-abdominal surgery?
How can a nurse effectively demonstrate respect for a client's privacy and dignity when assisting them with a bedpan post-abdominal surgery?
Why is client positioning important in nursing care?
Why is client positioning important in nursing care?
What is one of the main responsibilities of nurses in patient care?
What is one of the main responsibilities of nurses in patient care?
Why do nurses follow specific procedures for tasks in nursing care?
Why do nurses follow specific procedures for tasks in nursing care?
What is a crucial consideration when assisting a patient with bedpan removal?
What is a crucial consideration when assisting a patient with bedpan removal?
How can nurses best assist clients with various tasks in nursing care?
How can nurses best assist clients with various tasks in nursing care?
What is the significance of understanding clients' cultural and religious beliefs in nursing care?
What is the significance of understanding clients' cultural and religious beliefs in nursing care?
What is NOT a responsibility of a nurse when preparing clients for surgeries?
What is NOT a responsibility of a nurse when preparing clients for surgeries?
During bedpan removal, what should the nurse do before entering the room?
During bedpan removal, what should the nurse do before entering the room?
Which aspect is essential for nurses assisting clients post-surgery with bedpan use?
Which aspect is essential for nurses assisting clients post-surgery with bedpan use?
What is a key requirement for nurses when providing client assistance post-surgery?
What is a key requirement for nurses when providing client assistance post-surgery?
Which of the following is NOT part of client assistance provided by nurses?
Which of the following is NOT part of client assistance provided by nurses?
What is the most important intervention for a nurse to perform to prevent skin breakdown for clients using a bedpan?
What is the most important intervention for a nurse to perform to prevent skin breakdown for clients using a bedpan?
Which action is NOT recommended to prevent skin breakdown for clients using a bedpan?
Which action is NOT recommended to prevent skin breakdown for clients using a bedpan?
When assisting a client with bedpan removal, what should the nurse prioritize?
When assisting a client with bedpan removal, what should the nurse prioritize?
What is a critical responsibility of the nurse after a client uses a bedpan?
What is a critical responsibility of the nurse after a client uses a bedpan?
What is a key aspect for nurses to remember when assisting clients with bedpan use?
What is a key aspect for nurses to remember when assisting clients with bedpan use?
What is the primary assessment necessary for the nurse to complete after removing the bedpan from a frail older adult client?
What is the primary assessment necessary for the nurse to complete after removing the bedpan from a frail older adult client?
What is the nurse's primary responsibility when assisting a client with a bedpan post-abdominal surgery?
What is the nurse's primary responsibility when assisting a client with a bedpan post-abdominal surgery?
What should the nurse do before entering the room during bedpan removal?
What should the nurse do before entering the room during bedpan removal?
Why is it important for a nurse to assess the client's skin after they have used a bedpan?
Why is it important for a nurse to assess the client's skin after they have used a bedpan?
What is NOT a primary consideration for the nurse when providing assistance to a client with a bedpan?
What is NOT a primary consideration for the nurse when providing assistance to a client with a bedpan?
What is the primary reason for male patients confined to bed usually preferring to use the urinal for voiding?
What is the primary reason for male patients confined to bed usually preferring to use the urinal for voiding?
When assisting a patient with using a urinal, why should the bottom of the urinal be kept lower than the penis?
When assisting a patient with using a urinal, why should the bottom of the urinal be kept lower than the penis?
What should the nurse prioritize when assisting a patient who is unable to stand when using a urinal?
What should the nurse prioritize when assisting a patient who is unable to stand when using a urinal?
Why should a nurse not leave the urinal in place for extended periods when assisting a patient?
Why should a nurse not leave the urinal in place for extended periods when assisting a patient?
What is a crucial consideration for male patients using a urinal in bed?
What is a crucial consideration for male patients using a urinal in bed?
What should be done by the nurse if a patient is unable to stand while using a urinal?
What should be done by the nurse if a patient is unable to stand while using a urinal?
What is a crucial factor in ensuring patient safety during commode usage?
What is a crucial factor in ensuring patient safety during commode usage?
How can privacy be maintained for bedridden patients during commode usage?
How can privacy be maintained for bedridden patients during commode usage?
What is a key aspect of ensuring patient independence with commode usage?
What is a key aspect of ensuring patient independence with commode usage?
What can assistive toileting devices help healthcare professionals with?
