Podcast
Questions and Answers
What is the primary epithelium type found in the mucosa of the oesophagus?
What is the primary epithelium type found in the mucosa of the oesophagus?
- Cuboidal epithelium
- Ciliated epithelium
- Squamous epithelium (correct)
- Columnar epithelium
Which type of oesophageal diverticulum involves all four layers of the wall?
Which type of oesophageal diverticulum involves all four layers of the wall?
- Pulsion diverticulum
- False diverticulum
- Functional diverticulum
- True diverticulum (correct)
Which condition is characterized by 'failure to relax' of the oesophageal sphincter?
Which condition is characterized by 'failure to relax' of the oesophageal sphincter?
- Scleroderma
- Achalasia (correct)
- Reflux esophagitis
- Diverticulitis
What anatomical abnormality is associated with trachea-oesophageal fistula?
What anatomical abnormality is associated with trachea-oesophageal fistula?
What consequence results from an increased resting tone of the lower oesophageal sphincter?
What consequence results from an increased resting tone of the lower oesophageal sphincter?
Which type of hiatus hernia is the most common, representing 95% of cases?
Which type of hiatus hernia is the most common, representing 95% of cases?
Which of the following is NOT considered a major category causing dysphagia?
Which of the following is NOT considered a major category causing dysphagia?
Which condition is NOT a primary cause of achalasia?
Which condition is NOT a primary cause of achalasia?
What causes pulsion diverticula?
What causes pulsion diverticula?
What is the most common cause of oesophageal perforation?
What is the most common cause of oesophageal perforation?
Which factor contributes to the development of oesophageal varices?
Which factor contributes to the development of oesophageal varices?
What is the key histological feature of Barrett's oesophagus?
What is the key histological feature of Barrett's oesophagus?
What is the composition of a 'false' diverticulum?
What is the composition of a 'false' diverticulum?
What histological changes are characteristic of reflux oesophagitis?
What histological changes are characteristic of reflux oesophagitis?
What are potential causes of oesophagitis?
What are potential causes of oesophagitis?
What type of metaplasia is referred to as Barrett's oesophagus?
What type of metaplasia is referred to as Barrett's oesophagus?
Which infectious agent is commonly associated with secondary achalasia?
Which infectious agent is commonly associated with secondary achalasia?
What characteristic finding might suggest the presence of a Mallory-Weiss tear?
What characteristic finding might suggest the presence of a Mallory-Weiss tear?
What is a common complication of oesophageal perforation?
What is a common complication of oesophageal perforation?
Which of the following factors could lead to reflux oesophagitis?
Which of the following factors could lead to reflux oesophagitis?
What is the term used to describe the change from squamous mucosa to glandular mucosa in the oesophagus due to chronic acid exposure?
What is the term used to describe the change from squamous mucosa to glandular mucosa in the oesophagus due to chronic acid exposure?
What characterizes long-segment Barrett's oesophagus?
What characterizes long-segment Barrett's oesophagus?
Which condition results from chronic acid exposure leading to a change in oesophageal mucosa?
Which condition results from chronic acid exposure leading to a change in oesophageal mucosa?
Which of the following is NOT a benign or malignant tumor of the oropharynx, oesophagus, or stomach?
Which of the following is NOT a benign or malignant tumor of the oropharynx, oesophagus, or stomach?
What is a common cause of salivary gland enlargement?
What is a common cause of salivary gland enlargement?
What is the annual risk percentage of developing adenocarcinoma from Barrett's oesophagus?
What is the annual risk percentage of developing adenocarcinoma from Barrett's oesophagus?
Which histological type accounts for 70% of oesophageal cancers?
Which histological type accounts for 70% of oesophageal cancers?
Which location is most commonly affected by squamous cell carcinoma of the oesophagus?
Which location is most commonly affected by squamous cell carcinoma of the oesophagus?
What is a common lifestyle risk factor for the development of squamous cell carcinoma of the oesophagus?
What is a common lifestyle risk factor for the development of squamous cell carcinoma of the oesophagus?
What percentage of oesophageal malignancies does adenocarcinoma represent?
What percentage of oesophageal malignancies does adenocarcinoma represent?
What type of treatment is frequently employed for oesophageal cancer?
What type of treatment is frequently employed for oesophageal cancer?
Which of the following is NOT a benign tumor of the oesophagus?
Which of the following is NOT a benign tumor of the oesophagus?
What is a common symptom associated with both squamous cell carcinoma and adenocarcinoma of the oesophagus?
What is a common symptom associated with both squamous cell carcinoma and adenocarcinoma of the oesophagus?
Which of the following is NOT a known cause of acute gastritis?
Which of the following is NOT a known cause of acute gastritis?
What histological feature is commonly observed in acute gastritis?
What histological feature is commonly observed in acute gastritis?
Which of the following is a characteristic feature of erythroplakia?
Which of the following is a characteristic feature of erythroplakia?
Which type of gastritis is characterized by the presence of mucosal atrophy and epithelial metaplasia?
Which type of gastritis is characterized by the presence of mucosal atrophy and epithelial metaplasia?
The presence of which bacteria is primarily associated with Helicobacter-associated gastritis?
The presence of which bacteria is primarily associated with Helicobacter-associated gastritis?
