Podcast
Questions and Answers
Which ion is primarily reabsorbed through active transport in the renal tubule?
Which ion is primarily reabsorbed through active transport in the renal tubule?
- Chloride
- Potassium
- Calcium
- Sodium (correct)
What condition results from a build-up of uric acid in the blood?
What condition results from a build-up of uric acid in the blood?
- Kidney Stones
- Diabetes Insipidus
- Gout (correct)
- Cirrhosis
What part of the kidney is responsible for urine collection?
What part of the kidney is responsible for urine collection?
- Renal Pelvis (correct)
- Medulla
- Cortex
- Afferent Arterioles
How does aldosterone affect potassium in the kidney?
How does aldosterone affect potassium in the kidney?
In which vessel does blood flow last as it exits the kidney?
In which vessel does blood flow last as it exits the kidney?
Where does antidiuretic hormone (ADH) primarily promote water absorption?
Where does antidiuretic hormone (ADH) primarily promote water absorption?
What is the correct sequence of blood flow through the kidney starting from the renal artery?
What is the correct sequence of blood flow through the kidney starting from the renal artery?
Which part of the kidney contains the nephrons responsible for filtration?
Which part of the kidney contains the nephrons responsible for filtration?
What effect does increased arterial blood pressure have on glomerular hydrostatic pressure?
What effect does increased arterial blood pressure have on glomerular hydrostatic pressure?
How do the ureters connect to the urinary bladder to prevent backflow?
How do the ureters connect to the urinary bladder to prevent backflow?
In what order does the filtrate flow through the renal tubule?
In what order does the filtrate flow through the renal tubule?
What is the role of the juxtaglomerular apparatus in the regulation of blood pressure?
What is the role of the juxtaglomerular apparatus in the regulation of blood pressure?
What is the primary function of the countercurrent mechanism in the loop of Henle?
What is the primary function of the countercurrent mechanism in the loop of Henle?
How does glomerular filtrate differ from plasma?
How does glomerular filtrate differ from plasma?
Where does conscious control of micturition primarily inhibit the micturition reflex?
Where does conscious control of micturition primarily inhibit the micturition reflex?
What adaptation do the epithelial cells of the proximal tubule possess to enhance reabsorption?
What adaptation do the epithelial cells of the proximal tubule possess to enhance reabsorption?
What is the primary purpose of the glomerular capillaries?
What is the primary purpose of the glomerular capillaries?
How are hydrogen ions secreted in the kidneys?
How are hydrogen ions secreted in the kidneys?
What triggers the formation of water channels (aquaporins) in the collecting ducts?
What triggers the formation of water channels (aquaporins) in the collecting ducts?
What is the function of podocytes in the glomerulus?
What is the function of podocytes in the glomerulus?
How do electrolytes influence the movement of water across cell membranes?
How do electrolytes influence the movement of water across cell membranes?
Which factor inhibits the thirst center's activity?
Which factor inhibits the thirst center's activity?
What potential condition can result from prolonged dehydration?
What potential condition can result from prolonged dehydration?
What characterizes extracellular fluid in comparison to intracellular fluid?
What characterizes extracellular fluid in comparison to intracellular fluid?
How do protein buffers primarily function in maintaining pH?
How do protein buffers primarily function in maintaining pH?
Why are chemical buffers considered the first line of defense against pH shifts?
Why are chemical buffers considered the first line of defense against pH shifts?
What effect do ketone bodies have on blood pH?
What effect do ketone bodies have on blood pH?
What is the role of antidiuretic hormone (ADH) on water output in the kidneys?
What is the role of antidiuretic hormone (ADH) on water output in the kidneys?
What physiological response occurs after blood donation?
What physiological response occurs after blood donation?
What effect does activation of the renin-angiotensin system have on blood pressure?
What effect does activation of the renin-angiotensin system have on blood pressure?
How does gastric band placement affect thirst mechanisms?
How does gastric band placement affect thirst mechanisms?
What drives fluid exchange through capillary membranes?
What drives fluid exchange through capillary membranes?
