Podcast
Questions and Answers
What is the primary function of the stomach in the GI tract?
What is the primary function of the stomach in the GI tract?
- Mixing food with digestive enzymes (correct)
- Absorbing nutrients into the bloodstream
- Storing food for later digestion
- Breaking down proteins into peptides
Which of the following pathologies is related to the gastric mucosal mechanisms of acid secretion and mucosal protection?
Which of the following pathologies is related to the gastric mucosal mechanisms of acid secretion and mucosal protection?
- Pyloric stenosis
- Peptic ulcers (correct)
- Gastroesophageal reflux disease
- Acute pancreatitis
What is the primary mechanism of digestion and absorption in the GI tract?
What is the primary mechanism of digestion and absorption in the GI tract?
- Mechanical breakdown of food by teeth and stomach contractions
- Elimination of waste products through the anus
- Absorption of nutrients through the intestinal walls
- Chemical breakdown of food by enzymes and acids (correct)
Which of the following is NOT a pathology related to the stomach's function?
Which of the following is NOT a pathology related to the stomach's function?
What is the primary clinical sign of a GI pathology?
What is the primary clinical sign of a GI pathology?
Which part of the brain is responsible for the vomiting reflex?
Which part of the brain is responsible for the vomiting reflex?
What is the term for bloody stools?
What is the term for bloody stools?
What is the most common mechanism of abdominal pain in gastrointestinal disorders?
What is the most common mechanism of abdominal pain in gastrointestinal disorders?
Which layer of the gastrointestinal tract is most commonly affected by pathology?
Which layer of the gastrointestinal tract is most commonly affected by pathology?
What is the term for a connection between the trachea and esophagus?
What is the term for a connection between the trachea and esophagus?
Which of the following is NOT a mechanism of gastrointestinal dysfunction?
Which of the following is NOT a mechanism of gastrointestinal dysfunction?
What is the term for the sensation of nausea associated with a number of conditions?
What is the term for the sensation of nausea associated with a number of conditions?
Which of the following is a complication of gastrointestinal bleeding?
Which of the following is a complication of gastrointestinal bleeding?
What is the term for the passage of bright red blood per rectum?
What is the term for the passage of bright red blood per rectum?
Which of the following is a congenital anomaly that can affect the esophagus?
Which of the following is a congenital anomaly that can affect the esophagus?
What percentage of adults in developed countries are infected with H. pylori?
What percentage of adults in developed countries are infected with H. pylori?
What is the primary effect of H. pylori infection on the cardia?
What is the primary effect of H. pylori infection on the cardia?
What is the primary effect of H. pylori infection on the antrum?
What is the primary effect of H. pylori infection on the antrum?
What is the primary effect of H. pylori infection on the fundus and body?
What is the primary effect of H. pylori infection on the fundus and body?
What is the term for the clinical combination of duodenal ulcers and a pancreatic gastrin tumor?
What is the term for the clinical combination of duodenal ulcers and a pancreatic gastrin tumor?
What is the term for a gastrin-secreting tumor that can occur in the pancreas or the duodenum?
What is the term for a gastrin-secreting tumor that can occur in the pancreas or the duodenum?
What is the primary effect of somatostatin on HCL production?
What is the primary effect of somatostatin on HCL production?
What is the primary effect of anticholinergics on HCL production?
What is the primary effect of anticholinergics on HCL production?
What is the primary effect of H2 blockers on HCL production?
What is the primary effect of H2 blockers on HCL production?
What is the condition characterized by delayed gastric emptying?
What is the condition characterized by delayed gastric emptying?
What percentage of Europeans continue to produce lactase enzyme throughout their lives?
What percentage of Europeans continue to produce lactase enzyme throughout their lives?
What is the result of bile salt deficiency in the small intestine?
What is the result of bile salt deficiency in the small intestine?
What is the common characteristic of lesions in Ulcerative Colitis?
What is the common characteristic of lesions in Ulcerative Colitis?
What is the primary treatment for dumping syndrome?
What is the primary treatment for dumping syndrome?
What is the result of malabsorption of vitamin B12 and folic acid in Crohn Disease?
