Podcast
Questions and Answers
Which of the following is the primary function of chief cells in the stomach?
Which of the following is the primary function of chief cells in the stomach?
- Producing the hormone gastrin
- Creating and releasing pepsinogen (correct)
- Encouraging the production of intrinsic factor
- Secreting hydrochloric acid
How does hydrochloric acid contribute to digestion in the stomach?
How does hydrochloric acid contribute to digestion in the stomach?
- By converting pepsinogen into pepsin (correct)
- By directly breaking down carbohydrates
- By increasing the absorption of fats
- By neutralizing stomach acid
What is the primary role of parietal cells in the stomach?
What is the primary role of parietal cells in the stomach?
- Secretion of mucus to protect the stomach lining
- Secretion of gastric acid (correct)
- Production of gastrin to stimulate stomach motility
- Absorption of nutrients
How does histamine contribute to the production of hydrochloric acid in the stomach?
How does histamine contribute to the production of hydrochloric acid in the stomach?
What is the function of the mucus-bicarbonate barrier in the stomach?
What is the function of the mucus-bicarbonate barrier in the stomach?
Medication absorption in the GI tract is most affected by which factor?
Medication absorption in the GI tract is most affected by which factor?
Which of the following factors contributes to the development of peptic ulcer disease (PUD)?
Which of the following factors contributes to the development of peptic ulcer disease (PUD)?
A patient with a history of NSAID use is diagnosed with a peptic ulcer. Where are ulcers caused by NSAIDs typically located?
A patient with a history of NSAID use is diagnosed with a peptic ulcer. Where are ulcers caused by NSAIDs typically located?
Which of the following lifestyle factors is most likely to exacerbate gastroesophageal reflux disease (GERD)?
Which of the following lifestyle factors is most likely to exacerbate gastroesophageal reflux disease (GERD)?
If a patient with GERD reports experiencing dysphagia, what does this symptom indicate?
If a patient with GERD reports experiencing dysphagia, what does this symptom indicate?
A patient is prescribed omeprazole for the long-term management of GERD. What potential nutritional deficiency should the healthcare provider monitor?
A patient is prescribed omeprazole for the long-term management of GERD. What potential nutritional deficiency should the healthcare provider monitor?
How does omeprazole reduce gastric acid secretion?
How does omeprazole reduce gastric acid secretion?
A patient taking omeprazole reports frequent headaches and diarrhea. How should the healthcare provider respond?
A patient taking omeprazole reports frequent headaches and diarrhea. How should the healthcare provider respond?
A patient is prescribed famotidine for GERD. What is the mechanism of action of this medication?
A patient is prescribed famotidine for GERD. What is the mechanism of action of this medication?
What advice should be given to a patient taking famotidine and antacids concurrently?
What advice should be given to a patient taking famotidine and antacids concurrently?
A patient on famotidine is also a smoker. How does smoking affect the effectiveness of famotidine?
A patient on famotidine is also a smoker. How does smoking affect the effectiveness of famotidine?
What is the primary action of antacids in treating hyperacidity?
What is the primary action of antacids in treating hyperacidity?
Which side effect is most commonly associated with the use of aluminum hydroxide antacids?
Which side effect is most commonly associated with the use of aluminum hydroxide antacids?
What is a key consideration when administering antacids to patients taking other medications?
What is a key consideration when administering antacids to patients taking other medications?
What is the primary mechanism of action of bismuth compounds like Pepto-Bismol?
What is the primary mechanism of action of bismuth compounds like Pepto-Bismol?
Which of these instructions is most important to include in the teaching for a patient who is newly prescribed bismuth subsalicylate?
Which of these instructions is most important to include in the teaching for a patient who is newly prescribed bismuth subsalicylate?
What drug requires caution to use with ASA(aspirin), cold medication?
What drug requires caution to use with ASA(aspirin), cold medication?
What is the primary goal of using multiple medications to treat Helicobacter pylori?
What is the primary goal of using multiple medications to treat Helicobacter pylori?
A patient is prescribed sucralfate for the treatment of a duodenal ulcer. How does sucralfate work?
A patient is prescribed sucralfate for the treatment of a duodenal ulcer. How does sucralfate work?
A patient taking sucralfate is also prescribed an antacid. What is a potential concern with this combination?
A patient taking sucralfate is also prescribed an antacid. What is a potential concern with this combination?