What type of salivary gland tumor is most common in the parotid gland?
What type of salivary gland tumor is most common in the parotid gland?
Which of the following statements about chronic gastritis is correct?
Which of the following statements about chronic gastritis is correct?
Which of the following factors is associated with Warthin’s tumor?
Which of the following factors is associated with Warthin’s tumor?
What is the primary characteristic indicating malignant salivary gland tumors?
What is the primary characteristic indicating malignant salivary gland tumors?
What is one potential complication of untreated chronic gastritis?
What is one potential complication of untreated chronic gastritis?
Which condition is NOT associated with Helicobacter pylori infection?
Which condition is NOT associated with Helicobacter pylori infection?
Which condition is characterized by inflammation of the salivary glands?
Which condition is characterized by inflammation of the salivary glands?
What histological change is characterized by the infiltration of lymphocytes and plasma cells?
What histological change is characterized by the infiltration of lymphocytes and plasma cells?
Which of the following substances is known to be corrosive and can contribute to acute gastritis?
Which of the following substances is known to be corrosive and can contribute to acute gastritis?
Which of the following is a common symptom of both acute and chronic gastritis?
Which of the following is a common symptom of both acute and chronic gastritis?
What factor is associated with a higher risk of developing gastric carcinoma?
What factor is associated with a higher risk of developing gastric carcinoma?
Which histological type of gastric cancer is known for being more infiltrative and having a worse prognosis?
Which histological type of gastric cancer is known for being more infiltrative and having a worse prognosis?
What is the 5-year survival rate for localized gastric cancer?
What is the 5-year survival rate for localized gastric cancer?
Which method is primarily used to treat Gastrointestinal Stromal Tumours (GIST)?
Which method is primarily used to treat Gastrointestinal Stromal Tumours (GIST)?
Which condition is characterized by a white plaque in the mouth that cannot be removed by scraping?
Which condition is characterized by a white plaque in the mouth that cannot be removed by scraping?
What is the cure rate for submucosal involvement in early gastric cancer?
What is the cure rate for submucosal involvement in early gastric cancer?
What is a common clinical feature of GISTs in adults?
What is a common clinical feature of GISTs in adults?
What is a common diagnostic method for Helicobacter-Associated Gastritis?
What is a common diagnostic method for Helicobacter-Associated Gastritis?
Which of the following is NOT typically associated with benign tumors of the mouth?
Which of the following is NOT typically associated with benign tumors of the mouth?
Which prognostic factor is important in determining the outcome for gastric cancer?
Which prognostic factor is important in determining the outcome for gastric cancer?
Which condition is characterized by autoantibodies against parietal cells?
Which condition is characterized by autoantibodies against parietal cells?
What is the main cause of malignant tumors in the mouth linked to squamous cell carcinoma?
What is the main cause of malignant tumors in the mouth linked to squamous cell carcinoma?
What histological change is observed in intestinal metaplasia?
What histological change is observed in intestinal metaplasia?
Which type of gastritis is most commonly associated with prior gastric surgery?
Which type of gastritis is most commonly associated with prior gastric surgery?
What is the risk associated with autoimmune chronic gastritis?
What is the risk associated with autoimmune chronic gastritis?
Which of the following is NOT a typical site for peptic ulcers?
Which of the following is NOT a typical site for peptic ulcers?
What is a consequence of decreased intrinsic factor production in autoimmune chronic gastritis?
What is a consequence of decreased intrinsic factor production in autoimmune chronic gastritis?
Which feature is typically seen microscopically in chemical / reflux gastritis?
Which feature is typically seen microscopically in chemical / reflux gastritis?
What is a defining feature of peptic ulcers?
What is a defining feature of peptic ulcers?
What is the term for the condition where gastric epithelium undergoes metaplasia to resemble small intestine?
What is the term for the condition where gastric epithelium undergoes metaplasia to resemble small intestine?
What is the primary factor that influences the prognosis of gastric carcinoma?
What is the primary factor that influences the prognosis of gastric carcinoma?
Which type of gastric carcinoma is characterized by diffuse growth and a worse prognosis?
Which type of gastric carcinoma is characterized by diffuse growth and a worse prognosis?
Which factor is associated with a significantly improved cure rate in early gastric cancer?
Which factor is associated with a significantly improved cure rate in early gastric cancer?
What is a common mutation associated with Gastrointestinal Stromal Tumours (GIST)?
What is a common mutation associated with Gastrointestinal Stromal Tumours (GIST)?
Which symptom is least likely associated with gastrointestinal stromal tumors (GIST) in adults?
Which symptom is least likely associated with gastrointestinal stromal tumors (GIST) in adults?
Which of the following is a primary cause of acute gastritis?
Which of the following is a primary cause of acute gastritis?
What histological feature is characteristic of chronic gastritis?
What histological feature is characteristic of chronic gastritis?
Which type of gastritis is commonly associated with autoimmune processes?
Which type of gastritis is commonly associated with autoimmune processes?
Which clinical presentation is most consistent with acute gastritis?
Which clinical presentation is most consistent with acute gastritis?
What is a common histological finding associated with Helicobacter-associated gastritis?
What is a common histological finding associated with Helicobacter-associated gastritis?