What is the result of malabsorption of vitamin B12 and folic acid in Crohn Disease?
What is the characteristic appearance of lesions in Crohn Disease?
What is the characteristic appearance of lesions in Crohn Disease?
What is the primary complication of bile salt deficiency?
What is the primary complication of bile salt deficiency?
What is the treatment for bile salt deficiency?
What is the treatment for bile salt deficiency?
What is the common characteristic of Inflammatory Bowel Disease?
What is the common characteristic of Inflammatory Bowel Disease?
What is the primary manifestation of dumping syndrome?
What is the primary manifestation of dumping syndrome?
What is the fate of amniotic fluid during fetal development?
What is the fate of amniotic fluid during fetal development?
What is the primary predisposing factor for the development of gastroparesis?
What is the primary predisposing factor for the development of gastroparesis?
What is the term for the narrowing of the esophagus, typically caused by mucosal inflammation and scarring?
What is the term for the narrowing of the esophagus, typically caused by mucosal inflammation and scarring?
What is the term for the mass of hardened, undigested food or other material trapped in the digestive system?
What is the term for the mass of hardened, undigested food or other material trapped in the digestive system?
What is the primary cause of esophagitis?
What is the primary cause of esophagitis?
What is the term for the growth of columnar epithelium with goblet cells in the lower esophagus, typically caused by chronic acid reflux?
What is the term for the growth of columnar epithelium with goblet cells in the lower esophagus, typically caused by chronic acid reflux?
What is the primary mechanism by which the kidney responds to decreased blood volume and pH imbalances in pyloric stenosis?
What is the primary mechanism by which the kidney responds to decreased blood volume and pH imbalances in pyloric stenosis?
What is the primary function of mucous cells in the stomach?
What is the primary function of mucous cells in the stomach?
What is the term for the obstruction of the opening between the stomach and duodenum, which can be acquired or congenital?
What is the term for the obstruction of the opening between the stomach and duodenum, which can be acquired or congenital?
What is the primary site of delivery for the pancreas, liver, and gallbladder?
What is the primary site of delivery for the pancreas, liver, and gallbladder?
What is the term for the inflammation of the gastric mucosa?
What is the term for the inflammation of the gastric mucosa?
What is the primary cause of peptic ulcer disease?
What is the primary cause of peptic ulcer disease?
What is the term for the hypertrophy of the pyloric sphincter, which can occur in babies and adults?
What is the term for the hypertrophy of the pyloric sphincter, which can occur in babies and adults?
What is the function of the spleen in the immune system?
What is the function of the spleen in the immune system?
What is the term for the abnormal connection between the esophagus and trachea?
What is the term for the abnormal connection between the esophagus and trachea?
What is the symptom of esophageal achalasia that is characterized by a distended 'megaesophagus' with disordered, ineffective movement?
What is the symptom of esophageal achalasia that is characterized by a distended 'megaesophagus' with disordered, ineffective movement?
What is the term for the classic symptom of pyloric stenosis in babies, characterized by vomiting that is non-bilious and projectile?
What is the term for the classic symptom of pyloric stenosis in babies, characterized by vomiting that is non-bilious and projectile?
What is the primary area affected in Crohn Disease?
What is the primary area affected in Crohn Disease?
What is the term for the condition in which the stomach empties slowly, leading to delayed gastric emptying?
What is the term for the condition in which the stomach empties slowly, leading to delayed gastric emptying?
What is the primary site of acid neutralization in the small intestine?
What is the primary site of acid neutralization in the small intestine?
What is the term for the sensation of incomplete emptying after a bowel movement?
What is the term for the sensation of incomplete emptying after a bowel movement?
What is the term for the physical sign of pyloric stenosis in adults, characterized by a mass in the epigastric region?
What is the term for the physical sign of pyloric stenosis in adults, characterized by a mass in the epigastric region?
What is the term for the blockage of the small or large bowel, resulting in the inability of contents to pass through?
What is the term for the blockage of the small or large bowel, resulting in the inability of contents to pass through?
What is the term for hard, dry stool retained in the rectum?
What is the term for hard, dry stool retained in the rectum?
