Podcast
Questions and Answers
How does the urinary system contribute to the regulation of blood pressure?
How does the urinary system contribute to the regulation of blood pressure?
- By secreting hormones that constrict blood vessels.
- By producing more red blood cells to increase blood volume.
- By increasing the heart rate to pump more blood.
- By controlling the volume of blood and the balance of sodium and water. (correct)
Which structure in the kidney is directly responsible for filtering blood to form urine?
Which structure in the kidney is directly responsible for filtering blood to form urine?
- Renal lobe
- Collecting duct
- Nephron (correct)
- Renal pelvis
What is the function of the renal fascia?
What is the function of the renal fascia?
- To attach the kidney to the abdominal wall. (correct)
- To facilitate urine drainage from the kidneys.
- To provide cushioning around the kidneys.
- To filter electrolytes from the blood.
Which of the following ions does the urinary system primarily regulate?
Which of the following ions does the urinary system primarily regulate?
What is one role of the kidneys in maintaining blood pH?
What is one role of the kidneys in maintaining blood pH?
Which of the following layers is responsible for giving shape to the kidney?
Which of the following layers is responsible for giving shape to the kidney?
Which part of the kidney is the inner region where nephron loops are located?
Which part of the kidney is the inner region where nephron loops are located?
What is the primary waste product excreted by the kidneys?
What is the primary waste product excreted by the kidneys?
In the kidney, which component directly connects to the ureters to transport urine?
In the kidney, which component directly connects to the ureters to transport urine?
What is the function of the urethra?
What is the function of the urethra?
What is the primary function of the glomerulus in the renal corpuscle?
What is the primary function of the glomerulus in the renal corpuscle?
Which layer of the ureter's mucosa is responsible for providing structural support?
Which layer of the ureter's mucosa is responsible for providing structural support?
What stimulates the juxtaglomerular apparatus to release nitric oxide?
What stimulates the juxtaglomerular apparatus to release nitric oxide?
What occurs during the micturition reflex when the bladder contains 200-400 mL of urine?
What occurs during the micturition reflex when the bladder contains 200-400 mL of urine?
What distinguishes cortical nephrons from juxtamedullary nephrons?
What distinguishes cortical nephrons from juxtamedullary nephrons?
How do renal veins drain blood from the kidneys?
How do renal veins drain blood from the kidneys?
What type of epithelium is found in the proximal convoluted tubule of the nephron?
What type of epithelium is found in the proximal convoluted tubule of the nephron?
Which condition results from a decrease in glomerular filtration?
Which condition results from a decrease in glomerular filtration?
What is the main anatomical challenge posed by an enlarged prostate in aging men?
What is the main anatomical challenge posed by an enlarged prostate in aging men?
What is the primary role of the mucosa in the digestive system?
What is the primary role of the mucosa in the digestive system?
Which layer is responsible for controlling the secretion rate of glands in the digestive system?
Which layer is responsible for controlling the secretion rate of glands in the digestive system?
What is the role of the muscularis layer in the digestive system?
What is the role of the muscularis layer in the digestive system?
Which muscle type is primarily found in the muscularis layer of the digestive tract?
Which muscle type is primarily found in the muscularis layer of the digestive tract?
What function does the serosa serve in the digestive system?
What function does the serosa serve in the digestive system?
What is the primary function of mesenteries in the abdominal cavity?
What is the primary function of mesenteries in the abdominal cavity?
What type of epithelial tissue is primarily found in the mucosa of the stomach and intestines for secretion?
What type of epithelial tissue is primarily found in the mucosa of the stomach and intestines for secretion?
Which of the following is considered the largest fold of peritoneum?
Which of the following is considered the largest fold of peritoneum?
Which specialized cells within the mucosa function to secrete hormones into the cardiovascular system?
Which specialized cells within the mucosa function to secrete hormones into the cardiovascular system?
What is the primary purpose of segmentation in the digestive tract?
What is the primary purpose of segmentation in the digestive tract?
Which structure connects the liver to the anterior abdominal wall?
Which structure connects the liver to the anterior abdominal wall?
