Podcast
Questions and Answers
What is the normal Glomerular Filtration Rate (GFR) per day?
What is the normal Glomerular Filtration Rate (GFR) per day?
- 120 L/day
- 200 L/day
- 140 L/day
- 180 L/day (correct)
Which factor will directly increase the GFR?
Which factor will directly increase the GFR?
- Decreased blood volume
- Decreased glomerular capillary pressure
- Increased resistance in the efferent arteriole
- Increased glomerular capillary flow (correct)
What substance is normally totally reabsorbed in the kidneys?
What substance is normally totally reabsorbed in the kidneys?
- Urea
- Sodium
- Creatinine
- Glucose (correct)
What is the role of the juxtaglomerular apparatus in kidney function?
What is the role of the juxtaglomerular apparatus in kidney function?
Which condition can cause a decrease in GFR?
Which condition can cause a decrease in GFR?
What is the primary function of the macula densa cells?
What is the primary function of the macula densa cells?
What mechanism occurs when there is a severe drop in blood pressure?
What mechanism occurs when there is a severe drop in blood pressure?
Which compound is responsible for vasodilation and can affect GFR?
Which compound is responsible for vasodilation and can affect GFR?
What is the effect of increased sodium concentration in the distal convoluted tubule (DCT)?
What is the effect of increased sodium concentration in the distal convoluted tubule (DCT)?
What is the primary mechanism by which the body eliminates acid in cases of chronic acidosis?
What is the primary mechanism by which the body eliminates acid in cases of chronic acidosis?
How does an increase in extracellular fluid hydrogen ion concentration affect renal glutamine metabolism?
How does an increase in extracellular fluid hydrogen ion concentration affect renal glutamine metabolism?
What is the primary function of the ascending limb of the loop of Henle?
What is the primary function of the ascending limb of the loop of Henle?
Which of the following is TRUE about the descending limb of the loop of Henle?
Which of the following is TRUE about the descending limb of the loop of Henle?
Which of the following correctly describes the relationship between the descending limb and the ascending limb of the loop of Henle?
Which of the following correctly describes the relationship between the descending limb and the ascending limb of the loop of Henle?
What is the primary role of urea in the countercurrent multiplier system?
What is the primary role of urea in the countercurrent multiplier system?
What is the effect of the active transport of salts out of the ascending limb of the loop of Henle?
What is the effect of the active transport of salts out of the ascending limb of the loop of Henle?
Which of the following statements accurately describes the medullary ECF in the countercurrent multiplier system?
Which of the following statements accurately describes the medullary ECF in the countercurrent multiplier system?
What is the primary mechanism responsible for water reabsorption in the descending limb of the loop of Henle?
What is the primary mechanism responsible for water reabsorption in the descending limb of the loop of Henle?
Which of the following statements accurately describes the countercurrent multiplier system?
Which of the following statements accurately describes the countercurrent multiplier system?
What can an increased excretion of solute such as glucose indicate in urine analysis?
What can an increased excretion of solute such as glucose indicate in urine analysis?
What does a high urinary osmolality indicate?
What does a high urinary osmolality indicate?
What does the presence of more than 10 white blood cells per cm3 in urine commonly suggest?
What does the presence of more than 10 white blood cells per cm3 in urine commonly suggest?
What urinary appearance might suggest the presence of hemoglobinuria?
What urinary appearance might suggest the presence of hemoglobinuria?
Which renal function test would likely show elevated levels in the presence of poor renal function?
Which renal function test would likely show elevated levels in the presence of poor renal function?
What can the discoloration of urine due to beets indicate?
What can the discoloration of urine due to beets indicate?
In normal urine analysis, which of these findings would most likely indicate a renal issue?
In normal urine analysis, which of these findings would most likely indicate a renal issue?
What does hyperkalemia signify in the context of renal analysis?
What does hyperkalemia signify in the context of renal analysis?
What does a urinary pH test primarily help determine?
What does a urinary pH test primarily help determine?
What might be inferred from a sample showing both bacteria and white blood cells?
What might be inferred from a sample showing both bacteria and white blood cells?