Which of the following is a risk factor for Mechanical Bowel Obstruction?
Which of the following is a risk factor for Mechanical Bowel Obstruction?
What is the term for the connection between the gut and the peritoneum, which can occur in Mechanical Bowel Obstruction?
What is the term for the connection between the gut and the peritoneum, which can occur in Mechanical Bowel Obstruction?
What is the location of the pancreatic head in relation to the duodenum?
What is the location of the pancreatic head in relation to the duodenum?
What is the primary function of Brunner's glands in the proximal duodenum?
What is the primary function of Brunner's glands in the proximal duodenum?
What is the characteristic of retroperitoneal organs?
What is the characteristic of retroperitoneal organs?
What is the length of the pancreas?
What is the length of the pancreas?
What is the primary function of the pancreatic duct system?
What is the primary function of the pancreatic duct system?
What is the result of zymogens activating early in the pancreas?
What is the result of zymogens activating early in the pancreas?
What is the characteristic of pancreatic pain due to the retroperitoneal location?
What is the characteristic of pancreatic pain due to the retroperitoneal location?
What is the consequence of a ductal blockage in the pancreas?
What is the consequence of a ductal blockage in the pancreas?
What is the histological feature of the gallbladder?
What is the histological feature of the gallbladder?
What is the result of pancreatitis?
What is the result of pancreatitis?
What is the primary function of the muscularis externa in the gallbladder?
What is the primary function of the muscularis externa in the gallbladder?
What is the primary route of bile entry into the gallbladder?
What is the primary route of bile entry into the gallbladder?
What is the primary composition of cholesterol gallstones?
What is the primary composition of cholesterol gallstones?
What is the primary risk factor for the development of gallstones?
What is the primary risk factor for the development of gallstones?
What is the primary complication of symptomatic gallstones?
What is the primary complication of symptomatic gallstones?
What is the primary difference between maldigestion and malabsorption?
What is the primary difference between maldigestion and malabsorption?
What is the primary cause of lactose intolerance?
What is the primary cause of lactose intolerance?
What is the primary treatment for maldigestion due to pancreatic insufficiency?
What is the primary treatment for maldigestion due to pancreatic insufficiency?
What is the primary effect of 'gallbladder sludge' on gallstone formation?
What is the primary effect of 'gallbladder sludge' on gallstone formation?
What is the primary consequence of a blocked exit in the biliary tree?
What is the primary consequence of a blocked exit in the biliary tree?
What is the primary characteristic of anorexia nervosa?
What is the primary characteristic of anorexia nervosa?
What is the term for a condition that prevents proper digestion or absorption, or significantly increases metabolic consumption?
What is the term for a condition that prevents proper digestion or absorption, or significantly increases metabolic consumption?
Which of the following is a symptom of bulimia nervosa?
Which of the following is a symptom of bulimia nervosa?
What is the primary cause of malnutrition?
What is the primary cause of malnutrition?
Which of the following is NOT a characteristic of anorexia nervosa?
Which of the following is NOT a characteristic of anorexia nervosa?
Which vitamin is particularly prone to deficiency in individuals with alcoholism?
Which vitamin is particularly prone to deficiency in individuals with alcoholism?
What is the primary source of energy for the brain?
What is the primary source of energy for the brain?
Which vitamin is essential for the coagulation of blood?
Which vitamin is essential for the coagulation of blood?
Which mineral is required for the oxygen-carrying capacity of red blood cells?
Which mineral is required for the oxygen-carrying capacity of red blood cells?
What is the term for the deficiency of vitamin C?
What is the term for the deficiency of vitamin C?
Which of the following is a high-risk population for vitamin D deficiency?
Which of the following is a high-risk population for vitamin D deficiency?
What is the primary function of vitamin K in the body?
What is the primary function of vitamin K in the body?
What is the recommended supplementation for all neonates within 1 hour of birth?
What is the recommended supplementation for all neonates within 1 hour of birth?
Which of the following is a clinical sign of a nutritional deficiency?
Which of the following is a clinical sign of a nutritional deficiency?
What is the primary effect of thiamine deficiency on the brain?
What is the primary effect of thiamine deficiency on the brain?