Which instruction is most important to provide to a patient starting sucralfate for ulcer treatment?
Which instruction is most important to provide to a patient starting sucralfate for ulcer treatment?
Non-pharmacological treatments for nausea include which of the following?
Non-pharmacological treatments for nausea include which of the following?
What is the primary mechanism of action of ondansetron in treating nausea and vomiting?
What is the primary mechanism of action of ondansetron in treating nausea and vomiting?
Scopolamine is an example of what kind of medication?
Scopolamine is an example of what kind of medication?
A patient is prescribed meclizine for vertigo. How does this medication work?
A patient is prescribed meclizine for vertigo. How does this medication work?
Dronabinol is an example of what kind of medication?
Dronabinol is an example of what kind of medication?
What instruction is crucial for a patient using scopolamine patches for motion sickness?
What instruction is crucial for a patient using scopolamine patches for motion sickness?
Which factor should the healthcare provider consider when administering dronabinol to a patient?
Which factor should the healthcare provider consider when administering dronabinol to a patient?
The nurse knows the patient is to receive oral ondansetron. The tablet can be administered by which route(s)?
The nurse knows the patient is to receive oral ondansetron. The tablet can be administered by which route(s)?
When should a patient taking famotidine make lifestyle changes?
When should a patient taking famotidine make lifestyle changes?
What should be monitored for patients who are taking Bismuth for diarrhea accompanied by fever?
What should be monitored for patients who are taking Bismuth for diarrhea accompanied by fever?
Flashcards
Mouth
Mouth
The breakdown of food begins here
Esophagus
Esophagus
Connects the mouth to the stomach
Stomach
Stomach
It is where food is churned and digestion begins
Small intestine
Small intestine
Signup and view all the flashcards
Large intestine
Large intestine
Signup and view all the flashcards
Chief cells
Chief cells
Signup and view all the flashcards
Pepsin
Pepsin
Signup and view all the flashcards
Parietal cells
Parietal cells
Signup and view all the flashcards
Hydrochloric acid
Hydrochloric acid
Signup and view all the flashcards
Gastrin
Gastrin
Signup and view all the flashcards
Mucus-bicarbonate
Mucus-bicarbonate
Signup and view all the flashcards
Small intestine
Small intestine
Signup and view all the flashcards
Large intestine
Large intestine
Signup and view all the flashcards
Peptic ulcer disease (PUD)
Peptic ulcer disease (PUD)
Signup and view all the flashcards
GERD
GERD
Signup and view all the flashcards
Medication management goals
Medication management goals
Signup and view all the flashcards
Proton pump inhibitors
Proton pump inhibitors
Signup and view all the flashcards
H2-receptor antagonists
H2-receptor antagonists
Signup and view all the flashcards
Antacids
Antacids
Signup and view all the flashcards
Aluminum hydroxide
Aluminum hydroxide
Signup and view all the flashcards
Magnesium hydroxide
Magnesium hydroxide
Signup and view all the flashcards
Calcium carbonate
Calcium carbonate
Signup and view all the flashcards
Sodium bicarbonate
Sodium bicarbonate
Signup and view all the flashcards
Antacids Considerations
Antacids Considerations
Signup and view all the flashcards
Bismuth compounds
Bismuth compounds
Signup and view all the flashcards
Anti-infectives
Anti-infectives
Signup and view all the flashcards
Sucralfate
Sucralfate
Signup and view all the flashcards
Ondansetron
Ondansetron
Signup and view all the flashcards
Meclizine
Meclizine
Signup and view all the flashcards
Scopolamine
Scopolamine
Signup and view all the flashcards
Study Notes
- Nutrition is covered in Unit 8.
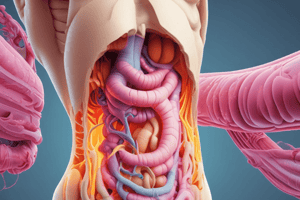
Anatomy and Physiology of the GI System
- The GI system includes the mouth, esophagus, stomach, small intestine, and large intestine.
Stomach Anatomy and Physiology
- Chief cells in the stomach create and release pepsinogen.
- Stomach acid converts pepsinogen into pepsin, a digestive enzyme.
- Pepsin breaks down proteins in food.
- Parietal cells are responsible for gastric acid (hydrochloric acid) secretion.