What can assistive toileting devices help healthcare professionals with?
Why should healthcare providers consider mobility considerations when utilizing commodes?
Why should healthcare providers consider mobility considerations when utilizing commodes?
What is the significance of respecting the dignity of bedridden patients during commode usage?
What is the significance of respecting the dignity of bedridden patients during commode usage?
What is a critical factor that can significantly improve overall patient care when assisting patients with toileting?
What is a critical factor that can significantly improve overall patient care when assisting patients with toileting?
How does encouraging patients to participate in the toileting process benefit them?
How does encouraging patients to participate in the toileting process benefit them?
Why is designing commodes that cater to specific mobility requirements important?
Why is designing commodes that cater to specific mobility requirements important?
How does empowering patients to perform tasks independently benefit them?
How does empowering patients to perform tasks independently benefit them?
What role does regular training in communication skills play when assisting patients with toileting?
What role does regular training in communication skills play when assisting patients with toileting?
Why does encouraging patients to participate in their own personal care prepare them for discharge home?
Why does encouraging patients to participate in their own personal care prepare them for discharge home?
What is the primary reason for assessing a client for weakness, unsteady gait, and any functional limitations before assisting with a bedside commode?
What is the primary reason for assessing a client for weakness, unsteady gait, and any functional limitations before assisting with a bedside commode?
Why should the nurse offer a bedpan as an alternative option only under specific conditions?
Why should the nurse offer a bedpan as an alternative option only under specific conditions?
What could be a possible consequence of leaving drains and IV fluid lines unchecked before assisting a client with a bedside commode?
What could be a possible consequence of leaving drains and IV fluid lines unchecked before assisting a client with a bedside commode?
When assisting a client with limited mobility, why is proper footwear crucial?
When assisting a client with limited mobility, why is proper footwear crucial?
What should the nurse prioritize to enhance patient safety during assisted toileting?
What should the nurse prioritize to enhance patient safety during assisted toileting?
What is recommended as the guideline for catheterization based on postvoid residual (PVR) volume?
What is recommended as the guideline for catheterization based on postvoid residual (PVR) volume?
What position should the patient ideally be in during a bladder scan to ensure the most accurate results?
What position should the patient ideally be in during a bladder scan to ensure the most accurate results?
In what situation should a bladder scanner be utilized to assess bladder volume?
In what situation should a bladder scanner be utilized to assess bladder volume?
What setting on a bladder scanner should be ensured to be correct for accurate readings for a female patient after a hysterectomy?
What setting on a bladder scanner should be ensured to be correct for accurate readings for a female patient after a hysterectomy?
Why is it crucial to establish protocols to guide decision-making when considering catheterization for a patient?
Why is it crucial to establish protocols to guide decision-making when considering catheterization for a patient?
What should be the nursing priority when assisting a patient with limited mobility who needs to use a urinal?
What should be the nursing priority when assisting a patient with limited mobility who needs to use a urinal?
Why is establishing protocols important before deciding on catheterization for a patient?
Why is establishing protocols important before deciding on catheterization for a patient?
What effect does muscle atrophy due to menopausal hormonal changes have on urinary elimination?
What effect does muscle atrophy due to menopausal hormonal changes have on urinary elimination?
What should the nurse do if a patient with palpable bladder distention shows little urine in the bladder during a portable bladder ultrasound?
What should the nurse do if a patient with palpable bladder distention shows little urine in the bladder during a portable bladder ultrasound?
What is a recommended nursing action when assisting a patient with limited mobility who needs to use a urinal?
What is a recommended nursing action when assisting a patient with limited mobility who needs to use a urinal?
Why is encouraging patient independence with commode usage important in a healthcare setting?
Why is encouraging patient independence with commode usage important in a healthcare setting?
In what scenario would using powder on a bedpan pose a risk to the client?
In what scenario would using powder on a bedpan pose a risk to the client?
How does empowering patients to perform tasks independently benefit both the patients and healthcare providers?
How does empowering patients to perform tasks independently benefit both the patients and healthcare providers?
What should a nurse do if the external urinary sheath leaks with every voiding?
What should a nurse do if the external urinary sheath leaks with every voiding?
If a patient's external urinary sheath will not stay on, what is the appropriate action for the nurse to take?
If a patient's external urinary sheath will not stay on, what is the appropriate action for the nurse to take?