What is the primary function of vitamin C in the human body?
What is the primary function of vitamin C in the human body?
What is the primary cause of vitamin B12 deficiency in patients with a history of gastric bypass surgery?
What is the primary cause of vitamin B12 deficiency in patients with a history of gastric bypass surgery?
What is the primary function of folic acid in the human body?
What is the primary function of folic acid in the human body?
What is the primary cause of thiamine (vitamin B1) deficiency?
What is the primary cause of thiamine (vitamin B1) deficiency?
What is the primary manifestation of Wernicke's encephalopathy, a degenerative brain disorder caused by thiamine deficiency?
What is the primary manifestation of Wernicke's encephalopathy, a degenerative brain disorder caused by thiamine deficiency?
What is the primary function of vitamin C in the absorption of nonheme iron?
What is the primary function of vitamin C in the absorption of nonheme iron?
What is the primary cause of folate deficiency in patients with celiac disease?
What is the primary cause of folate deficiency in patients with celiac disease?
What is the primary effect of vitamin B12 deficiency on the nervous system?
What is the primary effect of vitamin B12 deficiency on the nervous system?
What is the primary function of intrinsic factor in the stomach?
What is the primary function of intrinsic factor in the stomach?
What is the primary cause of iron deficiency in patients with intestinal disease?
What is the primary cause of iron deficiency in patients with intestinal disease?
What is the purpose of exposing lymphocytes to 'self' during education?
What is the purpose of exposing lymphocytes to 'self' during education?
Which type of T cell regulates the immune response?
Which type of T cell regulates the immune response?
What is the function of cytotoxic T cells?
What is the function of cytotoxic T cells?
Where do B cells mature?
Where do B cells mature?
What is the function of regulatory T cells?
What is the function of regulatory T cells?
Where do T cells mature?
Where do T cells mature?
What type of immunity is primarily responsible for protection against many bacteria and viruses?
What type of immunity is primarily responsible for protection against many bacteria and viruses?
What is the primary function of Helper T-cells?
What is the primary function of Helper T-cells?
What type of receptors are found on the surface of B-cells?
What type of receptors are found on the surface of B-cells?
What is the primary function of Cytotoxic T cells?
What is the primary function of Cytotoxic T cells?
What is the term for the process by which B-cells mature into plasma cells and start producing antibodies?
What is the term for the process by which B-cells mature into plasma cells and start producing antibodies?
What is the primary function of IgM in the early stages of B-cell mediated immunity?
What is the primary function of IgM in the early stages of B-cell mediated immunity?
What is the function of the variable region of an antibody?
What is the function of the variable region of an antibody?
Which class of antibody is responsible for neutralizing antigens in the early stages of B-cell mediated immunity?
Which class of antibody is responsible for neutralizing antigens in the early stages of B-cell mediated immunity?
What is the primary function of IgA in the body?
What is the primary function of IgA in the body?
What is the primary mechanism of IgE-mediated immunity?
What is the primary mechanism of IgE-mediated immunity?
What is the primary function of the constant region of an antibody?
What is the primary function of the constant region of an antibody?
What is the primary function of T cells?
What is the primary function of T cells?
What is the role of MHC Class II molecules?
What is the role of MHC Class II molecules?
What is the function of IgE antibodies?
What is the function of IgE antibodies?
What is the role of professional antigen-presenting cells (APCs)?
What is the role of professional antigen-presenting cells (APCs)?
What is the difference between MHC Class I and MHC Class II molecules?
What is the difference between MHC Class I and MHC Class II molecules?
What is the function of cytotoxic T cells?
What is the function of cytotoxic T cells?
What is the role of helper T cells?
What is the role of helper T cells?
What is the function of natural killer cells?
What is the function of natural killer cells?
What is the term for the molecules that are unique to each individual and help to identify cells as 'self'?
What is the term for the molecules that are unique to each individual and help to identify cells as 'self'?
What is the role of IgA antibodies?
What is the role of IgA antibodies?
What is the primary function of NK cells in the immune system?
What is the primary function of NK cells in the immune system?
What is the significance of IgM and IgG antibodies in the immune response?