What is the primary function of the peritoneum?
What is the primary function of the peritoneum?
What condition is characterized by inflammation of the peritoneum?
What condition is characterized by inflammation of the peritoneum?
Which of the following correctly describes the retroperitoneal space?
Which of the following correctly describes the retroperitoneal space?
Which part of the mesentery stabilizes the small intestines?
Which part of the mesentery stabilizes the small intestines?
What key vessels are contained within the lesser omentum?
What key vessels are contained within the lesser omentum?
Which fold of peritoneum holds the large intestine to the posterior abdominal wall?
Which fold of peritoneum holds the large intestine to the posterior abdominal wall?
Which of the following structures connects the stomach to the liver and duodenum?
Which of the following structures connects the stomach to the liver and duodenum?
What is primarily responsible for the body's immune response to substances entering through the digestive tract?
What is primarily responsible for the body's immune response to substances entering through the digestive tract?
Which organ can cause peritonitis if it ruptures and leaks feces?
Which organ can cause peritonitis if it ruptures and leaks feces?
Flashcards
What is the main function of the urinary system?
What is the main function of the urinary system?
The urinary system filters blood, removes excess water and solutes, stores urine, and allows us to urinate. It also plays a crucial role in regulating blood pressure, pH, glucose, and ion content.
How does the urinary system regulate blood pressure?
How does the urinary system regulate blood pressure?
The kidneys control the volume of blood and balance of sodium and water. When blood pressure is high, kidneys filter excess sodium and water, reducing blood volume and lowering pressure.
What role does the urinary system play in blood pH regulation?
What role does the urinary system play in blood pH regulation?
Kidneys selectively remove hydrogen ions and reabsorb bicarbonate ions from the blood, these ions are then excreted in urine, helping to maintain blood pH balance.
What are the organs of the urinary system?
What are the organs of the urinary system?
Signup and view all the flashcards
What is the function of the kidneys?
What is the function of the kidneys?
Signup and view all the flashcards
What is the renal capsule?
What is the renal capsule?
Signup and view all the flashcards
What is the difference between the cortex and the medulla in the kidney?
What is the difference between the cortex and the medulla in the kidney?
Signup and view all the flashcards
What is the nephron?
What is the nephron?
Signup and view all the flashcards
What is the flow of urine through the kidney?
What is the flow of urine through the kidney?
Signup and view all the flashcards
What are the calices?
What are the calices?
Signup and view all the flashcards
What are the two layers of the ureter's mucosa?
What are the two layers of the ureter's mucosa?
Signup and view all the flashcards
What is the function of the glomerulus?
What is the function of the glomerulus?
Signup and view all the flashcards
What are the two regions of a nephron?
What are the two regions of a nephron?
Signup and view all the flashcards
What is the juxtaglomerular apparatus?
What is the juxtaglomerular apparatus?
Signup and view all the flashcards
What is the function of the macula densa in the juxtaglomerular apparatus?
What is the function of the macula densa in the juxtaglomerular apparatus?
Signup and view all the flashcards
What is the function of the juxtaglomerular cells in the juxtaglomerular apparatus?
What is the function of the juxtaglomerular cells in the juxtaglomerular apparatus?
Signup and view all the flashcards
What are the three main functions of the nephron?
What are the three main functions of the nephron?
Signup and view all the flashcards
What is the detrusor muscle and where is it located?
What is the detrusor muscle and where is it located?
Signup and view all the flashcards
What is the micturition reflex?
What is the micturition reflex?
Signup and view all the flashcards
What is the innermost layer of the digestive system called?
What is the innermost layer of the digestive system called?
Signup and view all the flashcards
What are the layers of the digestive system?
What are the layers of the digestive system?
Signup and view all the flashcards
What are the functions of the mucosa?
What are the functions of the mucosa?
Signup and view all the flashcards
What is the submucosa?
What is the submucosa?
Signup and view all the flashcards
What is the muscularis layer?
What is the muscularis layer?
Signup and view all the flashcards
What is peristalsis?
What is peristalsis?
Signup and view all the flashcards
What is segmentation?