What should a nurse do if a patient with a retracted penis experiences issues with an external urinary sheath?
What should a nurse do if a patient with a retracted penis experiences issues with an external urinary sheath?
What should be avoided when there is a break in skin integrity found while assessing a patient's penis?
What should be avoided when there is a break in skin integrity found while assessing a patient's penis?
If a patient has a break in skin integrity while using an external urinary sheath, what should be arranged for by the healthcare provider?
If a patient has a break in skin integrity while using an external urinary sheath, what should be arranged for by the healthcare provider?
What is a recommended strategy to manage sudden leakages from condom catheters?
What is a recommended strategy to manage sudden leakages from condom catheters?
Why is regularly monitoring the catheter's performance essential?
Why is regularly monitoring the catheter's performance essential?
In what situation might occasional leakage from a condom catheter not require replacement?
In what situation might occasional leakage from a condom catheter not require replacement?
What factors might contribute to the decision to replace a condom catheter?
What factors might contribute to the decision to replace a condom catheter?
How does replacing a catheter help reduce the risk of complications?
How does replacing a catheter help reduce the risk of complications?
What is a crucial aspect to consider to prevent condom catheter leakage related to urinary catheter insertion?
What is a crucial aspect to consider to prevent condom catheter leakage related to urinary catheter insertion?
How do incontinence briefs, when used with a condom catheter, contribute to minimizing leakage?
How do incontinence briefs, when used with a condom catheter, contribute to minimizing leakage?
Which method of urination assistance can help reduce the risk of leaking in patients with a condom catheter?
Which method of urination assistance can help reduce the risk of leaking in patients with a condom catheter?
What impact can proper catheter replacement have on managing condom catheter leakage?
What impact can proper catheter replacement have on managing condom catheter leakage?
When assisting a patient with urination, which factor has the most significant effect on reducing condom catheter leakage?
When assisting a patient with urination, which factor has the most significant effect on reducing condom catheter leakage?
How does misalignment during urinary catheter insertion contribute to potential complications like leakage?
How does misalignment during urinary catheter insertion contribute to potential complications like leakage?
What should be done if there is not an immediate flow of urine after an intermittent catheter has been inserted?
What should be done if there is not an immediate flow of urine after an intermittent catheter has been inserted?
In what situation might selecting a catheter and balloon size separately be a requirement?
In what situation might selecting a catheter and balloon size separately be a requirement?
What can be done if urine flow does not occur within a minute of catheter insertion?
What can be done if urine flow does not occur within a minute of catheter insertion?
What is a possible reason for needing assistance from another staff member during catheterization?
What is a possible reason for needing assistance from another staff member during catheterization?
What should be done if a catheter cannot be advanced after insertion?
What should be done if a catheter cannot be advanced after insertion?
How can a nurse determine if there is a need for irrigating the catheter after insertion?
How can a nurse determine if there is a need for irrigating the catheter after insertion?
What is the primary reason behind the recommendation to avoid urinary catheterization whenever possible?
What is the primary reason behind the recommendation to avoid urinary catheterization whenever possible?
What type of catheter is designed to ensure it remains in the bladder by inflating a balloon?
What type of catheter is designed to ensure it remains in the bladder by inflating a balloon?
What is the recommended duration for which intermittent urethral catheters (straight catheters) are typically used to drain the bladder?
What is the recommended duration for which intermittent urethral catheters (straight catheters) are typically used to drain the bladder?
Why is intermittent catheterization considered an alternative to indwelling urethral catheterization?
Why is intermittent catheterization considered an alternative to indwelling urethral catheterization?
Which method of urinary catheter placement is primarily aimed at continuous drainage?
Which method of urinary catheter placement is primarily aimed at continuous drainage?
When replacing a urinary catheter, what should be inflated to ensure the new catheter remains in the bladder?
When replacing a urinary catheter, what should be inflated to ensure the new catheter remains in the bladder?
What is a key consideration regarding urinary catheter insertion?
What is a key consideration regarding urinary catheter insertion?
When managing intermittent catheter leakage, what is a common misconception to avoid?
When managing intermittent catheter leakage, what is a common misconception to avoid?
What is a critical aspect in ensuring proper incontinence brief placement with a condom catheter?
What is a critical aspect in ensuring proper incontinence brief placement with a condom catheter?