What is the primary action of diuretics in the kidneys?
What is the primary action of diuretics in the kidneys?
Which of the following is a consequence of increased aldosterone release?
Which of the following is a consequence of increased aldosterone release?
What overall effect does the renin-angiotensin system have on electrolyte balance?
What overall effect does the renin-angiotensin system have on electrolyte balance?
Which processes are primarily involved in fluid movement at the capillary level?
Which processes are primarily involved in fluid movement at the capillary level?
What is the main effect of sodium reabsorption in the context of the renin-angiotensin system?
What is the main effect of sodium reabsorption in the context of the renin-angiotensin system?
What is one potential effect of fluid retention driven by aldosterone?
What is one potential effect of fluid retention driven by aldosterone?
How do diuretics influence blood pressure?
How do diuretics influence blood pressure?
Flashcards
Kidney function
Kidney function
Kidneys filter blood, produce urine, and regulate blood pressure and volume.
Nephron location
Nephron location
Nephrons are located in the cortex of the kidney.
Renal blood flow
Renal blood flow
Blood flows from the renal artery to the glomerulus, then to the peritubular capillaries and back to the renal vein.
ADH water absorption
ADH water absorption
Signup and view all the flashcards
Gout crystal formation
Gout crystal formation
Signup and view all the flashcards
Filtrate path
Filtrate path
Signup and view all the flashcards
Ureter & Bladder
Ureter & Bladder
Signup and view all the flashcards
Effect of blood pressure
Effect of blood pressure
Signup and view all the flashcards
Aldosterone's effect
Aldosterone's effect
Signup and view all the flashcards
Renal Clearance Definition
Renal Clearance Definition
Signup and view all the flashcards
Renal Tubule Sequence
Renal Tubule Sequence
Signup and view all the flashcards
Juxtaglomerular Apparatus's role
Juxtaglomerular Apparatus's role
Signup and view all the flashcards
Countercurrent Mechanism Function
Countercurrent Mechanism Function
Signup and view all the flashcards
Glomerular Filtrate vs. Plasma
Glomerular Filtrate vs. Plasma
Signup and view all the flashcards
Micturition Reflex Control
Micturition Reflex Control
Signup and view all the flashcards
Proximal Tubule Reabsorption
Proximal Tubule Reabsorption
Signup and view all the flashcards
Glomerular Capillary Purpose
Glomerular Capillary Purpose
Signup and view all the flashcards
Peritubular/Vasa Recta Capillary Purpose
Peritubular/Vasa Recta Capillary Purpose
Signup and view all the flashcards
Hydrogen Ion Secretion
Hydrogen Ion Secretion
Signup and view all the flashcards
Water Channel Formation
Water Channel Formation
Signup and view all the flashcards
Renin-Angiotensin System (RAS)
Renin-Angiotensin System (RAS)
Signup and view all the flashcards
Aldosterone's Role in RAS
Aldosterone's Role in RAS
Signup and view all the flashcards
How does RAS affect electrolyte balance?
How does RAS affect electrolyte balance?
Signup and view all the flashcards
Gastric Band Impact on Thirst
Gastric Band Impact on Thirst
Signup and view all the flashcards
Net Hydrostatic Forces
Net Hydrostatic Forces
Signup and view all the flashcards
Diuretic Function
Diuretic Function
Signup and view all the flashcards
How do diuretics work?
How do diuretics work?
Signup and view all the flashcards
What is the main function of the kidneys?
What is the main function of the kidneys?
Signup and view all the flashcards
What is the function of the glomerulus?
What is the function of the glomerulus?
Signup and view all the flashcards
What is the function of the nephron?
What is the function of the nephron?
Signup and view all the flashcards
Water & Electrolyte Interdependence
Water & Electrolyte Interdependence
Signup and view all the flashcards
Thirst Center Stimulation
Thirst Center Stimulation
Signup and view all the flashcards
How is thirst inhibited?
How is thirst inhibited?