What is segmentation?
Signup and view all the flashcards
What is the serosa?
What is the serosa?
Signup and view all the flashcards
What is the peritoneum?
What is the peritoneum?
Signup and view all the flashcards
What is the function of the peritoneal cavity?
What is the function of the peritoneal cavity?
Signup and view all the flashcards
What are mesenteries?
What are mesenteries?
Signup and view all the flashcards
What is the role of the greater omentum?
What is the role of the greater omentum?
Signup and view all the flashcards
What is the falciform ligament?
What is the falciform ligament?
Signup and view all the flashcards
What is the lesser omentum's function?
What is the lesser omentum's function?
Signup and view all the flashcards
What is the function of the mesentery (proper)?
What is the function of the mesentery (proper)?
Signup and view all the flashcards
What is the mesocolon's function?
What is the mesocolon's function?
Signup and view all the flashcards
What is peritonitis?
What is peritonitis?
Signup and view all the flashcards
What are the main functions of the kidneys?
What are the main functions of the kidneys?
Signup and view all the flashcards
What is the function of the pancreas?
What is the function of the pancreas?
Signup and view all the flashcards
What are the parts of the large intestine?
What are the parts of the large intestine?
Signup and view all the flashcards
Study Notes
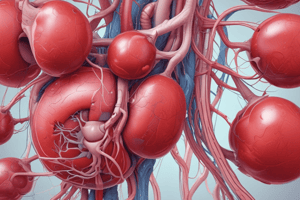
Urinary System Overview
- The urinary system significantly impacts the cardiovascular system by filtering blood, removing excess water and solutes, storing urine, and enabling voluntary urination.
- It regulates blood pressure by controlling blood volume and sodium/water balance. High blood pressure triggers the kidneys to filter excess sodium and water, reducing blood volume and lowering pressure.
- Blood pH regulation: The kidneys selectively remove hydrogen ions and reabsorb bicarbonate ions, which are then excreted in urine.
- Blood glucose regulation: Kidneys can lower or raise blood glucose levels through gluconeogenesis.
- Blood ion content regulation: Kidneys manage Na+, K+, Ca2+, and Cl- levels.
- Hormone production: Kidneys produce endocrine hormones.
- Waste excretion: The system excretes wastes (ammonia, urea, creatine) from the blood.
Kidney Anatomy & Physiology
- External Anatomy:
- Located retroperitoneally (behind the peritoneum).
- Reddish color due to extensive blood supply.
- Surrounded by layers:
- Renal capsule (fibrous): encloses the kidney.
- Adipose capsule (perinephric fat): provides padding.
- Renal fascia: anchors the kidney to abdominal walls.
- Internal Anatomy:
- Cortex: Outer layer, containing renal corpuscles, convoluted tubules, and proximal ends of collecting ducts.
- Medulla: Middle layer housing nephron loops and distal ends of collecting ducts, renal pyramids, renal columns, and/or renal lobe.
- Nephron - Functional Unit:
- Filters blood and forms urine.
- Urine flows through nephrons to collecting ducts then to calices, forming renal pelvis then flowing in to ureters.
- Each kidney contains approximately 1 million nephrons.
- Blood Supply:
- Kidneys receive about 25% of blood flow.
- Blood travels from abdominal aorta to renal arteries to segmental, interlobar, arcuate, and cortical radiate arteries..
- Afferent arterioles supply blood to glomeruli within nephrons.
- Efferent arterioles carry blood away from glomeruli, forming peritubular capillaries and vasa recta.
- Blood returns through veins: cortical radiate vein, arcuate vein, interlobar vein, renal vein, and eventually into the inferior vena cava.
- Lymphatic capillaries are also present.
- Nephron Regions:
- Renal corpuscle (glomerulus and glomerular capsule)
- Renal tubule
- Proximal convoluted tubule
- Nephron loop
- Distal convoluted tubule
- Juxtaglomerular apparatus (where afferent and efferent arterioles meet)
Kidney Histology
- Glomerular Capsule (Bowman's capsule):
- Double-layered simple squamous epithelium.