Which of the following factors is least likely to cause acute gastritis?
Which of the following factors is least likely to cause acute gastritis?
Which feature differentiates chronic gastritis from acute gastritis?
Which feature differentiates chronic gastritis from acute gastritis?
What complication is associated with untreated chronic gastritis?
What complication is associated with untreated chronic gastritis?
Which statement about Helicobacter pylori is accurate?
Which statement about Helicobacter pylori is accurate?
Which factor is correlated with the development of gastric carcinoma?
Which factor is correlated with the development of gastric carcinoma?
What is the estimated annual risk percentage for the development of adenocarcinoma in patients with Barrett's oesophagus?
What is the estimated annual risk percentage for the development of adenocarcinoma in patients with Barrett's oesophagus?
Which histological subtype is most prevalent among oesophageal cancers?
Which histological subtype is most prevalent among oesophageal cancers?
Which condition is primarily associated with the development of adenocarcinoma of the oesophagus?
Which condition is primarily associated with the development of adenocarcinoma of the oesophagus?
What is a common clinical feature associated with both types of oesophageal cancer?
What is a common clinical feature associated with both types of oesophageal cancer?
What factor significantly increases the risk of developing squamous cell carcinoma of the oesophagus?
What factor significantly increases the risk of developing squamous cell carcinoma of the oesophagus?
Which of the following statements about oesophageal cancer prognosis is accurate?
Which of the following statements about oesophageal cancer prognosis is accurate?
What is a major feature for the presence of Barrett's oesophagus identified during an endoscopy?
What is a major feature for the presence of Barrett's oesophagus identified during an endoscopy?
What type of oesophageal cancer is primarily characterized by ulcerating gross appearance?
What type of oesophageal cancer is primarily characterized by ulcerating gross appearance?
What is a common clinical presentation of gastric ulcers?
What is a common clinical presentation of gastric ulcers?
Which of the following statements accurately describes autoimmune chronic gastritis?
Which of the following statements accurately describes autoimmune chronic gastritis?
What microscopical feature is most indicative of reflux gastritis?
What microscopical feature is most indicative of reflux gastritis?
In the microscopic appearance of peptic ulcers, which zone is NOT typically identified?
In the microscopic appearance of peptic ulcers, which zone is NOT typically identified?
In terms of gastric cancer risk, which condition is closely linked to intestinal metaplasia?
In terms of gastric cancer risk, which condition is closely linked to intestinal metaplasia?
Which complication of peptic ulcers can result in life-threatening scenarios?
Which complication of peptic ulcers can result in life-threatening scenarios?
Which diagnosis can be definitively established through a biopsy?
Which diagnosis can be definitively established through a biopsy?
What is a characteristic feature of stress ulcers?
What is a characteristic feature of stress ulcers?
What underlying condition must be considered when treating a patient with autoimmune chronic gastritis?
What underlying condition must be considered when treating a patient with autoimmune chronic gastritis?
Which symptom is often associated with duodenal ulcers?
Which symptom is often associated with duodenal ulcers?
Which site is least commonly involved in peptic ulcer disease?
Which site is least commonly involved in peptic ulcer disease?
What is NOT a characteristic of the gross appearance of peptic ulcers?
What is NOT a characteristic of the gross appearance of peptic ulcers?
What is the primary etiological factor in peptic ulcer disease?
What is the primary etiological factor in peptic ulcer disease?
What is a potential outcome of prolonged peptic ulcer disease?
What is a potential outcome of prolonged peptic ulcer disease?
Which condition is characterized by metaplasia of gastric epithelium to small intestinal epithelium?
Which condition is characterized by metaplasia of gastric epithelium to small intestinal epithelium?
Which of the following is true regarding the vascular changes in the scarred area of peptic ulcers?
Which of the following is true regarding the vascular changes in the scarred area of peptic ulcers?
Which of the following statements about the urea breath test is correct?
Which of the following statements about the urea breath test is correct?
Which treatment option is generally not indicated for peptic ulcer disease?
Which treatment option is generally not indicated for peptic ulcer disease?
What is a distinguishing characteristic of complications arising from peptic ulcers?
What is a distinguishing characteristic of complications arising from peptic ulcers?
Which condition may show a histological feature of vascular ectasia?
Which condition may show a histological feature of vascular ectasia?
Which type of benign tumor is the most common in the parotid gland?
Which type of benign tumor is the most common in the parotid gland?
Which characteristic is indicative of malignant transformation in pleomorphic adenoma?
Which characteristic is indicative of malignant transformation in pleomorphic adenoma?
What is the percentage of Warthin's tumors that can be classified as multifocal?
What is the percentage of Warthin's tumors that can be classified as multifocal?
What histological feature is observed in adenoid cystic carcinoma?
What histological feature is observed in adenoid cystic carcinoma?
Which of the following statements about pleomorphic adenoma is correct?
Which of the following statements about pleomorphic adenoma is correct?
Which of the following is a typical characteristic of malignant salivary gland tumors?
Which of the following is a typical characteristic of malignant salivary gland tumors?
A hiatus hernia can be classified into two types: [blank] and sliding (95%):
A hiatus hernia can be classified into two types: [blank] and sliding (95%):
Commonly due to instrumentation or severe vomiting , the esophagus is a condition characterized by a tear in the mucosa of the esophagus. This condition is known as a [blank].
