Podcast
Questions and Answers
What is the most common complication associated with peptic ulcers?
What is the most common complication associated with peptic ulcers?
- Bleeding (correct)
- Outlet obstruction
- Chemical inflammation
- Perforation
Which of the following conditions is NOT associated with inflammation of the mouth?
Which of the following conditions is NOT associated with inflammation of the mouth?
- Gingivitis
- Esophagitis (correct)
- Parotiditis
- Glossitis
Which type of ulcer is more frequently located in the first portion of the duodenum?
Which type of ulcer is more frequently located in the first portion of the duodenum?
- Stress ulcer
- Duodenal ulcer (correct)
- Gastric ulcer
- NSAID-induced ulcer
What is the most appropriate initial manifestation found in esophageal stenosis?
What is the most appropriate initial manifestation found in esophageal stenosis?
Which of the following diseases can result from motor impairment of the upper gastrointestinal system?
Which of the following diseases can result from motor impairment of the upper gastrointestinal system?
At what age do gastric ulcers typically occur?
At what age do gastric ulcers typically occur?
Which symptom is often associated with duodenal ulcers and may awaken the patient?
Which symptom is often associated with duodenal ulcers and may awaken the patient?
In the context of upper GI pathology, which diagnostic tool is primarily used for both visualization and intervention?
In the context of upper GI pathology, which diagnostic tool is primarily used for both visualization and intervention?
Which patient group is more likely to experience perforation as a complication of peptic ulcer disease?
Which patient group is more likely to experience perforation as a complication of peptic ulcer disease?
Which upper GI manifestation is defined by the presence of acid and bile without distention?
Which upper GI manifestation is defined by the presence of acid and bile without distention?
What would be a common symptom of outlet obstruction due to peptic ulcers?
What would be a common symptom of outlet obstruction due to peptic ulcers?
Among the following neoplasms, which type is least likely to be found in the mouth?
Among the following neoplasms, which type is least likely to be found in the mouth?
Which source accounts for upper gastrointestinal bleeding other than peptic ulcers?
Which source accounts for upper gastrointestinal bleeding other than peptic ulcers?
What condition involves the inability to coordinate the movements necessary for swallowing?
What condition involves the inability to coordinate the movements necessary for swallowing?
What is the typical mortality rate associated with upper GI bleeding?
What is the typical mortality rate associated with upper GI bleeding?
Which anatomical alteration is characterized by a failure to connect the upper and lower parts of the esophagus?
Which anatomical alteration is characterized by a failure to connect the upper and lower parts of the esophagus?
Which statement accurately describes the pathophysiology of achalasia?
Which statement accurately describes the pathophysiology of achalasia?
What is a key symptom of gastroesophageal reflux disease (GERD)?
What is a key symptom of gastroesophageal reflux disease (GERD)?
Which diagnostic method is appropriate for diagnosing a hiatal hernia?
Which diagnostic method is appropriate for diagnosing a hiatal hernia?
What type of surgical treatment is often recommended for severe cases of GERD?
What type of surgical treatment is often recommended for severe cases of GERD?
What is a common cause of secondary gastroparesis?
What is a common cause of secondary gastroparesis?
Which type of esophageal cancer is mentioned as a common neoplasm?
Which type of esophageal cancer is mentioned as a common neoplasm?
What is a characteristic symptom of cancer that arises in the esophagus or stomach?
What is a characteristic symptom of cancer that arises in the esophagus or stomach?
Which statement best describes the treatment options for achalasia?
Which statement best describes the treatment options for achalasia?
What is the primary role of prostaglandins in the stomach?
What is the primary role of prostaglandins in the stomach?
Which of the following is NOT a cause of acute gastritis?
Which of the following is NOT a cause of acute gastritis?
What are the main characteristics of Menetrier’s disease?
What are the main characteristics of Menetrier’s disease?
Which type of ulcer is most commonly found in the first portion of the duodenum?
Which type of ulcer is most commonly found in the first portion of the duodenum?
What condition is primarily associated with autoimmune chronic gastritis?
What condition is primarily associated with autoimmune chronic gastritis?
Which of the following consequences is NOT associated with H.pylori infection?
Which of the following consequences is NOT associated with H.pylori infection?
Which statement about gastric ulcers is accurate?
Which statement about gastric ulcers is accurate?
Which statement accurately describes the treatment approach for neoplasms associated with H.pylori?
Which statement accurately describes the treatment approach for neoplasms associated with H.pylori?
Flashcards
Duodenoyeyunal Flexure (Angle of Treitz)
Duodenoyeyunal Flexure (Angle of Treitz)
The point where the duodenum joins the jejunum, marked by the suspensory muscle of the duodenum (Treitz ligament).
Vomits without distention in upper GI obstruction
Vomits without distention in upper GI obstruction
Distention refers to swelling or inflation, so 'vomits without distention' means vomiting without bloating or fullness.
Gingivitis and Dental Caries
Gingivitis and Dental Caries
Inflammation of the gums and decay of teeth.