- Gastric acid aids in food breakdown, kills harmful microorganisms, and activates pepsinogen.
- Parietal cells encourage the production of intrinsic factor (IF), a glycoprotein.
- Intrinsic factor is vital for the absorption of Vitamin B12.
- Enteroendocrine cells produce/secrete the hormone gastrin.
- Gastrin stimulates gastric motility.
- Gastrin secretes histamine, which binds to parietal cells and creates hydrochloric acid.
- The pH of the stomach is 1.5 – 3.5, indicating an acidic environment.
- The mucus-bicarbonate barrier protects the stomach by neutralizing its pH.
- The small intestine is the primary absorption site of medication.
- The large intestine is the primary absorption site of water.
- Medication absorption is affected by the speed at which it goes through the GI tract.
Peptic Ulcer Disease (PUD)
- PUD involves an imbalance of protective factors (mucous & bicarbonate) versus aggravating factors (pepsin and gastric acid).
- PUD may cause bleeding, perforation, penetration, or GI obstruction.
- Risk factors for PUD include family history, smoking, caffeine use, stress, Zollinger-Ellison Syndrome, H. pylori, and certain medications (NSAIDs, steroids).
- Most peptic ulcers found in the stomach are caused by NSAID use, due to inhibiting prostaglandins.
- Duodenal peptic ulcers are usually caused by H-pylori.
Gastroesophageal Reflux Disease (GERD)
- Stomach acids enter the esophagus due to a relaxed lower esophageal sphincter.
- Risk factors for GERD include caffeine, alcohol, acidic foods, carbonation, pregnancy, obesity, smoking, nitrates, benzodiazepines, anticholinergics, beta-blockers, NSAIDs, steroids, TCA's, opioids, levodopa, bisphosphonates, estrogen, and progesterone.
- Symptoms of GERD include heartburn, dyspepsia, dysphagia, cough, sore throat, hoarseness, and nasal congestion.
PUD and GERD Medications
- Goals of medication management for PUD and GERD include relief of symptoms, promoting healing, preventing complications, and preventing reoccurrence.
- Proton pump inhibitors (PPIs) include omeprazole, esomeprazole, lansoprazole, and pantoprazole.
- H2-receptor antagonists (H2 blockers) include famotidine, cimetidine, and nizatidine.
- Antacids include sodium, calcium, magnesium, aluminum, and bicarbonate.
- H. pylori is treated with antibiotics, PPIs, and bismuth.
- Miscellaneous medications include sucralfate and bismuth compounds.
Omeprazole
- Omeprazole is a PPI that reduces acid secretion by irreversibly binding to the proton pump.
- Omeprazole can be administered orally or enterally, and has a delayed-release formulation.
- Omeprazole treats heartburn and prevents PUD in patients taking NSAIDs.
- Omeprazole is used in treating H. pylori.
- Contraindications/cautions include GI bleed and not being recommended in children < 1 year old.
- Potential side effects or adverse reactions include headache and nausea/diarrhea.
- Potential interactions include decreased bioavailability of meds that need an acidic environment for absorption (minerals).
- Mineral deficiencies can occur with long-term PPI use.
- Nursing consideration includes monitoring B12 and LFTs with prolonged use, and monitoring for therapeutic effects.
- Omeprazole has a short half-life, and a longer duration of action (new cells have to be produced).
- Patients should report severe diarrhea and GI bleeding signs/symptoms.
- The omeprazole regimen is 4-8 weeks.
- Decreasing the acidic environment may allow more microorganisms which can lead to diarrhea (c-diff).
- Omeprazole is generally dispensed as extended-release tablets so it can be absorbed in the small intestine.
- It should be taken 20 - 30 minutes before the first meal of the day. -Monitor for effectiveness.
Famotidine (Pepcid)
- Famotidine is an H2 Receptor Antagonist.
- The MOA is that it blocks acid production by blocking H2 receptors on parietal cells.
- It blocks daytime, nighttime, fasting, and food stimulated secretions.
- Is administered PO/enteral, IV.
- Expected therapeutic use include the treatment of PUD, GERD, and stress ulcers
- Contraindications/cautions include severe renal or liver disease
- Potential side effects or adverse reactions include headache, GI (constipation, diarrhea, abdominal pain), B12 deficiency (long term use), thrombocytopenia
- Potentional side effect, decreased absorptions with antacids, smoking decreases effectiveness.