Commonly due to instrumentation or severe vomiting , the esophagus is a condition characterized by a tear in the mucosa of the esophagus. This condition is known as a [blank].
Dilated veins due to portal hypertension, prevalent in cirrhotic patients, are known as [blank].
Dilated veins due to portal hypertension, prevalent in cirrhotic patients, are known as [blank].
Causes of Achalasia
Primary: Neural imbalance, degenerative conditions, diabetes.
Secondary:
Infectious ________.
Infiltrative (tumors, amyloidosis, sarcoidosis)
Causes of Achalasia
Primary: Neural imbalance, degenerative conditions, diabetes.
Secondary:
Infectious ________.
Infiltrative (tumors, amyloidosis, sarcoidosis)
One of the common fungal infections of the upper GI tract is [blank].
One of the common fungal infections of the upper GI tract is [blank].
In inflammatory disorders, examples of viral infections include [blank] and [blank].
In inflammatory disorders, examples of viral infections include [blank] and [blank].
Inflammatory disorders can be caused by organisms such as fungal (Candida albicans), viral (Herpes, CMV), and by [blank] exposure or caustic substances.
Inflammatory disorders can be caused by organisms such as fungal (Candida albicans), viral (Herpes, CMV), and by [blank] exposure or caustic substances.
Which of the following are contributing factors to reflux? (Select all that apply)
Which of the following are contributing factors to reflux? (Select all that apply)
Which of the following histological features are characteristic of Reflux Esophagitis? (Select all that apply)
Which of the following histological features are characteristic of Reflux Esophagitis? (Select all that apply)
Which statements about the Esophagogastric Junction are correct? (Select all that apply)
Which statements about the Esophagogastric Junction are correct? (Select all that apply)
Which of the following statements is true regarding Barrett's esophagus?
Which of the following statements is true regarding Barrett's esophagus?
Which condition may develop dysplasia, leading to a risk of adenocarcinoma at approximately 0.5% per year?
Which condition may develop dysplasia, leading to a risk of adenocarcinoma at approximately 0.5% per year?
Which of the following are benign tumours found in the oesophagus? (Select all that apply)
Which of the following are benign tumours found in the oesophagus? (Select all that apply)
Oesophageal tumours include benign types such as leiomyomas, lipomas, and fibromas.
Oesophageal tumours include benign types such as leiomyomas, lipomas, and fibromas.
Malignant primary tumors predominantly are epithelial, with which of the following distributions?
Malignant primary tumors predominantly are epithelial, with which of the following distributions?
Which of the following gross appearances is associated with oesophageal tumours? (Select all that apply)
Which of the following gross appearances is associated with oesophageal tumours? (Select all that apply)
What are common risk factors for squamous cell carcinoma (SCC) of the esophagus? (Select all that apply)
What are common risk factors for squamous cell carcinoma (SCC) of the esophagus? (Select all that apply)
Which of the following statements about squamous cell carcinoma (SCC) of the esophagus is true? (Select all that apply)
Which of the following statements about squamous cell carcinoma (SCC) of the esophagus is true? (Select all that apply)
Which of the following are risk factors for squamous cell carcinoma (SCC) of the esophagus? (Select all that apply)
Which of the following are risk factors for squamous cell carcinoma (SCC) of the esophagus? (Select all that apply)
Which changes are associated with chronic gastritis? (Select all that apply)
Which changes are associated with chronic gastritis? (Select all that apply)
Chronic gastritis histology reveals lymphocyte and plasma cell infiltration. Which type of chronic gastritis is associated with this histological finding?
Chronic gastritis histology reveals lymphocyte and plasma cell infiltration. Which type of chronic gastritis is associated with this histological finding?
What is a characteristic feature of acute gastritis?
What is a characteristic feature of acute gastritis?
Which of the following statements about H. pylori is correct?
Which of the following statements about H. pylori is correct?
Which of the following statements about H. pylori is true?
Which of the following statements about H. pylori is true?
Which of the following statements about urease is true?
Which of the following statements about urease is true?
What characterizes Diffuse Antral Gastritis (DAG) in the stomach's antral region?
What characterizes Diffuse Antral Gastritis (DAG) in the stomach's antral region?
Diffuse Antral Gastritis (DAG) is primarily caused by which of the following?
Diffuse Antral Gastritis (DAG) is primarily caused by which of the following?
What is true about Multifocal Atrophic Gastritis (MAG)?
What is true about Multifocal Atrophic Gastritis (MAG)?
H. pylori bacteria are found in the superficial mucous layers of the stomach lining. Which diagnostic technique can be used to detect the bacteria?
H. pylori bacteria are found in the superficial mucous layers of the stomach lining. Which diagnostic technique can be used to detect the bacteria?
Which of the following complications is associated with Autoimmune Chronic Gastritis?
Which of the following complications is associated with Autoimmune Chronic Gastritis?
What condition is typically associated with Autoimmune Chronic Gastritis and is characterized by the presence of autoantibodies against parietal cells?
What condition is typically associated with Autoimmune Chronic Gastritis and is characterized by the presence of autoantibodies against parietal cells?