Glossitis
Glossitis
Signup and view all the flashcards
Tonsilitis
Tonsilitis
Signup and view all the flashcards
Pharyngitis
Pharyngitis
Signup and view all the flashcards
Parotiditis
Parotiditis
Signup and view all the flashcards
Chewing Impairment (Dysphagia)
Chewing Impairment (Dysphagia)
Signup and view all the flashcards
Achalasia?
Achalasia?
Signup and view all the flashcards
GERD?
GERD?
Signup and view all the flashcards
Hiatal Hernia?
Hiatal Hernia?
Signup and view all the flashcards
Esophagus or Stomach Cancer?
Esophagus or Stomach Cancer?
Signup and view all the flashcards
Gastritis?
Gastritis?
Signup and view all the flashcards
Gastroparesis?
Gastroparesis?
Signup and view all the flashcards
Stomach Problems?
Stomach Problems?
Signup and view all the flashcards
Lower Esophageal Sphincter (LES)?
Lower Esophageal Sphincter (LES)?
Signup and view all the flashcards
Duodenal Ulcer
Duodenal Ulcer
Signup and view all the flashcards
Gastric Ulcer
Gastric Ulcer
Signup and view all the flashcards
Epigastric Pain
Epigastric Pain
Signup and view all the flashcards
Ulcer Perforation
Ulcer Perforation
Signup and view all the flashcards
Peptic Ulcer Outlet Obstruction
Peptic Ulcer Outlet Obstruction
Signup and view all the flashcards
Peptic Ulcer Bleeding
Peptic Ulcer Bleeding
Signup and view all the flashcards
Upper GI Bleeding
Upper GI Bleeding
Signup and view all the flashcards
Esophageal Varices
Esophageal Varices
Signup and view all the flashcards
What is the role of prostaglandins in the stomach?
What is the role of prostaglandins in the stomach?
Signup and view all the flashcards
How do NSAIDs and corticosteroids affect prostaglandins?
How do NSAIDs and corticosteroids affect prostaglandins?
Signup and view all the flashcards
What is H. pylori and what are its consequences?
What is H. pylori and what are its consequences?
Signup and view all the flashcards
What is chronic gastritis?
What is chronic gastritis?
Signup and view all the flashcards
What are peptic ulcers and what are their causes?
What are peptic ulcers and what are their causes?
Signup and view all the flashcards
What are some characteristics of duodenal ulcers?
What are some characteristics of duodenal ulcers?
Signup and view all the flashcards
What are some characteristics of gastric ulcers?
What are some characteristics of gastric ulcers?
Signup and view all the flashcards
What is a unique characteristic of MALT lymphoma?
What is a unique characteristic of MALT lymphoma?
Signup and view all the flashcards
Study Notes
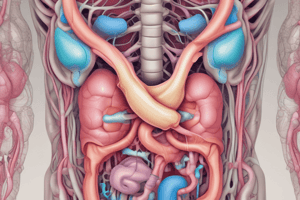
Upper GI Pathology
- Upper GI system encompasses the organs from the mouth to the duodenum.
- Learning objectives include clinical presentations of upper GI diseases, characterizing the upper GI system, and introducing diseases of the esophagus, stomach, and duodenum.
Upper GI System
- Duodenoyeyunal flexure (Angle of Treitz): The junction of the duodenum and jejunum.
- Suspensory muscle of the duodenum (Treitz ligament): Anatomical structure in this region.
- Duodenum blockage: Potentially occurs due the superior mesenteric artery.
Clinical Manifestations
- Bleeding: A symptom associated with upper GI diseases.
- Obstruction: Characterized by vomiting without abdominal distension, often involving acid and bile.
- Acid and bile: Found in vomitus in certain cases of upper GI obstruction.
Diagnostic Implications
- Upper GI endoscopy: Diagnostic tool for upper GI pathology.
- ERCP (Endoscopic Retrograde Cholangiopancreatography) and ultrasonography: Used in conjunction with endoscopy for comprehensive assessment.
Mouth
- Inflammatory conditions: Gingivitis, dental caries, glossitis, tonsilitis, pharyngitis, and parotiditis.
- Infections and other factors: Infections, radiation exposure, and autoimmune diseases can cause mouth inflammation.
- Motor impairment: Difficulties with chewing and swallowing (dysphagia).
- Neuropathies, myopathies and Collagenopathies: Related to nerve, muscle or connective tissue diseases.
- Salivation disturbances: Disruptions in saliva production, often linked to inflammation, obstructions or tumors.
- Neoplasms: Epidermoid carcinoma, lymphoma, Kaposi's sarcoma are potential cancers affecting the mouth.
Esophagus
- Inflammations (esophagitis): Infections, radiation therapy, and autoimmune disorders often lead to esophageal inflammation.
- Motor impairment: Affecting swallowing (dysphagia), often due to conditions involving nerves, muscles or connective tissue.
- Neoplasms: Epidermoid carcinoma, adenocarcinoma, and lymphoma are examples of esophageal cancers.
- Anatomical alterations: Fistulas, atresia, and perforations can be present in the esophagus.
- Tumors and cysts: Malignant and benign lesions in the esophagus.