In urinary catheter management, what is a common error to avoid when replacing a condom catheter?
In urinary catheter management, what is a common error to avoid when replacing a condom catheter?
When assisting a patient with urination, what is a misconception to be cautious about?
When assisting a patient with urination, what is a misconception to be cautious about?
What is a crucial step in managing occasional leakage from a condom catheter?
What is a crucial step in managing occasional leakage from a condom catheter?
What is a crucial step before assisting a patient with intermittent urethral catheterization?
What is a crucial step before assisting a patient with intermittent urethral catheterization?
What is the recommended position for the patient during intermittent urethral catheterization?
What is the recommended position for the patient during intermittent urethral catheterization?
What should be done if there is a break in skin integrity while assessing a patient's penis during catheter insertion?
What should be done if there is a break in skin integrity while assessing a patient's penis during catheter insertion?
In managing intermittent catheter leakage, what is an important consideration to avoid?
In managing intermittent catheter leakage, what is an important consideration to avoid?
When replacing a urinary catheter, what should be inflated to ensure the new catheter remains in the bladder?
When replacing a urinary catheter, what should be inflated to ensure the new catheter remains in the bladder?
What is a common misconception to avoid when replacing a condom catheter?
What is a common misconception to avoid when replacing a condom catheter?
What should the nurse do if a patient experiences urinary catheter resistance through the urethra during insertion?
What should the nurse do if a patient experiences urinary catheter resistance through the urethra during insertion?
What is an important step in managing sudden leakages from condom catheters?
What is an important step in managing sudden leakages from condom catheters?
When replacing a urinary catheter, what should the nurse inflate to ensure the new catheter remains in the bladder?
When replacing a urinary catheter, what should the nurse inflate to ensure the new catheter remains in the bladder?
What is a common error to avoid when managing incontinence brief placement with a condom catheter?
What is a common error to avoid when managing incontinence brief placement with a condom catheter?
Why is intermittent catheterization considered an alternative to indwelling urethral catheterization?
Why is intermittent catheterization considered an alternative to indwelling urethral catheterization?
What should be done if a patient with a retracted penis experiences issues with an external urinary sheath?
What should be done if a patient with a retracted penis experiences issues with an external urinary sheath?
Why do male patients usually prefer using a urinal for voiding when confined to bed?
Why do male patients usually prefer using a urinal for voiding when confined to bed?
What is a recommended practice for managing occasional leakage from a condom catheter?
What is a recommended practice for managing occasional leakage from a condom catheter?
What should be avoided when dealing with a break in skin integrity found while assessing a patient's penis?
What should be avoided when dealing with a break in skin integrity found while assessing a patient's penis?
During urinary catheter insertion, what is essential to prevent potential complications like leakage?
During urinary catheter insertion, what is essential to prevent potential complications like leakage?
When replacing a urinary catheter, what should be inflated to ensure the new catheter remains in the bladder?
When replacing a urinary catheter, what should be inflated to ensure the new catheter remains in the bladder?
What is a common misconception to avoid when replacing a condom catheter?
What is a common misconception to avoid when replacing a condom catheter?
How can nurses best manage drainage bag leakage issues during urinary catheterization?
How can nurses best manage drainage bag leakage issues during urinary catheterization?
What is a potential complication that can arise during urinary catheter insertion?
What is a potential complication that can arise during urinary catheter insertion?
When replacing a condom catheter, what is a common error to avoid?
When replacing a condom catheter, what is a common error to avoid?
How can nurses best manage sudden leakages from condom catheters?
How can nurses best manage sudden leakages from condom catheters?
What is a crucial step in managing urinary drainage bag leakage issues during urinary catheterization?
What is a crucial step in managing urinary drainage bag leakage issues during urinary catheterization?
Why should a nurse assess the client's skin after using an incontinence brief?
Why should a nurse assess the client's skin after using an incontinence brief?
During a urinary catheter replacement, what should be ensured to prevent complications?
During a urinary catheter replacement, what should be ensured to prevent complications?
Why is it essential for healthcare providers to recognize the signs and symptoms of a urinary tract infection (UTI) in patients undergoing intermittent self-catheterization?
Why is it essential for healthcare providers to recognize the signs and symptoms of a urinary tract infection (UTI) in patients undergoing intermittent self-catheterization?
What common misconception should healthcare providers avoid when managing intermittent catheter leakage?