There is a decrease in gastric acid production due to the loss of parietal cells, which condition does this describe?
There is a decrease in gastric acid production due to the loss of parietal cells, which condition does this describe?
Autoimmune chronic gastritis is often seen in conjunction with other autoimmune diseases, including which of the following? (Select all that apply)
Autoimmune chronic gastritis is often seen in conjunction with other autoimmune diseases, including which of the following? (Select all that apply)
In patients with chemical reflux gastritis, microscopy reveals which of the following features?
In patients with chemical reflux gastritis, microscopy reveals which of the following features?
Intestinal metaplasia associated with chronic gastritis refers to which of the following transformations?
Intestinal metaplasia associated with chronic gastritis refers to which of the following transformations?
Which condition is characterized by gastrin-secreting tumors (gastrinomas) that cause excessive gastric acid production, leading to multiple peptic ulcers?
Which condition is characterized by gastrin-secreting tumors (gastrinomas) that cause excessive gastric acid production, leading to multiple peptic ulcers?
Which of the following descriptions accurately describes peptic ulcers?
Which of the following descriptions accurately describes peptic ulcers?
What are the characteristic features of an ulcer under miacroscob described in the provided details?
What are the characteristic features of an ulcer under miacroscob described in the provided details?
Three distinct zones of ulcer under microscopy are [blank].
Three distinct zones of ulcer under microscopy are [blank].
Under microscopy, ulcers can be categorized into three distinct zones which help in understanding the healing process and pathology. Vessels within the scarred area are ..........
Under microscopy, ulcers can be categorized into three distinct zones which help in understanding the healing process and pathology. Vessels within the scarred area are ..........
Acute Gastric Ulcers ("Stress Ulcers"): Microscopy: ............... The ulcers typically occur under conditions of severe stress.
Acute Gastric Ulcers ("Stress Ulcers"): Microscopy: ............... The ulcers typically occur under conditions of severe stress.
Acute gastric ulcers are also known as 'Stress Ulcers' and can lead to [blank] and may heal without scarring within days to several weeks.
Acute gastric ulcers are also known as 'Stress Ulcers' and can lead to [blank] and may heal without scarring within days to several weeks.
GIST tumors are often associated with .......; treated with tyrosine kinase inhibitors like Gleevec™.
GIST tumors are often associated with .......; treated with tyrosine kinase inhibitors like Gleevec™.
Clinical features of GIST include: [blank]
Clinical features of GIST include: [blank]
Gastrointestinal stromal tumors (GISTs) commonly present with abdominal pain and may cause melaena, while obstruction is a rare occurrence. Which of the following statements is true regarding GISTs?
Gastrointestinal stromal tumors (GISTs) commonly present with abdominal pain and may cause melaena, while obstruction is a rare occurrence. Which of the following statements is true regarding GISTs?
A patient presents with abdominal pain without obstruction and is an adult. What is the likely diagnosis?
A patient presents with abdominal pain without obstruction and is an adult. What is the likely diagnosis?
What is the most common site for gastric carcinoma and its prevalence? 50-60%
What is the most common site for gastric carcinoma and its prevalence? 50-60%
What is the least common site for gastric carcinoma and its prevalence?
What is the least common site for gastric carcinoma and its prevalence?
Benign tumors include squamous papillomas linked to which of the following HPV types?
Benign tumors include squamous papillomas linked to which of the following HPV types?
Malignant tumors of the upper gastrointestinal tract are primarily classified as squamous cell carcinoma (>95%). Which of the following factors are linked to these types of malignancies?
Malignant tumors of the upper gastrointestinal tract are primarily classified as squamous cell carcinoma (>95%). Which of the following factors are linked to these types of malignancies?
Glossitis: Deficiencies in B12 and iron are associated with which condition?
Glossitis: Deficiencies in B12 and iron are associated with which condition?
Which of the following infections is associated with hairy leukoplakia in HIV patients?
Which of the following infections is associated with hairy leukoplakia in HIV patients?
Leukoplakia: A white plaque or patch on mucous membranes, often considered.....
Leukoplakia: A white plaque or patch on mucous membranes, often considered.....
Red, velvety patch with a high risk of malignancy; common in smokers and males. What is this condition called?
Red, velvety patch with a high risk of malignancy; common in smokers and males. What is this condition called?
Salivary Glands secrete proteins and fluid, categorized as mucinous or mixed. Ducts are lined by what type of epithelium?
Salivary Glands secrete proteins and fluid, categorized as mucinous or mixed. Ducts are lined by what type of epithelium?
Flashcards are hidden until you start studying
Study Notes
Learning Outcomes
- Understand normal anatomy of the mouth, esophagus, and stomach.
- Recognize benign and malignant tumors of the oropharynx, esophagus, and stomach.
- Identify common conditions affecting the mouth and causes of salivary gland enlargement.
- Diagnose causes of esophagitis and gastritis.
- Define Barrett's esophagus.
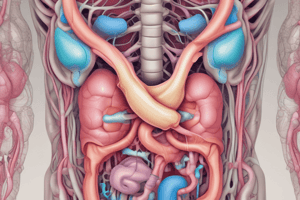
Esophagus Anatomy
- Mucosa: Comprises squamous epithelium and lamina propria (loose connective tissue).