Dysphagia
- Oropharyngeal dysphagia: Issues with initial stages of swallowing (movement coordination, swallowing initiation, choking, and aspiration).
- Esophageal stenosis: Difficulty swallowing, progressing from solids to liquids, and resulting in food retention and regurgitation.
Esophago-gastric Junction
- Achalasia: Condition impacting the lower esophageal sphincter (LES).
- GERD (Gastroesophageal reflux disease): Stomach contents returning to the esophagus, leading to symptoms like heartburn and regurgitation.
- Hiatal hernia: Passage of abdominal contents through the esophageal hiatus; can produce GERD-like symptoms.
- Cancer: Cancers impacting the esophagogastric junction
Achalasia
- Reduced ganglionic cells in LES: Leading to hypertonic LES.
- Progressive dysphagia: Swallowing difficulty worsening over time.
- Esophageal dilation: Enlargement of the esophagus.
- Diagnosis: Manometry, biopsy
- Treatment: Dilatation, sphincterotomy
GERD
- Hypotonic LES: Lower esophageal sphincter doesn't function effectively, allowing stomach contents to reflux.
- Symptoms: Heartburn, regurgitation, and nonspecific symptoms.
- Esophagitis and Barrett's esophagus: Inflammation and precancerous changes in the esophagus.
- Diagnosis: pH monitoring, endoscopy
- Treatment: Medications (PPIs), dietary changes, fundoplication
Hiatal Hernia
- Passage of abdominal contents through esophageal hiatus: Portion of stomach protruding into the chest.
- Types of hiatal hernias: Sliding, paraesophageal, and mixed.
- Symptoms: Can cause GERD-like symptoms; symptoms may depend on the type of hernia.
- Diagnosis: Upper endoscopy, gastrointestinal transit studies.
- Treatment: Medications, dietary changes, fundoplication.
Cancer
- Neoplasms (cancers) in the esophagus and stomach: Epidermoid carcinoma, adenocarcinoma.
- Symptoms: Obstruction, weight loss, and distant disease.
- Diagnosis: Endoscopy and imaging techniques assessing distant disease.
- Treatment: Surgery, chemotherapy, radiation therapy, and palliative care.
Stomach
- Inflammations (Gastritis): Acute or chronic conditions, including infections, drug reactions, and autoimmune diseases can all lead to gastric inflammation.
- Motor impairment (Gastroparesis): Slowed emptying of the stomach, causing symptoms like nausea, vomiting, and early satiety (feeling full quickly).
- Neoplasms: Adenocarcinoma, GIST (Gastrointestinal stromal tumor) and MALT (mucosa-associated lymphoid tissue).
- Anatomical alterations/ulcers: Ulcers of the stomach lining.
- Pyloric obstruction: Blockage of the stomach opening (pylorus) to the small intestine.
Gastroparesis - Causes and Diagnosis
- Defective gastric emptying without physical obstruction: Stomach cannot empty properly.
- Types of gastroparesis: Primary (related to gastric pacemaker dysfunction), secondary (due to autonomic nerve dysfunction, muscular disorders, medications).
- Diagnostic tests: History, physical examination, motility studies like gastric emptying tests.
Acute and chronic Gastritis
- Acute gastritis: Sudden inflammation of the stomach, often caused by NSAIDs, alcohol, or infections like H. pylori.
- Chronic gastritis: Long-term inflammation, can be associated with autoimmune conditions or persistent infections.
- Pernicious anemia: Deficiency in Vitamin B12.
- Menetrier's disease: Characterized by inflammation.
- Specific systemic diseases: e.g Crohn's disease
Helicobacter pylori (H. pylori)
- Gram-negative spiral bacteria: Causes gastritis.
- Adhesion proteins: Aid bacterial attachment to gastric mucosa.
- Urease enzyme: Facilitates bacterial survival in the stomach's acidic environment.
- Toxins: GagA, VacA cause inflammation.
- Pathology: Acute and chronic gastritis, peptic ulcers, and stomach cancer.
Peptic Ulcer
- Duodenal ulcers: Most frequent type.
- Gastric ulcers: Occur later in life; often asymptomatic.
- Clinical manifestations: Epigastric pain or discomfort (often relieved by food).
- Diagnosis: Endoscopy.
Complications of Peptic Ulcer
- Perforation: A serious complication, potentially fatal.
- Outlet obstruction: Narrowing of the pyloric opening.
- Bleeding: Significant blood loss, potentially life-threatening.
- Penetration and fistulas: Perforation of adjacent organs leading to an abnormal connection or fistula.
Upper GI Bleeding
- Most common GI emergency: Represents a significant clinical concern.
- Mortality: Can range from 10%.
- Causes: Varices (due to liver disease), peptic ulcers, hiatal hernias, gastric cancers, and vascular malformations.
- Clinical manifestations: Hematemesis (vomiting blood), melena (black, tarry stools), hematochezia (bright red blood in stools), and cardiovascular compromise.
- Management: Endoscopy, resuscitation, surgical interventions (e.g., Sengstaken-Blakemore tube), and consideration of liver transplantation in certain cases.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.