What is the significance of IgM and IgG antibodies in the immune response?
What is the primary function of memory B cells in the immune system?
What is the primary function of memory B cells in the immune system?
What is the significance of the secondary immune response?
What is the significance of the secondary immune response?
What is the primary difference between IgM and IgG antibodies?
What is the primary difference between IgM and IgG antibodies?
What is the primary function of helper T cells in the immune system?
What is the primary function of helper T cells in the immune system?
What is the significance of affinity maturation in the immune response?
What is the significance of affinity maturation in the immune response?
What is the primary function of Fc receptors on NK cells?
What is the primary function of Fc receptors on NK cells?
What is the primary difference between the primary and secondary immune responses?
What is the primary difference between the primary and secondary immune responses?
What is the significance of memory cells in the immune response?
What is the significance of memory cells in the immune response?
What type of immunity is acquired through the introduction of a microorganism or its antigens, inducing an immune response and production of memory cells?
What type of immunity is acquired through the introduction of a microorganism or its antigens, inducing an immune response and production of memory cells?
What type of antibodies are produced in response to vaccination, providing long-term immunity?
What type of antibodies are produced in response to vaccination, providing long-term immunity?
What is the specific antigen used in the Hepatitis B vaccine?
What is the specific antigen used in the Hepatitis B vaccine?
What is the main difference between active and passive immunity?
What is the main difference between active and passive immunity?
What is the function of immunologic memory?
What is the function of immunologic memory?
What is the result of having low titers of IgG antibodies against Hepatitis B?
What is the result of having low titers of IgG antibodies against Hepatitis B?
What happens when someone with type A blood receives a transfusion of type B blood?
What happens when someone with type A blood receives a transfusion of type B blood?
What is the term for the immunologic disorder that occurs in an Rh-negative patient carrying an Rh-positive fetus?
What is the term for the immunologic disorder that occurs in an Rh-negative patient carrying an Rh-positive fetus?
What is the most important carbohydrate system for transfusion reactions?
What is the most important carbohydrate system for transfusion reactions?
What is the universal donor blood type?
What is the universal donor blood type?
What is the percentage of cases of Rh Isoimmunization caused by D antibodies?
What is the percentage of cases of Rh Isoimmunization caused by D antibodies?
What is the term for the symptoms of a transfusion reaction, including itchiness, hemolysis, allergy, and alloimmunization?
What is the term for the symptoms of a transfusion reaction, including itchiness, hemolysis, allergy, and alloimmunization?
What is the primary mechanism of immune tolerance during fetal and early postnatal life?
What is the primary mechanism of immune tolerance during fetal and early postnatal life?
What is the primary function of Helper T cells in the immune response?
What is the primary function of Helper T cells in the immune response?
What is the primary characteristic of autoimmune diseases?
What is the primary characteristic of autoimmune diseases?
What is the target of the Human Immunodeficiency Virus (HIV)?
What is the target of the Human Immunodeficiency Virus (HIV)?
What is the primary effect of HIV on the immune system?
What is the primary effect of HIV on the immune system?
What is the primary mechanism of immune response against Hepatitis B infection?
What is the primary mechanism of immune response against Hepatitis B infection?
What is the primary consequence of a failure to develop immune tolerance?
What is the primary consequence of a failure to develop immune tolerance?
What is the primary function of B cells in the immune response?
What is the primary function of B cells in the immune response?
What is the primary characteristic of immunodeficiency diseases?
What is the primary characteristic of immunodeficiency diseases?
What is the primary cause of chronic Hepatitis B infection?
What is the primary cause of chronic Hepatitis B infection?
Flashcards are hidden until you start studying
Study Notes
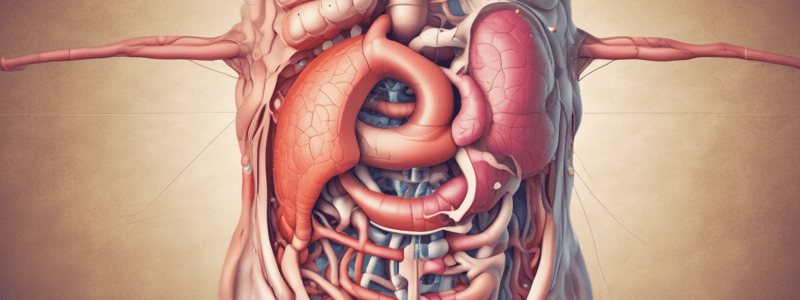
GI Pathophysiology
- Clinical signs of a GI pathology are not directly observable in pictures.