- Submucosa: Contains connective tissue, blood vessels, and nerves.
- Muscle Layer: Enables peristalsis.
- Adventitia: Connective tissue covering the esophagus.
Symptoms of Esophageal Disorders
- Dysphagia (difficulty swallowing) caused by:
- Lesions in the lumen (e.g., foreign body, tumors)
- Lesions in the wall (e.g., tumors, strictures)
- Lesions outside the wall (e.g., tumors, aortic aneurysms)
- Functional lesions (e.g., achalasia)
Anatomic Disorders of Esophagus
- Developmental Abnormalities:
- Atresia/Fistula: Often linked to pulmonary issues.
- Acquired Abnormalities:
- Diverticula:
- True (involves all layers) vs. False (involves only mucosa/submucosa).
- Pulsion: Pressure-induced; Traction: Local pathology-related.
- Webs/Rings:
- Webs: Thin mucosal folds (2-3mm).
- Rings: Bands involving mucosa and submucosa.
- Diverticula:
Hiatus Hernia
- Affects 1-20% of adults.
- Separation of diaphragmatic crura into:
- Sliding (95%): Movement of stomach through diaphragm.
- Paraesophageal: Non-axial positioning.
- Common Complications
- Reflux: Particularly with sliding hernias, GERD is common due to the weakening of the LES.
- Ulceration: Both types of hernias can result in ulcers within the herniated portion of the stomach due to the continuous acid exposure or mechanical irritation.
Esophageal Motor Disorders
- Achalasia:
- Characterized by failure to relax with three key abnormalities:
- Aperistalsis (lack of peristalsis)
- Incomplete relaxation of lower esophageal sphincter during swallowing
- Increased resting tone of lower esophageal sphincter
- Characterized by failure to relax with three key abnormalities:
Causes of Achalasia
- Primary: Neural imbalance, degenerative conditions, diabetes.
- Secondary:
- Infectious (Trypanosoma, Polio)
- Infiltrative (tumors, amyloidosis, sarcoidosis)
Other Esophageal Abnormalities
- Esophageal Perforation:
- Commonly due to instrumentation or severe vomiting (Mallory-Weiss tear).
- Esophageal Varices:
- Dilated veins due to portal hypertension, prevalent in cirrhotic patients.
Inflammatory Disorders
- Infective:
- Fungal (Candida albicans), viral (Herpes, CMV).
- Physical agents:
- Radiation exposure, caustic substances.
- Reflux:
- Contributing factors include abdominal pressure, hiatus hernia, smoking, and alcohol.
Reflux Esophagitis
- Histological features include:
- Basal cell hyperplasia, eosinophils increase, elongated lamina propria papillae.
Esophagogastric Junction
- Location between esophagus and stomach.
- Contains:
- Squamous Mucosa: Protective against physical trauma.
- Glandular Mucosa: Produces mucus for acid protection.
Metaplasia in the Esophagus
- Chronic acid irritation leads to squamous to glandular mucosa transformation known as Barrett's esophagus.
- Long-segment Barrett's: Defined as more than 3 cm of columnar epithelium.
Barrett’s Oesophagus
- Characterized by a junction between squamous and glandular mucosa observed during Upper GI Endoscopy.
- Associated with persistent reflux in 3-12% of symptomatic patients.
- May develop dysplasia, leading to a risk of adenocarcinoma at approximately 0.5% per year.
- Requires regular surveillance endoscopy for early detection.
Oesophageal Tumours
- Benign tumours include leiomyomas, lipomas, and fibromas.
- Malignant primary tumours predominantly are epithelial, with squamous (70%) and glandular (25%) types.
- Other types include gastrointestinal stromal tumours (GIST) and secondary tumours.
- Clinical presentation often includes dysphagia, especially for solids, along with diagnostic methods like endoscopy and biopsy.
Squamous Cell Carcinoma (SCC)
- Most common in the mid third of the oesophagus.
- Histology shows keratinizing or non-keratinizing squamous lesions.
- Symptoms include dysphagia, odynophagia, and weight loss.
- Risk factors consist of dietary deficiencies, alcohol, tobacco use, chronic oesophagitis, achalasia, Plummer-Vinson syndrome, and genetic predispositions.
Adenocarcinoma
- Accounts for 85-90% of cases arising from Barrett's oesophagus, primarily located in the lower third of the oesophagus.
- Represents approximately half of all oesophageal malignancies, with a typical onset in the mid-60s.
Prognosis of Oesophageal Cancer
- Spread occurs locally, to lymph nodes, and through the bloodstream.
- Prognosis varies by stage:
- 5-year survival for local disease ~45%, nodal disease ~25%, and distant spread ~5%.
- Treatment options include neoadjuvant chemotherapy and radiotherapy, oesophageal resection (40% success), stenting, and adjuvant chemotherapy/radiotherapy.
Inflammatory Disorders of the Stomach: Acute Gastritis
- Causes include alcohol, NSAIDs, steroids, smoking, corrosives, stress, uraemia, and gastric irradiation.
- Presentation may be asymptomatic or include epigastric pain, nausea, vomiting, anaemia, and gastrointestinal bleeding.