- Monitoring consideration include GI bleeding and checking monitor CBC
- Take with food or liquid, recommend to takes at bedtime, lifestyle changes, monitor for Vit B12, Don't take with antacids and avoid NSAIDS
- Relief may take several days as is safe to give to children or infants
Antacids
- These Alkaline substances that neutralize pH of hydrochloric acid in stomach and reduce the digestive action of pepsin
- Treats pain associated with hyperacidity in PUD, GERD, heartburn, and indigestion
- Action results in increased stomach PH to 3.5
- Aluminum Hydroxide
- Antacid (aka-AlternaGEL)
- Combines with gastric acid to produce aluminum chloride and water, which raises the pH of the stomach contents and inactivates pepsin. Side Effects/AE: constipation, nausea, obstruction/impaction hypophosphatemia, as it is Minimally absorbed and Frequently causes constipation.
- Often combined with magnesium hydroxide to counteract the constipation Magnesium Hydroxide:
- Milk of Magnesia
- Neutralizes stomach acid and inactivates pepsin. Reduces - Reduces symptoms of heartburn.
- AE diarrhea, nausea, vomiting, cramping and Hypermagnesemia. High doses of magnesium-containing antacids can cause symptoms of hypermagnesemia (fatigue, hypotension, and dysrhythmias) Acts as a laxative when it reaches the large intestine Calcium Carbonate:
- Antacid (aka-TUMS, Mylanta
- action neutralizes stomach acid and inactivates pepsin. Reduce symptoms of heartburn, as well as used for eplacement therapy
- SE constipation, flatulence, impaction and hypercalcemia, kidney failure at very high dose
- observe for elevated s/s s of hypercalcemia: HA, urinary frequency, anorexia, nausea, fatigue.
Sodium Bicarbonate:
- Antacid (aka-Alka seltzer).
- Action neutralizes gastric acid and inactivates pepsin.
- Side Effects/AE: abdominal distention, belching, edema, hypernatremia.
- is Not suitable for patients on a sodium-restricted diet or those with HTN, heart failure, or CKD due to the promotion of fluid retention.
- Administered: PO/enteral
- Possible Rebound acidity after they are discontinued
- Antacid effects change in electrolytes
- These will affect the solubility of other medications and change the absorption rate, that depending on the stomach PH for absorption at least and hour or two before medication
- These can improve medications that can improve the acidity of
Bismuth Compounds (Pepto-Bismol)
- Action works as Direct mucosal protective agent that acts as agent against, motility issues and has agent and an anti-inflammatory.
- PO/enteral administrations
- Therapeutic effects include Prophylaxis and treatment of diarrhea, relieve indigestion and H.pylori contraindications or cautions is Allergy to ASA (metabolized to salicylate) is a issue for under age 3. -SE darkening of stool and tongue when, Metallic taste and increased
- May increase aspirin levels as well as May decrease absorption of other medications. Nursing considerations when giving is that Nurse should Monitor bowel function and when it has not been fully assessed and Used when it has to combined with other cold medication.
HELICOBACTER PYLORI AGENTS
- anti-infectives used.
- (amoxicillin, metronidazole, clarithromycin, tetracycline) Antacids used for H. Pylori (and bismuth) for Proton Pump Inhibitors used for it as well (omeprazole)
Treatment for Sucralfate (Carafate)
- Drug class Miscellaneous drug: Pepsin inhibitor (mucosal protective drug)
- action reacts to form A thick to create adhesions to gastic.
- Given PO/enteral.
- Effect : ulcer will be the effect.
- side effects are rare effects for
- PO administered Interactions
- Decreases the absorption of some medications.
- decreases and causes the effectiveness (it needs acid to work).
- Needs gastric to prevent bezoar build to get treatment
Sucralfate: Nursing consideration, etc
- PO Administered should be done a empty stomach.
- Crush tab is a no: tablets are the best way to instruct continue the ordered of 4-8 for healing
- Give water and to exercise for constipation
- Give other meds 2 hours before or after sucralfate
Treatment of Nausea and Vomiting
- Controlled in brain in as CTZ that will become "vomiting center."
- treatments include , Ginger , banana and Acupuncture to help promote hydration Common treatments for the disease include ondansentrons for these issues.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.