What common misconception should healthcare providers avoid when managing intermittent catheter leakage?
What is a crucial step in ensuring proper placement of incontinence briefs for patients using a condom catheter?
What is a crucial step in ensuring proper placement of incontinence briefs for patients using a condom catheter?
Why should healthcare providers prioritize patient privacy and dignity during urination assistance procedures?
Why should healthcare providers prioritize patient privacy and dignity during urination assistance procedures?
In what scenario might a nurse need to ensure proper inflation of a balloon while replacing a urinary catheter?
In what scenario might a nurse need to ensure proper inflation of a balloon while replacing a urinary catheter?
What is an important consideration when replacing a condom catheter to prevent potential errors?
What is an important consideration when replacing a condom catheter to prevent potential errors?
What should be done if sterile gloves come in contact with a nonsterile surface?
What should be done if sterile gloves come in contact with a nonsterile surface?
Why is it suggested to bring an extra pair of sterile gloves when gathering supplies?
Why is it suggested to bring an extra pair of sterile gloves when gathering supplies?
When should sterile gloves be replaced?
When should sterile gloves be replaced?
What guideline should be followed regarding the position of hands while wearing sterile gloves?
What guideline should be followed regarding the position of hands while wearing sterile gloves?
What action compromises the integrity of sterile gloves?
What action compromises the integrity of sterile gloves?
What should a nurse avoid touching to prevent contamination when removing gloves?
What should a nurse avoid touching to prevent contamination when removing gloves?
Why is it important for the nurse to keep the hands above the waistline when exposing the sterile gloves?
Why is it important for the nurse to keep the hands above the waistline when exposing the sterile gloves?
What is the purpose of sliding the fingers of one hand under the cuff of the glove and fully extending it down the arm?
What is the purpose of sliding the fingers of one hand under the cuff of the glove and fully extending it down the arm?
Why should a nurse grasp the opposite glove near the cuff end on the outside exposed area when removing soiled gloves?
Why should a nurse grasp the opposite glove near the cuff end on the outside exposed area when removing soiled gloves?
What is a crucial step to take to prevent contamination when adjusting both gloves on the hands?
What is a crucial step to take to prevent contamination when adjusting both gloves on the hands?
Why is it important for sterile surfaces to touch only other sterile surfaces when handling gloves?
Why is it important for sterile surfaces to touch only other sterile surfaces when handling gloves?
What is the appropriate action to take if a patient touches the nurse's hands or the sterile field?
What is the appropriate action to take if a patient touches the nurse's hands or the sterile field?
In the case of a patient with a latex allergy, what type of sterile gloves should the nurse obtain?
In the case of a patient with a latex allergy, what type of sterile gloves should the nurse obtain?
What is the recommended procedure if a hole or tear is noticed in one of the gloves during a medical procedure?
What is the recommended procedure if a hole or tear is noticed in one of the gloves during a medical procedure?
What should be done if contamination occurs during the application of sterile gloves?
What should be done if contamination occurs during the application of sterile gloves?
What is advised in terms of bringing sterile gloves into a room according to facility policy?
What is advised in terms of bringing sterile gloves into a room according to facility policy?
What action should be taken if a patient touches only the nurse's hands but nothing else?
What action should be taken if a patient touches only the nurse's hands but nothing else?
What is the nurse's key role in preventing the most common complication of urinary catheters?
What is the nurse's key role in preventing the most common complication of urinary catheters?
What is a crucial aspect of regular catheter care to prevent complications?
What is a crucial aspect of regular catheter care to prevent complications?
What should the nurse do if a client with an indwelling catheter shows signs of uncontrolled suprapubic pain?
What should the nurse do if a client with an indwelling catheter shows signs of uncontrolled suprapubic pain?
Why is it crucial for nurses to prioritize sterile technique during urinary catheter insertion?
Why is it crucial for nurses to prioritize sterile technique during urinary catheter insertion?
What should be the nurse's immediate action if a client with an indwelling catheter starts experiencing unsuppressed bladder spasms?
What should be the nurse's immediate action if a client with an indwelling catheter starts experiencing unsuppressed bladder spasms?
What should the nurse do if the catheter appears to be in the vaginal orifice during insertion?
What should the nurse do if the catheter appears to be in the vaginal orifice during insertion?
What is the rationale behind using a new catheter when a misplaced catheter is encountered?