- Parietal layer (outer) and visceral layer (inner, which contacts glomerulus) of the capsule.
- Podocytes (visceral cells) aid in filtration.
- Collects filtered fluid (filtrate).
- Nephron Tubule:
- Proximal convoluted tubule: Simple cuboidal epithelium with microvilli.
- Nephron loop: Descending limb (simple squamous); Ascending limb (simple cuboidal, no microvilli).
- Distal convoluted tubule: Simple cuboidal epithelium, no microvilli.
- Collecting duct: Simple cuboidal, some with microvilli.
Juxtaglomerular Apparatus
- Consists of macula densa (specialized cells in nephron loop) and juxtaglomerular cells (specialized smooth muscle cells in arteriole).
- Macula densa senses filtration rate changes and releases nitric oxide (NO) to regulate blood flow.
- Juxtaglomerular cells detect blood pressure and release renin to regulate it.
Other Urinary Structures
- Ureters: Retroperitoneal tubes carrying urine from kidneys to bladder.
- Two layers of mucosa: transitional epithelium for stretching and lamina propria for support
- Approximately 11–18 calyces in humans.
- Bladder: Hollow organ situated anterior to rectum. - Contains transitional epithelium (mucosa), connective tissues (submucosa), and 3 layers of smooth muscle (muscularis, detrusor muscle).
- Urethra: Tube conveying urine from bladder to exterior.
- Men's urethra (8 inches) has three regions (prostatic, membranous, and spongy). Women's urethra (1.5 inches) has a simpler structure.
Micturition (Voiding Urine)
- Stretch receptors in the bladder trigger the micturition center in spinal cord when bladder is between 200-400 mL full
- The micturition reflex involves relaxation of internal urethral sphincter, contraction of detrusor muscle, and inhibition of external sphincter.
Aging and Renal Function
- Gradual decline in nephron function with age, leading to reduced filtration and urine formation.
- Loss of approximately 40% of nephrons by age 85.
- Potential prostate enlargement in men can affect urination.
Digestive System Layers
- Mucosa: Innermost layer, mucus membrane lining the lumen. Consists of mucosa-associated lymphoid tissue (MALT) for pathogen patrol. Contains mucosal, non-keratinized, stratified squamous epithelium for protection and simple columnar epithelium for secretion in parts of the digestive tract. Recovers every 7 days due to friction. Secretes mucus, hydrochloric acid, digestive enzymes, and hormones.
- Submucosa: Layer of areolar connective tissue containing blood vessels, lymph vessels, nerves, and Meissner's plexus (regulates gland secretions).
- Muscularis: Two layers of smooth muscle (circular and longitudinal) responsible for peristalsis (movement of materials). Can have a third layer in areas like the stomach. Includes skeletal muscle for voluntary control (mouth, pharynx, superior esophagus, and anal sphincter).
- Serosa: Outermost layer, serous membrane of simple squamous epithelium, secreting lubricating fluid and reducing organ friction in the abdominal cavity; replaced by adventitia in some regions like the pharynx, esophagus, and rectum for anchor.
Peritoneum and associated structures
- Peritoneum: Largest serous membrane composed of simple squamous epithelium and areolar connective tissue, providing support for organs, a pathway for blood vessels, and lymphatic vessels and immune response via lymph nodes . Parietal layer lines the abdominal cavity wall, visceral layer adheres to organs. Peritoneal cavity is the space between these layers, secreting and absorbing serous fluid.
- Retroperitoneal Space: Describes organs behind the peritoneum, including kidneys, pancreas, and parts of the large and small intestines.
- Mesenteries: Peritoneal folds that provide support, containing lymph nodes and blood vessels. Structures include:
- Greater omentum: Large fatty fold, significant lymph nodes.
- Falciform ligament: Attaches the liver to the anterior abdominal wall
- Lesser omentum: Connects the stomach, liver, and duodenum, and contains blood vessels.
- Mesentery (proper): Supports the jejunum and ileum.
- Mesocolon: Supports the transverse colon.
- Peritonitis: Inflammation/ infection of the peritoneum caused by organ rupture and leakage.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.