- Histologically shows neutrophilic influx and oedema.
Chronic Gastritis
- Associated chronic mucosal changes lead to mucosal atrophy and epithelial metaplasia.
- Most prevalent types:
- Helicobacter-associated gastritis
- Autoimmune chronic gastritis
- Chemical/reflux gastritis
- Histology reveals lymphocyte and plasma cell infiltration.
Helicobacter-associated Gastritis
- Affects individuals at any age and primarily involves the antrum and corpus of the stomach.
- Caused by H. pylori, leading to epithelial damage, inflammation, and lymphoid aggregates.
- Increased risk for peptic ulcers and gastric cancer.
Autoimmune Chronic Gastritis
-
Typically affects the elderly with autoantibodies against parietal cells.
-
Associated with pernicious anaemia and increased gastric carcinoma risk (2-4%).Pernicious Anemia: It is a specific type of megaloblastic anemia caused by a vitamin B12 deficiency.
-
There is a decrease in gastric acid production due to the loss of parietal cells, a condition known as hypochlorhydria.
-
Autoimmune chronic gastritis is often seen in conjunction with other autoimmune diseases, including:
-Hashimoto’s thyroiditis (an autoimmune thyroid disorder).
-Addison's disease (an autoimmune condition affecting the adrenal glands).
-
-
Histological features include gland destruction and mucosal atrophy.
Chemical / Reflux Gastritis
- Results from the reflux of duodenal fluid and bile.
- Frequently occurs post-gastric surgery.
- Microscopy shows foveolar hyperplasia and fibromuscular changes.
intestinal metaplasia
- Associated with Chronic Gastritis
- refers to the transformation of gastric epithelium (the normal lining of the stomach) into intestinal-type epithelium. This means that the cells lining the stomach take on characteristics of those normally found in the small intestine.
- can progress to dysplasia
- Endoscopic Surveillance: Patients with intestinal metaplasia, especially those with chronic gastritis or a history of H. pylori infection, may require regular endoscopic surveillance.
Peptic Ulcer Disease
-
Caused by gastric acid affecting various sites, including the duodenum and stomach.
-
Represents a breach extending into the submucosa or deeper.
-
Risk factors include H. pylori infection, blood group A, family history, and Zollinger-Ellison syndrome.
-
Peptic ulcers: round-oval, sharply punched-out, straight walls, level margins, smooth base.
-
Surrounding mucosa appears oedematous and reddened.
-
Peptic ulcers – microscopic appearance
- Ulcer on microscob shows fibrosis in the base and walls; has three zones: superficial slough, chronically inflamed granulation tissue, deep fibrous scar.
- Vessel walls in scarred area may be thickened and occasionally thrombosed.
clinical presentation for gastric and duodenal ulcers:
Gastric Ulcers:
- Pain: Epigastric pain that tends to be worse at night or 1-3 hours after eating.
- Symptoms: Loss of appetite, weight loss, nausea, vomiting, bloating, belching.
- Pain Characteristics: Often constant, can be aggravated by food.
Duodenal Ulcers:
- Pain: Typically relieved by eating or antacids. Pain may refer to the back, chest, or left upper quadrant (LUQ).
- Symptoms: Iron-deficiency anemia, hematemesis (vomiting blood), melena (black tarry stools).
- Complications: Penetrating ulcers can cause severe pain and potential perforation.
Acute Gastric Ulcers (“Stress Ulcers”):
- Development: Arise from acute erosive gastritis due to severe stress or shock (e.g., Cushing’s, Curling’s ulcers from burns or trauma) and can be drug-induced.
- Microscopy: Ranges from erosion to ulceration, usually <1mm in size, single or multiple, without scarring or thickening of blood vessels.
- Outcomes:
- Severe bleeding.
- Typically heal without scarring within days to several weeks.
- May progress to chronic peptic ulcers.
- Key Determinant: The ability to correct the underlying condition significantly affects the outcome.
Benign Tumours of the Stomach:
- Polyp: A nodule or mass projecting above the mucosa, uncommon in the stomach.
- Hyperplastic Polyps (90%): Arise in chronic gastritis.
- Adenomas (5-10%): Dysplastic epithelium with malignant potential, can be sessile or pedunculated.
- Hamartomas: Includes Peutz-Jeghers and juvenile polyps.
- Fundic Gland Polyps.
- Lipomas.
- Schwannomas.
Malignant Tumours of the Stomach:
- Carcinoma: Most common (90-95%).
- Lymphoma: 4%.
- Carcinoid Tumours: 3%.
- Mesenchymal Tumours: 2%, including:
- GIST (Gastrointestinal Stromal Tumours): Range from benign to malignant.
- Leiomyosarcoma.
Gastric Carcinoma:
-
Histologically classified into intestinal and diffuse types.
-
Epidemiology: Common cause of cancer-related deaths (after lung and colon), with a male-to-female ratio of 2:1. More prevalent in East Asia (Japan, China).
-
Risk Factors:
- Dietary: Smoked & salted foods, low fruit and vegetables, nitrites (from food, water, meat preservation).
- Medical Conditions: Adenomatous polyps, pernicious anemia, prior partial gastrectomy, peptic ulcer disease.
- Infection: H. pylori.