What is the rationale behind using a new catheter when a misplaced catheter is encountered?
In urinary catheterization, what is the purpose of leaving a misplaced catheter in place as a marker?
In urinary catheterization, what is the purpose of leaving a misplaced catheter in place as a marker?
Why should a bladder ultrasound not be performed when the catheter is found in the vaginal orifice?
Why should a bladder ultrasound not be performed when the catheter is found in the vaginal orifice?
What is the benefit of using a misplaced catheter as a marker for subsequent insertion attempts?
What is the benefit of using a misplaced catheter as a marker for subsequent insertion attempts?
What should the nurse prioritize when assisting a client who has placed the catheter bag next to them in bed and reports bladder pain?
What should the nurse prioritize when assisting a client who has placed the catheter bag next to them in bed and reports bladder pain?
What is a key consideration for the nurse when managing a female client with an indwelling urinary catheter who has a distended bladder?
What is a key consideration for the nurse when managing a female client with an indwelling urinary catheter who has a distended bladder?
Why is it important for the nurse to place the catheter bag lower than the client when managing a client with an indwelling urinary catheter?
Why is it important for the nurse to place the catheter bag lower than the client when managing a client with an indwelling urinary catheter?
What is a potential complication of leaving the catheter bag at a level higher than the client's bladder when managing urinary drainage?
What is a potential complication of leaving the catheter bag at a level higher than the client's bladder when managing urinary drainage?
What could be a potential reason for a female client to experience bladder pain with a distended bladder while having an indwelling urinary catheter in place?
What could be a potential reason for a female client to experience bladder pain with a distended bladder while having an indwelling urinary catheter in place?
What should be the nurse's immediate action if a female client with an indwelling urinary catheter shows signs of catheter obstruction?
What should be the nurse's immediate action if a female client with an indwelling urinary catheter shows signs of catheter obstruction?
If a female patient with an indwelling urinary catheter experiences bladder spasms, what action should the nurse avoid?
If a female patient with an indwelling urinary catheter experiences bladder spasms, what action should the nurse avoid?
In the context of caring for a female client with an indwelling urinary catheter, what is a common misconception to be wary of regarding catheter care?
In the context of caring for a female client with an indwelling urinary catheter, what is a common misconception to be wary of regarding catheter care?
When assisting a female client with an indwelling urinary catheter, what is a crucial consideration for preventing complications?
When assisting a female client with an indwelling urinary catheter, what is a crucial consideration for preventing complications?
What precaution should be taken by the nurse when removing an indwelling urinary catheter from a female patient?
What precaution should be taken by the nurse when removing an indwelling urinary catheter from a female patient?
What should a healthcare provider avoid doing to prevent damage to the urethra when managing a catheter?
What should a healthcare provider avoid doing to prevent damage to the urethra when managing a catheter?
In catheter management, what could happen if the balloon is refilled with water?
In catheter management, what could happen if the balloon is refilled with water?
Why should a healthcare provider be cautious when determining the need to replace a catheter?
Why should a healthcare provider be cautious when determining the need to replace a catheter?
What should be checked first when assessing a catheter that is not draining properly?
What should be checked first when assessing a catheter that is not draining properly?
If kinks or twisting are not evident in a catheter, what might be the next course of action?
If kinks or twisting are not evident in a catheter, what might be the next course of action?
Where should a nurse hold an indwelling urinary catheter to allow for adequate control and decrease the risk of contamination?
Where should a nurse hold an indwelling urinary catheter to allow for adequate control and decrease the risk of contamination?
Why should a nurse avoid holding an indwelling urinary catheter directly at the tip during insertion?
Why should a nurse avoid holding an indwelling urinary catheter directly at the tip during insertion?
What could be a consequence of holding an indwelling urinary catheter too far from the tip during insertion?
What could be a consequence of holding an indwelling urinary catheter too far from the tip during insertion?
Why is it important for a nurse to hold an indwelling urinary catheter 2 to 3 in (5 to 7.5 cm) from the tip during insertion?
Why is it important for a nurse to hold an indwelling urinary catheter 2 to 3 in (5 to 7.5 cm) from the tip during insertion?
What action should the nurse take to ensure proper placement of an indwelling urinary catheter once urine drains into the tubing?
What action should the nurse take to ensure proper placement of an indwelling urinary catheter once urine drains into the tubing?