Signup and view all the flashcards
Extracellular Fluid
Extracellular Fluid
Signup and view all the flashcards
Intracellular Fluid
Intracellular Fluid
Signup and view all the flashcards
Prolonged Vomiting Effects
Prolonged Vomiting Effects
Signup and view all the flashcards
What are buffer systems?
What are buffer systems?
Signup and view all the flashcards
Protein Buffer System
Protein Buffer System
Signup and view all the flashcards
Why are chemical buffers first line of defense?
Why are chemical buffers first line of defense?
Signup and view all the flashcards
Ketone Bodies Accumulation
Ketone Bodies Accumulation
Signup and view all the flashcards
Study Notes
Urinary System Organs and Function
- The urinary system consists of kidneys, ureters, bladder, and urethra.
- Gout is a condition where uric acid builds up in the blood, forming crystals in joints (often the big toe).
- High protein intake increases urea production, stressing kidneys and potentially causing dehydration or damage.
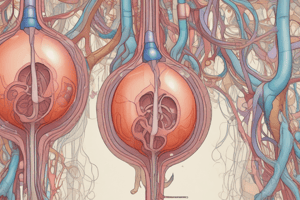
Kidney Structure and Function
- Cortex: Outer layer, containing nephrons for filtration.
- Medulla: Inner layer, containing renal pyramids for urine collection.
- Renal Pelvis: Central space collecting urine before ureter entry.
- ADH (Antidiuretic Hormone): Promotes water absorption in nephron collecting ducts.
- Secretion Ions in Renal Tubule: Sodium (actively), potassium, calcium, bicarbonate, and chloride (both active and passive).
- Renal Clearance: The rate kidneys remove a substance from the blood.
- Kidney Blood Vessel Pathway: Renal artery → segmental arteries → interlobar arteries → arcuate arteries → cortical radiate arteries → afferent arterioles → glomerulus → efferent arterioles → peritubular capillaries/vasa recta → cortical radiate veins → arcuate veins → interlobar veins → renal vein.
- Aldosterone Effect: Increases sodium reabsorption, potassium excretion, and water retention, controlling blood pressure and volume (produced by adrenal cortex).
- Filtrate Flow Through Renal Tubule: Glomerular capsule → proximal convoluted tubule → loop of Henle → distal convoluted tubule → collecting duct → renal pelvis.
Filtration, Reabsorption, and Secretion
- Glomerular Filtration: Glomerular filtrate is plasma minus large proteins and cells.
- Filtration Rate: Increased arterial blood pressure raises glomerular hydrostatic pressure and filtration rate; low pressure reduces it.
- Renal Tubule Secretion Sequence: Proximal convoluted tubule → Loop of Henle → distal convoluted tubule → collecting duct.
- Juxtaglomerular Apparatus (JGA): Regulates filtrate and blood pressure by releasing renin to activate the renin-angiotensin-aldosterone system (RAAS).
- Countercurrent Mechanism: Concentrates urine by establishing an osmotic gradient in the medulla through the loop of Henle.
Urine Formation and Excretion
-
Microvili in Proximal Tubule: Epithelial cells in the proximal tubules have microvilli increasing surface area for reabsorption.
-
Urinary Bladder Connection: Ureters enter the urinary bladder posteriorly in an oblique manner to prevent backflow.
-
Conscious Micturition Control: Conscious control inhibits urination reflex at the external urethral sphincter.
-
Hydrogen Ion Secretion: Hydrogen ions are secreted into distal convoluted tubules and collecting ducts for acid-base balance.
-
Capillary Bed Functions:
- Glomerular capillaries: Filtration.
- Peritubular capillaries/vasa recta: Reabsorption and secretion.
-
Podocytes and Pedicels: Podocytes comprise the filtration barrier in the glomerulus, with pedicels forming filtration slits which prevent large molecules from passing.
-
Aquaporins: Water channels stimulated by ADH in collecting ducts.
Blood Pathway Through the Kidney (Simplified)
- Renal artery → afferent arteriole → glomerulus → efferent arteriole → peritubular capillaries/vasa recta → renal vein.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.