- Clinical manifestations of GI dysfunction:
- Anorexia (loss of appetite)
- Nausea (subjective experience associated with multiple conditions)
- Vomiting (forceful emptying of the stomach and intestinal contents through the mouth)
- Pain (can be caused by stretching, inflammation, or ischemia)
- Constipation
- Diarrhea
- GI Bleeding (upper and lower GI bleeding)
GI Pathophysiology Mechanisms
- Stenosis (narrowing or stricture of an area)
- Regurgitation or insufficiency (backflow or pass-through when it should not occur)
- Abnormalities of Movement (too fast or too slow, think neurological)
- Inflammation/Trauma (can affect absorption, secretion, and bleeding)
Esophagus
- Connects pharynx to stomach
- Secrets some mucous, but no absorption occurs here
- Job: conduit for food, mechanical digestion
- Anatomically indistinct but physiologically demonstrable upper and lower esophageal sphincters
- Mechanisms of pathology:
- Stenosis (e.g., esophageal stricture, esophageal achalasia, T-E Fistula)
- Regurgitation or insufficiency (e.g., GERD, esophageal dysmotility)
- Abnormalities of Movement (e.g., esophageal dysmotility)
- Inflammation/Trauma (e.g., esophagitis, Barrett's Esophagus, Malory-Weiss tear)
Stomach
- Normal gastric secretory epithelium:
- Cardia (mucous-secreting cells)
- Fundus (acid-producing parietal cells, pepsin-producing chief cells)
- Pylorus (hormone production, e.g., gastrin)
- Gastric glands:
- Mucous cells (mucus production)
- Parietal cells (HCl production)
- Chief cells (pepsin production)
- Enteroendocrine cells (gastrin production)
- Mechanisms of pathology:
- Stenosis (e.g., pyloric stenosis)
- Regurgitation or insufficiency (e.g., GERD)
- Abnormalities of Movement (e.g., gastroparesis)
- Inflammation (e.g., gastritis, PUD)
Pyloric Obstruction/Stenosis
- Blocking or narrowing of the opening between the stomach and duodenum
- Can be acquired (GOO) or congenital (pyloric stenosis)
- Clinical manifestations:
- Epigastric pain and fullness
- Nausea
- Vomiting
- Malnutrition and dehydration
- Treatment:
- Gastric drainage (NG Tube)
- IV fluid and electrolytes
- Proton pump inhibitors or H2 blockers
- Surgery or stenting
Intestines
- Duodenum:
- Superior, Descending, Horizontal, and Ascending segments
- Site of delivery for stomach (L1)
- Acidic chyme must be neutralized here
- Site of delivery for pancreas, liver, and gallbladder
- Anatomic features:
- Shortest segment of the small intestine
- Starts at the pyloric sphincter and ends at the Ligament of Treitz
- Almost completely retroperitoneal
- Its segments:
- Superior: releases hormonal triggers for the gallbladder and pancreas
- Descending: pancreatic duct and common bile duct empty here
- Horizontal: digestion occurs here
- Ascending: continued digestion
Pancreas
- Gland with both exocrine and endocrine functions
- Retroperitoneal, arises from the wall of the duodenum
- Parts:
- Head
- Neck
- Body
- Tail
- The Pancreatic Ducts:
- Main pancreatic duct runs the entire length of the pancreas
- Empties its exocrine products at the Ampulla of Vater
- A portion of the head of the pancreas usually drains via a different duct (the accessory pancreatic duct) at the Ampulla of Santorini
Pancreatic Juice
- Secretion of pancreatic enzymes in a clear alkaline medium
- Enzymes are produced by the exocrine cells of the pancreas
- Alkaline mucousy liquid from the pancreatic ductal cells
- Flows to the duodenum via the pancreatic duct system
- Enzymes typically are released in inactive form and are activated by membrane-bound activators in the duodenum### Anatomy of the Gallbladder
- The gallbladder has three layers: simple columnar epithelium, muscularis externa, and adventitia.