Study Notes
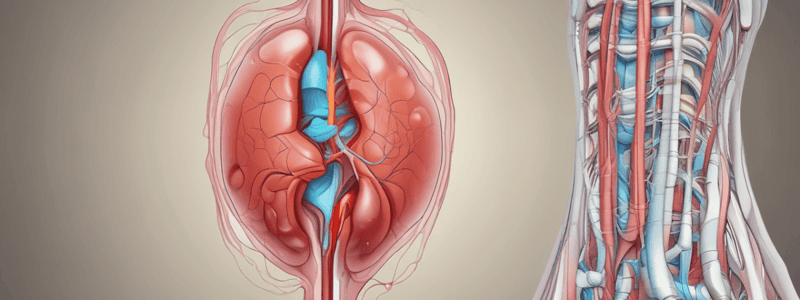
The Urinary System: Functional Significance
- The kidneys are retroperitoneal, located in the upper posterior abdominal wall at T11-T12.
- The right kidney is slightly lower than the left and shaped like a kidney bean, with a convex lateral surface and concave medial surface (hilum).
- Major functions include:
- Regulation of body fluid osmolarity, volume, electrolyte balance, acid-base balance, and blood pressure.
- Excretion of metabolic products, foreign substances (e.g., pesticides), and excess substances (e.g., water).
- Secretion of hormones such as erythropoietin, 1,25-dihydroxy vitamin D3, and renin.
Kidney Gross Anatomy
- The kidney consists of an outer cortex and an inner medulla.
- The hilum serves as the entry/exit point for major blood vessels, the ureter, lymphatics, and nerves.
Renal Blood Flow
- Blood flow through the renal system includes:
- Aorta > Renal Artery > Segmental Artery > Interlobar Artery > Arcuate Artery > Cortical Radiate Artery > Afferent Arteriole > Glomerulus > Efferent Arteriole > Peritubular Capillaries.
Microanatomy of the Nephron
- Two types of nephrons:
- Cortical Nephrons: Located in the outer cortex with short loops of Henle; rapid blood flow.
- Juxtamedullary Nephrons: Located in the inner cortex with long loops of Henle; maintain osmolality in hyperosmotic medulla.
- Collecting Ducts collect urine from distal convoluted tubules and open at the tip of the pyramid into the minor calyx.
Nephron Physiology Overview
- Key processes: filtration, reabsorption, secretion, and excretion.
- Filtration is the first step in urine formation, involving bulk transport of fluid from blood to kidney tubule.
- Glomerular Filtration Rate (GFR) is approximately 180 L/day.
- Reabsorption returns filtered materials to the bloodstream, with glucose typically being fully reabsorbed.
- Secretion adds materials from blood to kidney lumen, primarily via active transport.
Glomerular Filtration
- GFR is influenced by the dilation and constriction of afferent arterioles.
- Blood pressure in the glomerulus is much higher than typical capillary pressure, driving filtration.
- Filtration barrier consists of the squamous cell of the capillary and podocyte, providing protection against large molecules.
GFR Regulation
- Regulated by tubuloglomerular feedback involving sodium concentration detected by macula densa cells.
- A decrease in GFR and sodium concentration leads to renin release from juxtaglomerular cells.
Response to Blood Pressure Changes
- A severe drop in blood pressure triggers renin release, activating the renin-angiotensin system (RAS) to help restore GFR and blood flow.
- Renal function is modulated by factors such as sodium concentration, sympathetic nervous system activity, and hormones (e.g., angiotensin II, aldosterone).
Glomerular Filtration Rate Details
- GFR is the amount of filtrate produced in the kidneys each minute, averaging 125 mL/min.
- Control of glomerular capillary flow is crucial; increases in flow lead to increased GFR, while decreases lead to lowered GFR.
Pinocytosis and Urinary System Function
- Pinocytosis is not the main transport method but aids in reabsorbing larger proteins between cells.
- Mechanisms of reabsorption and secretion in the urinary system utilize similar processes.
Primary and Secondary Active Transport Mechanisms
- Sodium ion (Na+) transport involves primary active transport via antiport mechanisms across the basal membrane.
- The sodium-potassium ATPase generates the force required for sodium, chloride, water, glucose, and amino acid reabsorption.
- Secondary active transport occurs through symport mechanisms, aiding the movement of glucose and amino acids when coupled with Na+.
Proximal Convoluted Tubule (PCT) Reabsorption
- The proximal tubule is crucial for reabsorbing H2O, Na+, Cl-, glucose, and amino acids.
- In early PCT, sodium reabsorbs alongside glucose and amino acids; later portions prioritize sodium-chloride reabsorption.
- Almost all glucose is reabsorbed, with minimal glucose appearing in urine; the renal threshold for glucose is around 375 mg/min (men) and 300 mg/min (women).
Bicarbonate Reabsorption
- Bicarbonate is reclaimed for blood through specific transport mechanisms in the tubules.