During urinary catheter insertion, what could happen if the catheter is stopped immediately once urine is noted in the tubing?
During urinary catheter insertion, what could happen if the catheter is stopped immediately once urine is noted in the tubing?
In urinary catheterization, why is rotating the catheter not recommended unless resistance is met?
In urinary catheterization, why is rotating the catheter not recommended unless resistance is met?
What is the rationale behind not retracting the catheter immediately after urine is noted in the tubing?
What is the rationale behind not retracting the catheter immediately after urine is noted in the tubing?
Why does advancing the urinary catheter an additional 2 to 3 inches after urine drainage help in catheterization?
Why does advancing the urinary catheter an additional 2 to 3 inches after urine drainage help in catheterization?
Flashcards are hidden until you start studying
Study Notes
Assisted Toileting: A Team Effort
- Assisting patients with toileting requires effective teamwork among healthcare providers.
- Regular training in correct lifting techniques, communication skills, understanding patient needs, and time management can improve overall patient care.
- Encouraging patients to participate in the process whenever possible fosters independence and self-confidence.
Patient Independence: Empowering Individuals Through Self-Care
- Empowering patients to perform tasks independently whenever possible has significant benefits.
- Teaching patients how to operate commodes and encouraging participation in their own personal care improves confidence, sense of control, and prepares them for discharge home.
Mobility Considerations: Enhancing Accessibility and Comfort
- Designing commodes that cater to specific mobility requirements enhances both comfort and accessibility for patients.
- Examples of adapted commodes include wheelchair-accessible commodes and larger seats for obese patients.
Commode Usage: Promoting Patient Safety and Dignity
- Commode usage plays a critical role in promoting patient safety, respecting privacy, and delivering comprehensive care.
- Commodes allow patients to maintain dignity and independence while providing healthcare professionals with essential information regarding bowel function and hygiene.
Patient Safety: Prioritizing Health and Wellbeing
- Ensuring the safety of patients during commode usage is paramount.
- Proper placement of cushions, maintaining appropriate water levels, and locking mechanisms can prevent injury or falls.
- Regular inspection and maintenance of commodes can help detect potential issues before they become hazardous.
Privacy Measures: Respecting the Bedridden Patient's Dignity
- Maintaining the dignity of bedridden patients is vital when using commodes.
- Facilities and guidelines should be designed to ensure privacy during commode usage.
- Factors such as providing curtains or doors for individual rooms and clear communication between staff members can create a more comfortable environment for patients.
Urinary Elimination: Factors Affecting Urine Production and Excretion
- Urinary elimination is affected by numerous factors, including:
- Kidney function
- Prostate enlargement
- Ureter involvement
- Bladder capacity
- Urethral concerns
- Aging
- Food and fluid intake
- Psychological variables
- Medications
- Pathologic conditions
- Activity and muscle tone
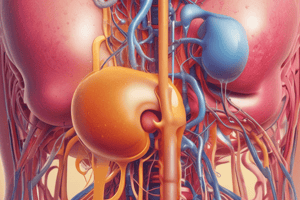
Genitourinary Tract: An Overview
- The genitourinary tract is a complex system responsible for eliminating waste from the body and maintaining its water balance.
- Components of the genitourinary tract include:
- Kidneys
- Prostate gland
- Ureters
- Bladder
- Urethra
Nursing Care: Client Positioning, Responsibilities, and Procedures
- Client positioning is crucial for preventing pressure ulcers, promoting proper lung expansion, and maintaining proper blood flow.
- Nurses are responsible for assessing clients' needs, providing medications, administering treatments, performing diagnostic tests, and educating clients about their health.
- Nursing procedures include:
- Preparing clients for surgeries
- Performing wound dressing changes
- Administering intravenous (IV) fluids
- Monitoring vital signs
- Giving medications as prescribed
- Removing a bedpan involves:
- Washing hands thoroughly
- Explaining the procedure to the client
- Using clean gloves and maintaining hand hygiene
- Client assistance includes:
- Assisting clients with bathing or using the toilet
- Providing emotional support during difficult times
- Helping with mobilization and exercise after surgery
Preventing Skin Breakdown
- The most important intervention to prevent skin breakdown for clients using a bedpan is to provide skin and perineal care after bedpan use.### Skin Assessment
- After using a bedpan, the nurse should assess the skin surrounding the buttocks and coccyx for irritation or skin breakdown due to pressure and friction.