- Metaplasia: Intestinal metaplasia.
- Genetic: Blood group A, family history.
Spread occurs locally, via lymphatics (with involvement of Virchow’s node), or haematogenously.
gastric Carcinoma Locations and Prevalence:
- Antrum: 50-60% (most common site).
- Body: 30-40%.
- Fundus: 5-10% (least common).
- Cardia: 10-20% (associated with Barrett’s esophagus and GERD).
Gastric Cancer Spread and Prognosis:
-
Spread:
- Local: Adjacent organs like duodenum, pancreas, retroperitoneum.
- Trans-coelomic: Krukenberg tumour in ovaries.
- Lymphatic: Virchow’s node (supraclavicular) and Troisier’s sign.
- Haematogenous: Bloodborne spread.
-
Prognosis:
- Localized: 70% 5-year survival.
- Regional: 30% 5-year survival.
- Distal (distant metastases): 5% 5-year survival.
- Overall 5-year survival rate: 32%.
Early Gastric Cancer
- Confined to mucosa or submucosa, regardless of lymph node status.
- Cure rates are high for intramucosal (93%) and submucosal cancers (80-89%).
Gastrointestinal Stromal Tumours (mesenchymal tumor)
-
Non-epithelial neoplasms arising from interstitial cells of Cajal. (“pacemakers” of the intestine)
-
Often associated with CD117 (c-kit) mutations; treated with tyrosine kinase inhibitors like Gleevec™.
-
Clinical features include:
Adults
Abdominal pain
Melaena
Rarely obstruction
Tumours of the Mouth
- Benign tumours include squamous papillomas linked to HPV types 6 & 11.
- Malignant cases are primarily squamous cell carcinomas, often found in the floor of mouth, tongue, and hard palate, with significant risk factors including tobacco and HPV 16/18.
Other Oral Conditions
- Aphthous ulcers may be associated with Crohn’s disease.
- Xerostomia (dry mouth) can be caused by autoimmune conditions or medications.
- Glossitis linked to nutritional deficiencies notably in vitamin B12 and iron or plummer-vinsion syndrom
- Leucoplakia (white plaque) poses a premalignant risk; hairy leukoplakia is HIV-associated with EBV infaection
- Erythroplakia has a high correlation with oral cancers, especially among smokers.
Salivary Glands Pathology
- Sialadenitis presents with sialorrhoea (excess saliva) and xerostomia.
- Benign tumours include pleomorphic adenomas (most common in parotid gland) and Warthin’s tumour.
- Malignant tumours are more frequently found in minor glands, often presenting with rapid growth and pain. Types include mucoepidermoid and adenoid cystic carcinoma.
Tumours of the Mouth
- Benign lesions include squamous papillomas associated with HPV types 6 and 11.
- Malignant tumours are primarily squamous cell carcinoma (>95%), linked to tobacco, alcohol, HPV types 16 and 18, and environmental factors.
Other Oral Conditions
- Aphthous Ulcers: May be related to Crohn’s disease.
- Xerostomia: Dry mouth resulting from autoimmune conditions, medications, or radiation.
- Glossitis: Deficiencies in B12 and iron; associated with Plummer-Vinson syndrome.
- Leucoplakia: White plaque not removable by scraping; cause unclear.
- Erythroplakia: Red, velvety patch with a high risk of malignancy; common in smokers and males.
Salivary Glands:
- Secrete proteins and fluid, categorized as mucinous or mixed.
- Ducts lined by cuboidal epithelium.
Pathology of Salivary Glands:
-
Inflammation (Sialadenitis):
- Can lead to Sialorrhoea (excessive saliva) or Xerostomia (dry mouth).
- Parotid gland involvement:
- Viral (e.g., mumps).
- Suppurative (e.g., Staphylococcus aureus).
- Autoimmune (e.g., Sjogren’s syndrome).
-
Tumours:
- Can be either benign or malignant.
Benign Tumours
-
Typically present as painless swelling.
-
Pleomorphic Adenoma: Most common parotid tumour.
- More frequent in females than males.
- Encapsulated structure with epithelial elements embedded in mucoid and chondroid stroma.
- Treated through wide excision; however, local recurrence is common.
- Difficult to completely excise, with a 25% chance of nucleation.
- Risk of malignant transformation occurs in approximately 2%.
-
Warthin’s Tumour: Accounts for 10% of parotid tumours.
- Predominantly found in older males, especially smokers.
- Features include a double layer of epithelial cells in a dense lymphoid stroma, with oncocytes and secretory cells, possibly exhibiting squamous metaplasia.
- Known as "adenolymphoma."
- Multifocality and bilateral occurrence found in 10% of cases.
Malignant Tumours
- More frequently observed in minor salivary glands.
- Indications of malignancy include rapid growth and pain.
- Types of Malignant Tumours:
- Mucoepidermoid Carcinoma: Composed of glandular and squamous cells.
- Adenoid Cystic Carcinoma: Characterized by cribriform, solid, and tubular gland formations, often with perineural invasion.
- Acinic Cell Carcinoma: Resembles normal acinar cells.
- Carcinoma ex Pleomorphic Adenoma: Originates from benign pleomorphic adenomas, transforming into malignant forms.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.