- Secreted hydrogen ions combine with bicarbonate in tubule fluid, producing carbonaceous compounds.
Hydrogen Ion Secretion
- The kidneys play a vital role in excreting non-volatile acids and reabsorbing HCO3- to maintain acid-base balance.
- Hydrogen ions are secreted primarily through secondary active transport in proximal tubules, loop of Henle, and distal tubules.
- The proton pump facilitates primary active transport of hydrogen ions at the tubular cell's luminal membrane, crucial for producing acidic urine.
Generation of New Bicarbonate
- Glutamine metabolism in proximal tubules generates ammonium and bicarbonate ions, contributing to new bicarbonate formation.
- Ammonia acts as a buffer, combining with excess hydrogen ions to maintain pH.
Countercurrent Multiplier in the Loop of Henle
- The Loop of Henle has distinct ascending and descending limbs with differing permeabilities.
- The descending limb is permeable to water but not salts; the ascending limb actively transports salts out while being impermeable to water.
- This transport creates a hypertonic medullary environment, enhancing water reabsorption in the collecting tubule.
Key Biochemical Players in Urinary Physiology
-
ADH/AVP (Antidiuretic Hormone/Vasopressin)
- Released due to hypothalamic stimulation from dehydration or elevated Angiotensin II (AgII) levels.
- Increases water retention by inserting more aquaporins in tubule cell membranes.
- Responsible for concentrating urine.
-
ANP (Atrial Natriuretic Peptide)
- Secreted by the atrium in response to stretching from increased blood volume.
- Promotes sodium and water loss by enhancing glomerular flow and inhibiting ADH secretion.
- Triggers natriuresis (sodium excretion) and diuresis (water excretion).
-
Aldosterone
- Released in reaction to increased levels of Angiotensin II.
- Promotes reabsorption of sodium and secretion of potassium in the kidneys.
- Enhances sodium permeability by stimulating the Na+-K+ ATPase pump.
-
Angiotensin II
- Stimulates the release of aldosterone and ADH.
- Causes vasoconstriction, increasing systemic blood pressure while decreasing glomerular filtration rate (GFR).
-
Renin
- An enzyme that converts Angiotensinogen to Angiotensin I.
- Secretion is regulated through renal (macula densa), nervous (sympathetic nerve stimulation), and hormonal mechanisms (epinephrine, prostaglandins).
Nervous System Influence on Renal Function
- Renal plexus of the autonomic nervous system influences kidney function by regulating smooth muscle in afferent arterioles.
- Effects of Sympathetic Nerve Activity:
- Decreases GFR via vasoconstriction of afferent arterioles.
- Increases sodium reabsorption in proximal tubules.
- Enhances renin release.
Nephron Operation Overview
- Key nephron interactions impact blood pressure and renal functioning, involving hormones such as ADH and aldosterone and responses to renal blood flow and composition.
Urination/Micturition Process
- Urination involves both autonomic and somatic control through various nervous systems, maintaining bladder tone and controlling sphincters.
- Bladder filling triggers sensory nerves, leading to a coordinated response for urination:
- Parasympathetic signals cause bladder contraction, while sympathetic inhibits urination maintaining sphincter tone until appropriate.
Urinalysis Overview
-
Definitions:
- Oliguria: Less than 300 ml/day; may suggest physiological feedback or renal disease.
- Polyuria: Increased urine output; often linked to conditions like hyperglycemia.
- Osmolality and Urinary pH: Useful for assessing urine concentration and diagnosing acid/base imbalances.
-
Appearance Assessment:
- Hematuria detected via dipstick tests; concentrated urine may be dark, while dilute can appear clear.
- Discoloration can arise from various causes (jaundice, medications, foods).
-
Microscopy Analysis:
- Clean mid-stream samples needed; presence of 10+ white blood cells indicates inflammation, suggestive of urinary tract infections (UTIs).
- Red blood cells and casts imply potential diseases or injuries.
Renal Function Blood Testing
- Indicators of poor renal function include:
- Hyperkalemia, Decreased bicarbonate, Elevated BUN (Blood Urea Nitrogen), Elevated creatinine, Elevated uric acid, Hypocalcemia, Hyperphosphatemia.
- Changes in pH and pCO2 may indicate acid/base disorders.
- Assessment of these parameters helps evaluate renal health and function effectively.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Explore the gross anatomy and microanatomy of the nephron and learn about the major functions of the kidneys, including regulation of bodily functions.