Urinal Use
- Male patients confined to bed may prefer to use a urinal for voiding.
- To use a urinal, hold it close to the penis and position the penis completely within the urinal, with the bottom of the urinal lower than the penis.
- Slight spreading of the legs allows for proper positioning of the urinal.
- The urinal should not be left in place for extended periods to avoid pressure and irritation.
Abdominal Assessment
- Start with inspection, then auscultation, percussion, and palpation.
- Assess the abdomen for skin color, contour, pulsations, the umbilicus, and other surface characteristics.
- Normal findings include a centrally located umbilicus and evenly rounded or symmetric abdomen.
Perineal Care
- Clean the perineal area with a washcloth, skin cleanser, and warm water, using a different corner of the washcloth with each stroke.
- Wipe from above the orifice downward toward the sacrum (front to back).
Catheterization
- Use sterile technique and a fenestrated sterile drape.
- Lubricate 1 to 2 inches of the catheter tip.
- Hold the catheter 2 to 3 inches from the tip and insert slowly into the urethra.
- Advance the catheter until there is a return of urine (approximately 2 to 3 inches).
Intermittent Female Urethral Catheterization
- Check the medical record for the order for intermittent urethral catheterization.
- Review the patient's chart for any limitations in physical activity.
- Gather equipment and obtain assistance from another staff member if necessary.
Portable Bladder Ultrasound
- This is an accurate, reliable, and noninvasive device used to assess bladder volume.
- Results are most accurate when the patient is in the supine position during the scanning.
- A postvoid residual (PVR) volume less than 50 mL indicates adequate bladder emptying.
Care of the Patient with an Indwelling Catheter
- Use an indwelling catheter only when necessary and for the shortest duration possible.
- Use strict hand hygiene principles and sterile technique when inserting a catheter.
- Secure the catheter properly to the patient's thigh or abdomen after insertion.
- Keep the drainage bag below the level of the patient's bladder to maintain drainage of urine and prevent backflow.
Leakage Management
- Strategies are available to manage leakages from condom catheters, including immediate removal and reinsertion of the catheter.
- Regularly monitoring the catheter's performance is essential to detect changes early and promptly address them.### Urinary Catheterization
- Urinary catheterization is the introduction of a catheter through the urethra into the bladder to withdraw urine.
- Catheter-associated UTIs are the most common hospital-acquired infection in the US, and catheterization should be avoided whenever possible.
- When necessary, catheterization should be performed using strict aseptic technique and left in place for the shortest time possible.
Types of Catheters
- Indwelling urethral catheters (retention or Foley catheters) are used for continuous drainage and designed to not slip out of the bladder.
- Intermittent urethral catheters (straight catheters) are used for shorter periods (5-10 minutes) and are becoming the gold standard for bladder-emptying dysfunctions and post-surgical interventions.
- Intermittent catheterization has advantages, including lower risks of catheter-associated UTIs and complications.
Insertion of an Indwelling Catheter
- The procedure requires careful preparation, including facility policy and primary health care provider guidelines.
- The patient should be assessed for ability to lift buttocks and maintain position, and assistance may be necessary.
- Supplies should be opened and prepared on the overbed table, with the tray moved onto the bed just before cleansing the patient.
Potential Issues and Solutions
- If there is no immediate flow of urine after insertion, measures such as deep breathing, rotating the catheter, raising the head of the bed, and assessing intake and output can be helpful.
- If the catheter cannot be advanced, the patient should take deep breaths, and the catheter should be rotated and tried again; if still unable, the catheter should be removed and the primary care provider notified.
Patient Intermittent Self-Catheterization
- Patients should be educated on the reason for self-catheterization, potential complications, and how to incorporate it into daily routine.
- Patients should be instructed on anatomy, hygiene, and catheter preparation, with demonstration and return demonstration.
- Patients should be provided with information on recognizing UTIs and other signs/symptoms to report to the primary health care provider.
Sterile Gloves and Removing Soiled Gloves
- Sterile gloves should be applied and removed carefully to maintain asepsis, with hands kept above waist level and away from nonsterile surfaces.
- Soiled gloves should be replaced if they develop an opening or tear, come into contact with nonsterile surfaces, or are compromised in any way.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.