- The muscularis externa layer is responsible for gallbladder contractions.
- The adventitia layer holds the gallbladder in place.
The Normal Biliary Tree
- Bile exits the liver via the left and right hepatic ducts.
- Bile can travel into the gallbladder via the cystic duct.
- Bile then leaves the gallbladder via the cystic duct and enters the common bile duct.
- There is only one way into and out of the gallbladder.
- The sphincter of Oddi is used by both the gallbladder and pancreas to enter the duodenum.
Gallbladder Problems
- Common problems include duct blockage, inflammation, and infection.
- Duct blockage can lead to gallstone pancreatitis, gallstone liver inflammation, and an increased risk of liver and pancreatic cancer.
- Symptoms after a cholecystectomy (gallbladder removal) may include fatty stools, poor tolerance of high-fat meals, dyspepsia, and nausea/vomiting.
Cholelithiasis (Gallstones)
- Gallstones are crystallized or solidified stones of gallbladder content.
- They are typically made of bile salts, cholesterol, and other substances.
- Cholesterol gallstones are yellow-gold in color, while pigment gallstones are darker.
- The pathogenesis of cholesterol gallstones involves either more cholesterol in bile than can be dissolved or bile in stasis for longer than normal.
- "Gallbladder sludge" is a risk factor for gallstones, and decreased gallbladder motility can increase the risk of gallstones.
- Estrogen increases the cholesterol composition of bile and decreases gallbladder motility, which is why pregnancy increases the incidence of gallstones.
Malabsorption Syndromes
- Malabsorption is a problem with the mucosa's ability to absorb nutrients into the bloodstream.
- Diseases that interfere with nutrient absorption, such as Crohn's disease and ulcerative colitis, can cause malabsorption.
- Maldigestion is a problem with the processes that get nutrients digested down to the monomer level, often due to an enzyme issue.
- Pancreatic insufficiency can cause maldigestion, particularly fat maldigestion, which can lead to steatorrhea and weight loss.
- Lactose intolerance occurs when the lactase enzyme ceases to be produced, leading to the inability to break down lactose into glucose and galactose.
- Bile salt deficiency can cause malabsorption, particularly of lipids, and can lead to steatorrhea, diarrhea, and a loss of fat-soluble vitamins.
Inflammatory Bowel Disease
- Inflammatory bowel disease is a chronic, relapsing-recurring bowel inflammation of unknown origin.
- The two main types are ulcerative colitis and Crohn's disease.
- Ulcerative colitis causes ulceration of the colonic mucosa, particularly in the sigmoid colon and rectum, and is characterized by continuous lesions with no skipped lesions.
- Crohn's disease causes granulomatous inflammation of the GI tract, which can affect any part of the digestive tract, and is characterized by skip lesions and a "cobblestone" appearance.
Mechanical Bowel Obstruction
- Mechanical bowel obstruction occurs when there is a blockage in the small or large bowel, preventing contents from passing "downstream".
- Risk factors include prior surgery, diseases causing gut inflammation or stricture, volvulus, and intussusception.
- Symptoms include abdominal pain, nausea, and vomiting, and can lead to peritonitis and bowel perforation.
Constipation
- Constipation is defined as infrequent or difficult defecation, with fewer than three bowel movements per week.
- Clinical definitions include straining with defecation, lumpy or hard stools, sensation of incomplete emptying, and manual maneuvers to facilitate stool evacuation.
- Pathophysiology involves transit times and muscular function, with normal transit (functional) constipation, slow-transit constipation, and pelvic floor dysfunction.
- Treatments include diet, exercise, bowel retraining, enemas, and biofeedback.
Diarrhea
- Diarrhea is defined as increased frequency of bowel movements, with three or more per day.
- Types of diarrhea include osmotic, secretory, and inflammatory diarrhea.
- Treatment depends on the physiologic type of diarrhea present.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.